
1
Vanderbilt University, Nashville, Tennes-
see;
2
New York University Medical Center,
Hospital for Joint Diseases, New York,
New York;
3
Drexel University College of
Medicine, Philadelphia, Pennsylvania,
USA.
Supported in part by grants from the
A rthritis Foundation, the Jack C. Massey
Foundation and Abbott Immunology.
T h e o d o re Pincus, MD; Yusuf Yazici, MD;
Martin Bergman, MD.
Please address correspondence to:
Theodore Pincus, MD, Professor of
Medicine, Division of Rheumatology and
Immunology, Vanderbilt University School
of Medicine, 203 Oxford House, Box 5,
Nashville, TN 37232-4500, USA.
E-mail: [email protected]
Clin Exp Rheumatol 2005; 23 (Suppl. 39):
S19-S28.
© Copyright CLINICALAND EXPERIMENTAL
RHEUMATOLOGY 2005.
Key words: MDHAQ, HAQ,
activities of daily living.
ABSTRACT
The HAQ has become the pre-eminent
patient questionnaire used in rheuma -
t o l o g y. It is easily completed by patients,
but not easily reviewed and scored in
s t a n d a rd clinical care and has some
minor psychometric limitations, as do
all questionnaires. Modifications of the
HAQ been made to facilitate use in
standard care, particularly to include
8-10 activities of daily living, along
with scores for pain and global status
and other information on one side of
one page for rapid review by the clini -
cian. A patient questionnaire for stan -
dard care should be limited to 2 sides
of 1 page, in a format amenable to
“eyeball” review by the clinician in 5
seconds or less. It can be scored for -
mally in 15-20 seconds or less, and is
useful in patients with all rh e u m a t i c
diseases.
The current version of a multi-dimen -
sional HAQ (MDHAQ) includes scor -
ing templates on the questionnaire to
allow formal scoring in less than 15 se -
conds by a rheumatologist or an assis -
tant, for possible entry onto a paper
and/or computerized flow sheet. Vari -
ous versions of the MDHAQ may also
include a "constant" region of physical
function, pain and patient global sta -
tus, and "variable" regions of fatigue,
morning stiffness, psychological dis -
tress, change in status, a review of sys -
tems, a rheumatoid arthritis disease ac -
tivity self-report joint count (RADAI),
review of recent health events, and re -
view of medications. The MDHAQ can
be used in the infrastructure of rheu -
matology care to include quantitative
data in standard care of all patients
with all rheumatic diseases.
Introduction
Over the last 25 years, since its land-
mark publication in April 1980, the
Health Assessment Questionnaire
(HAQ) (1) has become the pre-eminent
patient questionnaire in rheumatology.
The HAQ queries 20 activities of daily
living (ADL) (Table I) for which the
patient is asked to respond in 4 cate-
gories as to whether he or she can per-
form the activity “without any difficul-
ty” (= 0), “with some difficulty” (= 1),
“with much difficulty” (= 2), and
“unable to do” (= 3) (2). The 20 activi-
ties are classified into 8 categories of 2
or 3 each. The HAQ also queries the
use of 16 aids and devices. A score for
each of the 8 categories is based on the
maximum score for any of the 2 or 3
activities in the category, with an
increase in the score by 1 for any cate-
gory in which patients use an aid or
device. The total score is the mean of
the scores for the 8 categories (1). The
HAQ is discussed in detail in this Sup-
plement by its developer, James Fries
with Bonnie Bruce (3).
Some limitations of the HAQ
The HAQ has proven a major advance
in rheumatology clinical research.
However, as is the case with all mea-
surement methods, certain limitations
are seen, which are not of major conse-
quence but may detract from its psy-
chometric validity (Table I). A HAQ
score may be increased artefactually by
a rheumatologist recommending a
device to aid a patient’s function; for
example, if a patient responds that she
walks, opens jars, or performs another
activity “with some difficulty”, and is
given a cane, jar opener, or other de-
vice, but continues to respond “with
some difficulty”, the score will be
increased from 1 to 2, even though the
p a t i e n t ’s physical function may be
improved.
Different activities may determine the
HAQ scores on different completions,
as only 1 of 2 or 3 activities within each
category determines the score for the
category. The categories of the HAQ do
not necessarily group related activities
S-19
Development of a multi-dimensional health assessment
questionnaire (MDHAQ) for the infrastructure of standard
clinical care
T. Pincus
1
, Y. Yazici
2
, M. Bergman
3

S-20
Development of the MDHAQ / T. Pincus et al.
effectively; “stand up from a straight
chair” in the category of “arising” and
“get on and off the toilet” in the catego-
ry of “hygiene” are correlated at higher
levels of significance with one another
than with the other activities within the
categories of “arising” and “hygiene
(4). A patient may hypothetically im-
prove on 1 to 12 of the 20 activities on
the HAQ, but show no change in HAQ
score.
Floor effects are seen, namely that
patients may have normal HAQ scores,
but nonetheless feel that there exist
functional limitations. A change in
score of a given interval, say from 0.25
to 0.5, may not represent a similar
change as a change from 0.25 to 1.5
(5). As noted, none of these matters
limit the HAQ severely in the docu-
mentation and monitoring of status in
clinical trials, and in predicting work
disability and mortality in observation-
al clinical research, as the HAQ or a
derivative – rather than a joint count,
laboratory test or radiograph – is the
best predictor in rheumatoid arthritis
(RA) of functional status (6, 7), work
disability (8-10), costs (11), joint
replacement surgery (12) and prema-
ture death (6, 13-19).
The HAQ is generally easily completed
by most patients in 5-10 minutes. How-
ever, pragmatic considerations may li-
mit use of the HAQ in standard clinical
care, as few clinicians – with some
notable exceptions such as Dr. Freder-
ick Wolfe (20) – use the HAQ routine-
l y. Some HAQ activities, such as
“shampoo your hair” and “do chores
such as vacuuming or yard work” are
not performed by some patients, caus-
ing some interruption in completion by
some patients. Since the HAQ involves
2 sides of 1 page, it cannot be quickly
reviewed (“eyeballed”) by a clinician
to get a simple overview of patient sta-
tus. The scoring system is somewhat
complex, generally requiring at least a
minute. The HAQ does not include
data concerning psychological distress,
fatigue, change in status, morning stiff-
ness, or other constructs which some
clinicians may wish to monitor in stan-
dard care.
These considerations have led to efforts
to develop simpler patient question-
naires for use in standard clinical care,
in a more easily scored format, which
can be scanned (“eyeballed”) by a clin-
ician in 5 seconds or less, scored in less
than 10-20 seconds, and that provide
additional information concerning psy-
Table I. Items included on the HAQ, 8 ADLMHAQ, 14 ADLMDHAQ, 10 ADLMDHAQ
and HAQII. (The codes of the items are the same as used in other tables).
HAQ 8 ADL 14 ADL 10 ADL HAQII
MHAQ MDHAQ MDHAQ
(1) (4) (24) (2) (5)
DRESSING & GROOMING:
Dress yourself, including tying shoelaces
and doing buttons ? 1a a a a
Shampoo your hair ? 1b - - -
ARISING:
Stand up from a straight chair ? 2a - - - √
Get in and out of bed ? 2b b b b
EATING:
Cut your meat ? 3a - - -
Lift a full cup or glass to your mouth ? 3b c c c
Open a new milk carton ? 3c - - -
WALKING:
Walk outdoors on flat ground ? 4a d d d √
Climb up 5 steps ? 4b - - -
Walk 2 miles or 3 kilometers ? - - i i
HYGIENE:
Wash and dry your entire body ? 5a e e e
Take a tub bath ? 5b - - -
Get on and off the toilet ? 5c - - - √
REACH:
Reach and get down a 5 pound object
from above your head ? 6a - - - √
Bend down to pick up clothing from the floor ? 6b f f f
GRIP:
Open car doors ? 7a - - - √
Open previously opened jars ? 7b - - -
Turn regular faucets on and off ? 7c g g g
OTHER ACTIVITIES:
Run errands and shop ? 8a - k -
Get in and out of a car, bus, train, or airplane ? 8b h h h
Do chores such as vacuuming or yard work ? 8c - - -
Participate in sports and games as you would
like ? - - j j
Climb up a flight of stairs ? - - l -
Run or jog two miles ? - - m -
Drive a car 5 miles from your home ? - - n -
PSYCHOLOGICALSTATUS:
Get a good night’s sleep ? - - o o
Deal with the usual stresses of daily life ? - - p p
Deal with feelings of anxiety or being
nervous ? - - q -
Deal with feelings of depression of feeling
blue ? - - r -
HAQII ITEMS NOTLISTED ABOVE
Go up two or more flights of stairs ? √
Lift heavy objects ? √
Move heavy objects ? √
Wait in line for 15 minutes ? √
Do outside work (such as yard work) ? √
Source: Reference (2)

chological status, fatigue, change in sta-
tus, morning stiffness, review of systems,
medications used, all on 2 sides of 1
page. The modified HAQ (MHAQ) and
multi-dimensional HAQ (MDHAQ)
were developed to meet these goals.
Development of a modified HAQ
(MHAQ)
A modified HAQ (MHAQ) was des-
cribed in 1983 (4), which includes 8
activities of daily living, 1 from each
category of the HAQ (Table I), with no
aids and devices, for rapid review by a
clinician and scoring in less than half
the time needed for the HAQ. MHAQ
scores are correlated significantly with
HAQ scores (as would be expected for
the same items) (4), and with tradition-
al joint counts, radiographs and labora-
tory indicators of inflammation (21).
The MHAQ appears to be as sensitive
as the HAQ in clinical trials to recog-
nize differences between active and
control treatments (22), and as infor-
mative in longitudinal clinical studies
of morbidity (17), mortality (16, 17)
and work disability (8) in RA. T h e
MHAQ also includes 10 cm visual ana-
log scales for pain and global status, to
assess the 3 patient questionnaire mea-
sures on the ACR Core Data Set (23).
The activities chosen for the MHAQ
were generally the simplest of the 2 or
3 within each HAQ category (Table I),
as the deleted activities were some that
certain patients do not perform, such as
“shampoo your hair”, “vacuuming or
yard work”, or “take a tub bath.”
Therefore, MHAQ scores were system-
atically 0.3–0.4 units lower than HAQ
scores, and “floor effects,” i.e., scores
of 0 in people who had some functional
d i s a b i l i t y, were more common than
seen on the HAQ (24). This problem
became more prominent during the
1990s as the status of patients with RA
improved substantially with the aggres-
sive use of low dose methotrexate and
low dose prednisone (25).
Development of a multi-dimensional
HAQ (MDHAQ)
The lower scores with a greater level of
“floor effects” of the MHAQ compared
to the HAQ was addressed by the addi-
tion of 6 complex activities in a multi-
dimensional HAQ (MDHAQ) (Table I)
(24). The term “multi-dimensional” is
used in recognition that the question-
naire had been further modified over
the years to include not only the queries
of 8-10 activities of daily living, and
visual analog scales for pain and global
status from the ACR Core Data Set (23,
26, 27), but also scores for fatigue, psy-
chological distress, morning stiff n e s s
and change in status on one side of one
page, and review of systems and medi-
cations on the reverse side of the page.
The additional activities reduced the
number of patients with floor effects
from 16% on the HAQ and 30% on the
MHAQ, to less than 3% on the MD-
HAQ.
More recently, a further revision of the
MDHAQ with only 2 of 6 additional
activities, “walk 2 miles or 3 kilo-
meters” and “participate in recreation
and sports as you would like,” has been
reported (Table I) (2). This format fur-
ther advanced ease of scoring, as scores
for 10 activities may be divided by 10
and scored 0-3, as in the HAQ, or divi-
ded by 3 and scored 0-10, so that scores
for functional disability are scored 0-
10, as are scores for pain, global status
and fatigue (2). The prevalence of floor
effects was 10%, but most patients with
a score of “0” were in a clinical remis-
sion status.
The initial report of the MDHAQ
included 4 items to address psycholog-
ical distress, including anxiety, depres-
sion, sleep and dealing with stress (24),
in the patient-friendly HAQ format of 4
response items – “without any difficul-
ty, “with some difficulty,” “with much
difficulty,” “unable to do.” The depres-
sion item was found to be correlated
significantly with the Beck Depression
Inventory and Centers for Epidemio-
logic Studies Depression Inventory
(CES-D), which takes up a page or
more (r > 0.6, p < 0.001). In the revised
MDHAQ (2), scores for psychological
distress were found to be similar with
removal of the “stress” item, and 3
items for anxiety, depression and sleep
have been retained. Each item is scored
on a 0 to 3.3 scale, 0 = with no difficul-
ty, 1.1 = with some difficulty, 2.2 =
with much difficulty, and 3.3 = unable
to do. The total score for this psycho-
logical distress scale is the total of the 3
items, i.e. 0 – 9.9, again giving a total
near 10 as for the other scales.
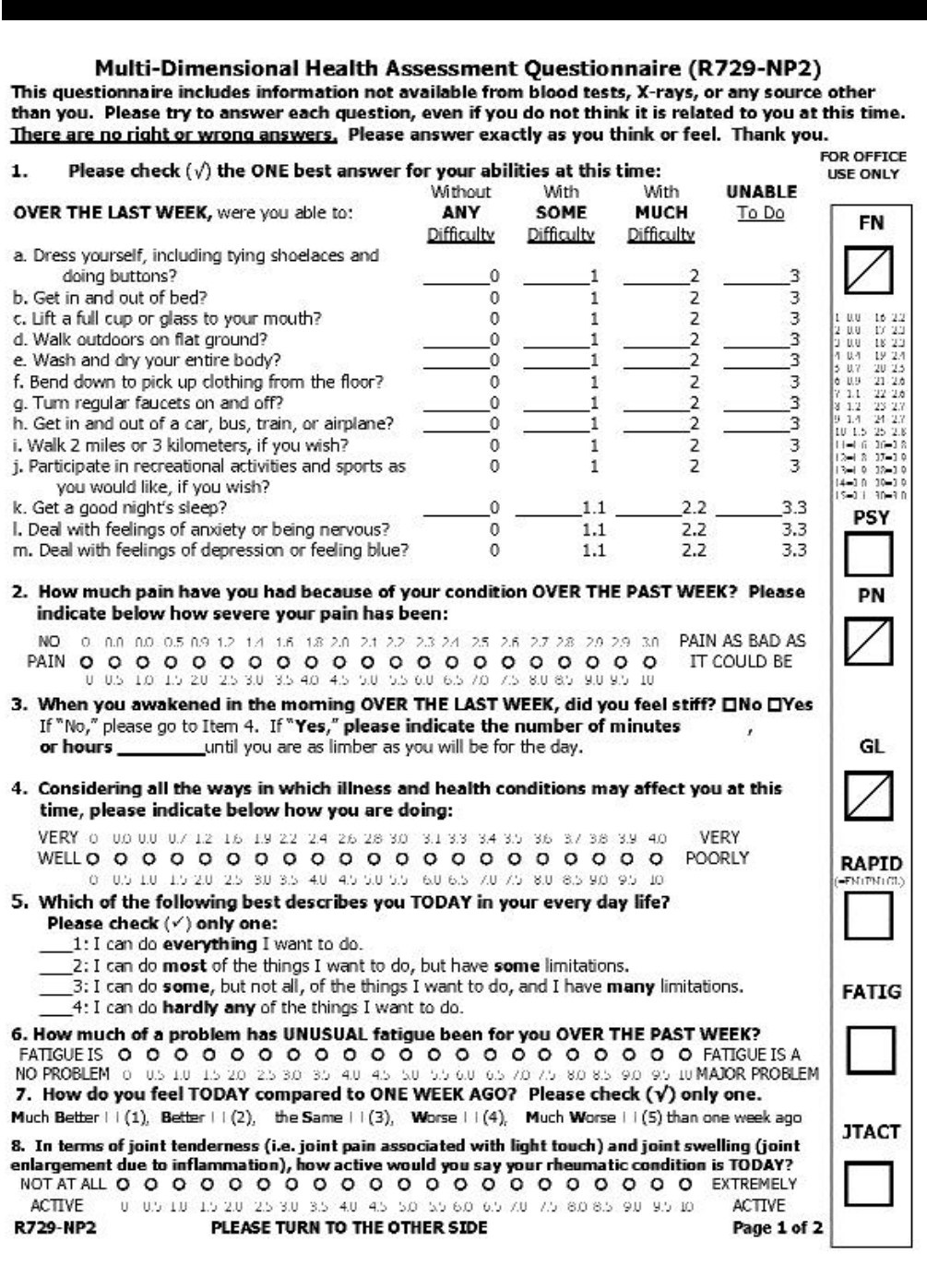
The recently reported MDHAQ (Fig. 1)
includes 7 scores: physical function,
pain, global status, psychological dis-
tress, and fatigue, each of which is
scored 0-10 (or 0-3 for physical func-
tion, if preferred), as well as change in
status and morning stiffness in minutes,
all on 1 side of 1 page which can be
easily scanned in 5 seconds to gain an
overview of a patient’s situation. While
it is pragmatically desirable that the
same questionnaire be completed by
each patient within each clinical set-
ting, it is not necessary that every pa-
tient questionnaire used in every rheu-
matology setting be identical. All ver-
sions of the MDHAQ (available at
website mdhaq.org) include a “con-
stant” region, analogous to immuno-
globulins, of physical function, pain,
and global status, the 3 patient self-
report measures from the ACR Core
Data Set (23), as well as strongly en-
couraged and optional “variable” re-
gions. “Variable” regions regarded as
“strongly encouraged” include scales
for psychological distress, fatigue,
change in status, morning stiffness, and
an RADAI-self-report joint count
(Table II). “Variable” regions regarded
as “optional” include (Table II): a re-
view of systems list of medications
used, recent medical events, demogra-
phic data, and physician assessment of
global status. One of the authors (YY)
includes a physician note on a 1-page
2-sided form.
One example is illustrated in Figures 1
and 2. One side of the page (Fig. 1)
includes 10 activities of daily living, 3
items to assess psychological distress,
S-21
Development of the MDHAQ / T. Pincus et al.
Fig. 1. (next page) A version of the multi-
dimensional health assessment questionnaire
(MDHAQ) designed for use in standard medical
care, which includes scores for physical func-
tion, psychological distress, pain, morning stiff-
ness, global status, self-report functional class,
change in status, fatigue, and disease activity
from the rheumatoid arthritis disease activity in-
dex (RADAI) self-report joint count, on one side
of one page. Scoring templates and space to enter
scores are provided on the questionnaire, as dis-
cussed in the text (translated versions of M D-
HAQ are available in French, German, Italian, Spa-
nish, Danish and Finnish at www. M D H A Q . o rg ) .
S-22
Development of the MDHAQ / T. Pincus et al.

S-23
Development of the MDHAQ / T. Pincus et al.

S-24
Development of the MDHAQ / T. Pincus et al.
visual analog scales (VAS) for pain,
global status, and fatigue, and scores
for change in status and morning stiff-
ness, and on the other side (Fig. 2) a
review of systems, the rheumatoid arth-
ritis disease activity index (RADAI)
self-report joint count (28), recent med-
ical events, and demographic data.
Simple questionnaires such as a 10-
item HAQ II (5, 29) or 12-item ROAD
(30), present reasonable alternatives to
the MDHAQ. Differences in the patient
questionnaire appear acceptable, so
long as the critical “constant” region is
included.
It should be emphasized that there is no
need to involve a computer in any of
these scoring activities, which are easi-
ly accomplished using pencil and paper
in any clinical setting, although a com-
puter database may be desirable. The
acquisition of additional information
on one page concerning psychological
distress, fatigue, morning stiffness, and
change in status, and ease of scoring
may be the advantages of an MDHAQ
compared to the HAQ. A change in
scores for pain, fatigue, global status,
and psychological distress often is at
least as important in clinical care as a
change in the functional disability
score.
Patient questionnaires for clinical
research and for standard clinical
care
As noted, the primary purpose of mod-
ifying the HAQ to develop the MD-
HAQ was to facilitate the application
of patient questionnaires beyond clini-
cal research (31-33) to standard clinical
rheumatology care. Many reasons have
been cited to explain why patient ques-
tionnaires are not included in standard
care. The first may be that data from a
physician and/or high-technology im-
aging and laboratory source are regard-
ed as “objective” clinical information
in the traditional “biomedical model”
paradigm, the basis for most of the spec-
tacular advances in 20
th
century med-
icine. By contrast, data from a patient
are regarded as “subjective” – with the
primary purpose of leading to “objec-
tive,” definitive data. However, no stu-
dy has documented greater significance
for an imaging method or laboratory
test compared to a patient question-
naire in the prognosis or documenta-
tion of important clinical outcomes in
rheumatoid arthritis, such as functional
status (6, 7), work disability (8-10),
costs (11), joint replacement surg e r y
Table II. Three types of components of MDHAQ for standard clinical care: “Constant” -
required, and “variable” - strongly encouraged and optional.
“Constant”- Required “Variable”- Strongly Encouraged Variable – “Optional”
Physical function Psychological distress Review of systems
Pain Fatigue Medications used
Patient global Change in status Recent medical events
Morning stiffness Physician global
RADAI-self-report joint count Physician note on 2-page form
Table III.Patient questionnaires in clinical research and clinical care.
Feature Clinical research Clinical care
Design considerations Complete, long Patient friendly, can be completed
by patient within 5–10 min
Effect on patient visit Adds time, interferes with flow Saves time for MD and patient
Type of questionnaire May be “generic”, “disease specific”, Applicable to patients with all
other research goals rheumatic diseases
Scoring Complex, requires computer Simple, may “eyeball” results; scored
in < 20 seconds
Goal of data Add to research database Add to clinical care
Focus of analysis Groups of patients in clinical trials Individual patients cared for by
or observational databases individual physicians
Data management Send to data center Review for patient care; may enter
into flow-sheet to compare to previous
visits
Major criteria for use Validity, reliability; assess minimum Document status, medical and
clinically important significant medico-legal rationale for aggressive
difference (MCID) therapies
Disposition of Enter into computer Enter into flow sheet in medical
questionnaire record
Table IV. A practical system for routine assessment of functional status, pain, global status,
fatigue and psychological distress.
1. Patient is given 2-page questionnaire by receptionist; it generally is most feasible to include each
patient with each diagnosis at each visit in the infrastructure of clinical care.
2. Patient completes simple questionnaire with minimum interruption of patient flow, usually in
waiting room; help is needed by 5-25% of patients.
3. Nurse or staff member may help patients when needed, review questionnaire for completeness,
and may score questionnaire.
4. Physician does as little as possible, but should scan (“eyeball”) contents - may score question-
naire and/or perform formal joint count.
5. Office staff may enter data unto flow sheet with laboratory and medication data.
Fig. 2. ( p revious page) Reverse side of the
MDHAQ, which includes a review of systems,
the rheumatoid arthritis disease activity index
(RADAI) self-report joint count (28), recent
medical events, and demographic data.

S-25
Development of the MDHAQ / T. Pincus et al.
Fig. 3.A patient seen initially on 5 March 2003, who developed rheumatoid arthritis in a post-partum period with a 3-month old baby, who she could not care
for because of functional disability. All MCP, PIPjoints, wrists and knees were tender and swollen. Her initial scores on 5 March 2003 were 6.3 for function-
al distress, 7.8 for pain, and 9.1 for global status. She was initially begun on prednisone 10 mg/day and methotrexate 15 mg/week. One week later she showed
substantial improvement with her functional status score declining to 2.0, pain to 5.6, and global status to 5.6. However, it was apparent that she had very
aggressive disease, and was begun on etanercept. Over the next 8 months clinical improvement is documented, with declines in the patient’s scores for func-
tional status to 0.67, pain to 0.7, global status to 0.3, as well as other scores. Two years later she continues in near-remission status, albeit with low dose
methotrexate, low-dose prednisone, and etanercept.

(12) or death (6, 13-19). If a laboratory
test for, say, a T-cell marker or cytokine
were available with the robust value of
the HAQ or MHAQ in the prognosis
and monitoring of rheumatoid arthritis,
it would surely be incorporated into
standard rheumatology care by all
rheumatologists.
One important concern that has not re-
ceived much emphasis involves the dif-
ferences between questionnaires de-
signed for clinical research versus
those intended for clinical care (Table
III). The experience of most rheumatol-
ogists with patient questionnaires has
involved lengthy questionnaires in cli-
nical trials and other clinical research,
and many rheumatologists have limited
experience with short questionnaires
adapted for standard clinical care. A
patient questionnaire designed for stan-
dard clinical care may differ consider-
ably from one designed for clinical re-
search (Table III), much as a test for
rheumatoid factor or C-reactive protein
developed in a research laboratory may
be adapted in a simplified form for
standard care.
In clinical research, the primary goal is
to acquire data that is as complete as
might be needed to address the study
questions. Patients and clinicians there-
fore recognize and accept the inconve-
niences of lengthy questionnaires. The
scoring may be quite complex and the
data are not interpreted at the clinical
site; rather they are sent to a data center
for entry into a large common database
(Table III). The clinician does not re-
view the data; indeed, in clinical trials
the clinician is generally expected not
to review the questionnaire data at all.
By contrast, a questionnaire for stan-
dard care must be feasible and practical
( Table III). Requirements for such a
questionnaire include (Table IV) that it
can be completed by a patient within 5-
10 minutes, scanned (“eyeballed”) by a
health professional for a clinical over-
view in less than 5 seconds, and scored
by a health professional within 20-30
seconds, and is amenable to entry onto
a flow sheet to compare with previous
visits within 30 seconds. Further, a
questionnaire for standard patient care
must be clinically applicable to patients
with all diagnoses (24, 34), and provide
time-saving information to the physi-
cian by enhancing a patient’s capacity
to describe concerns in the limited time
allotted for a clinical encounter. The
MDHAQ meets these requirements.
Use of patient questionnaires in
standard care
A very simple system has been imple-
mented effectively over the last 20
years, which can assure completion of
a questionnaire by almost every patient
at every visit (35) (Table IV). When the
patient registers for the visit, the recep-
tionist asks him or her to complete a
questionnaire – provided on a clip-
board together with a soft pencil or felt-
tip pen – while waiting to see the physi-
cian. The questionnaire should be pre-
sented as an important component of
medical care, contributing to provide
data regarding functional status, pain,
global status, fatigue, and psychologi-
cal status that cannot be obtained in any
other way. A cheerful and enthusiastic
manner is important – the patient loses
interest if the staff projects a general
disdain of questionnaires.
The questionnaire is completed by the
patient before being called into an ex-
amining room. Most patients wait at
least 5-10 minutes before seeing a rheu-
matologist. The questionnaire helps the
patient to focus on problems and sum-
marize the overall evaluation. Most pa-
tients do not need help from a health
care professional, although about 20%
of patients to ask for help from a fami-
ly member or health professional to
complete the questionnaire, which is
willingly provided.
The questionnaire may be reviewed
with a nurse or another member of the
office staff, when the weight or blood
pressure are checked, or when the pa-
tient is placed in an examination room.
This review is not necessary, but may
include the identification and comple-
tion of missing data, medications, pa-
tient inquiries, and scoring of the ques-
tionnaire scales, as described below.
The questionnaire should be scanned
briefly by the physician to review the
patient’s clinical status. Patients have
commented that they have felt unhappy
after completing questionnaires in phy-
sician’s offices if there was no evidence
that the information was reviewed by a
health professional.
Scoring of the MDHAQ
Another relatively neglected matter
involves the scoring of patient ques-
t i o n naires in standard clinical care. Of
course, it is possible to recognize the
extent of functional disability and pain
without a need for formal scoring, just
as a physician can recognize a fever or
tachycardia without formally measur-
ing the patient’s temperature or pulse.
H o w e v e r, formal quantitative informa-
tion enhances the information needed
for care, and formal scores for physical
function, pain and global status may
also improve care.
The MDHAQ has scoring templates
that allow a health professional to for-
merly depict a quantitative number for
each scale within 15 seconds, directly
on the questionnaire. The 10 activities
of daily living can be quickly totaled
without a calculator, computer or any
other device (other than a human
brain); the total is divided by 10 to
reach a 0–3 score, with scores compa-
rable to the HAQ. One can also divide
the score by 3 to derive a 0–10 score,
which will then be similar to scores for
pain and global status. Also included is
a logarithmic scale, which has been
found to be more sensitive than an
arithmetic scale to distinguish active
from control treatment in certain clini-
cal trials (Koch and Pincus, unpub-
lished data).
The visual analog scales for pain and
global status as well as fatigue, are pre-
sented as 21 circles rather than the tra-
ditional 10 cm line, to facilitate scoring
without a ruler. One version of the MD-
HAQ includes an arithmetic scale of
0–10 below the circles, and a logarith-
mic scale above the circles – the rheu-
matologist may choose either format.
The logarithmic scale has a range of 0-
3 for physical function, 0-3 for pain
and 0-4 for global status, for a total
range of 0-10. This score has been
termed the “rheumatology assessment
patient index data” (RAPID), and rep-
resents an index of patient scores with a
range of 0-10 that provides an absolute
score which is as sensitive as the dis-
ease activity score (DAS) in distin-
S-26
Development of the MDHAQ / T. Pincus et al.

S-27
Development of the MDHAQ / T. Pincus et al.
guishing active from control treatment
in certain clinical trials (Koch and Pin-
cus, unpublished data). Although the
format of labeling each circle may
appear quite “busy,” the inclusion of
only a few numbers along the visual
analog scale tends to lead patients to
cluster responses primarily in labeled
circles. Therefore, it appears best to la-
bel each circle or none at all, although
if there are no labels more time is
required to score the scales. Formal
scores can be entered into flowsheets as
illustrated below.
Management of MDHAQ data
using a clinical flowsheet
Many options exist for the management
of questionnaire data, ranging f r o m
simply scanning (“eyeballing”) the
questionnaire to assess patient status, to
formally scoring it, to keeping a flow-
sheet (Table IV, Fig. 3). A flowsheet
may be used to facilitate the recogni-
tion of possible changes in functional
capacity, pain, fatigue, or psychologi-
cal status from previous visits. A flow-
sheet appears very useful in the man-
agement of chronic disease in general,
and many clinicians record medica-
tions, laboratory tests, joint examina-
tion findings, and other data on a flow-
sheet. The one-page flowsheet, which
includes patient questionnaire scores,
laboratory data and drugs, is very use-
ful in standard clinical care.
One example of use of the flowsheet is
presented in Figure 3. This illustrates a
patient who was seen initially on 5
March 2003, who developed rheuma-
toid arthritis in a postpartum period
with a 3-month old baby, which she
could not take care of because of her
functional disability. All MCP, PIP
j o i n t s , wrists and knees were tender and
swollen. Her initial scores on 5 March
2003, were 6.3 for functional distress
7.8 for pain, and 9.1 for global status.
She was initially begun on prednisone
10 mg/day and methotrexate 15 mg/
week. One week later she showed sub-
stantial improvement with her func-
tional status score declining to 2.0, pain
to 5.6, and global status to 5.6. Howev-
er, it was apparent that she had very
aggressive disease, and was begun on
etanercept. Over the next 8 months, her
clinical improvement is documented
with declines of her scores for func-
tional status to 0.67, pain to 0.7, and
global status to 0.3, as well as other
scores. Two years later she continues in
n e a r-remission status, continuing to
take low-dose methotrexate, low-dose
prednisone, and etanercept.
Some principles of questionnaire
use in standard care
Clinicians have expressed concerns
that questionnaires may interfere with
office routine and time management,
with consequent increased costs and
time. However, data from a brief ques-
tionnaire designed for standard care
can provide an important s a v i n g o f
time (after a brief “learning curve,” as
is required with any new activity). In-
formation concerning functional status,
pain, psychological distress, fatigue,
global status, review of systems, and
medications are then known to the phy-
sician at the start of the visit, rather than
when acquiring basic data from the
patient. This facilitates a focus on mat-
ters that require attention, leading to
more efficient and effective clinical care.
The questionnaire contributes to clini-
cal judgement, but all decisions must
be made by the clinician.
Many specialized questionnaires such
as the Short Form 36 (SF36) and dis-
ease-specific questionnaires for anky-
losing spondylitis (36), fibromyalgia
(37) and osteoarthritis (38), are avail-
able for different types of clinical re-
search studies in which their use is un-
questioned. However, it is generally
not feasible to use additional question-
naires in standard clinical care. T h e
MDHAQ can be useful for patients
with any rheumatic disease (24, 34), all
of whom may experience physical dis-
ability, pain, fatigue and psychological
distress.
Many clinicians have suggested that it
would be desirable to select patients to
complete questionnaires on the basis of
specific diagnoses, the interval since
the last questionnaire, the beginning of
new therapy etc. However, schemes
that include only certain patients gener-
ally fail in standard clinical practice. It
is considerably easier for the off i c e
staff to hand a questionnaire to each
patient at each visit. Collection of rou-
tine data from consecutive patients at
each visit may be supplemented by
additional data collection at intervals in
certain subsets of patients, if desired.
For example, all patients of one of the
authors (TP) are invited to complete
questionnaires every 6 months for the
US National Database organized by Dr.
Wolfe (39).
Concluding thoughts
The authors believe that rheumatolo-
gists enhance the lives of their patients
as much as any physician, but improve-
ments in status generally are not docu-
mented quantitatively. The absence of
effective documentation adds a signifi-
cant problem to people with rheumatic
diseases, as the provision of many ser-
vices are limited in the current climate
of cost containment. Documentation of
the effectiveness of rheumatology care
is accomplished most cost-effectively
through the routine distribution of
patient self-report questionnaires in
standard care (35).
There is a general viewpoint that “sci-
ence” involves only high technology
and laboratory activities. However,
research over the last 25 years has doc-
umented that clinical rheumatology can
be a most effective quantitative “sci-
ence.” A self-report questionnaire may
be the only measure to recognize sig-
nificant disease progression over 5-10
years, while joint tenderness, erythro-
cyte sedimentation rate (ESR), global
severity, and morning stiffness may be
unchanged or improved over 5-10 years
(40). These observations suggest that
self-report questionnaires (and radio-
graphs) may be the optimal clinical
measures through which rheumatolo-
gists might document improvement or
prevention of disease progression over
5-10 years.
When data are not collected on any giv-
en day, information is not available to
compare to previous and future visits
or to document the potential value of
patient care. It may be regarded as an
intellectual responsibility of rheuma-
tology health professionals to imple-
ment clinical rheumatology as a quanti-
tative science, which is best accom-
plished using patient questionnaires.

S-28
Development of the MDHAQ / T. Pincus et al.
This practice will help to advance
rheumatology as a specialty to improve
the lives of millions of people with
rheumatic diseases.
References
1. FRIES JF, SPITZ P, KRAINES RG, HOLMAN
H R : Measurement of patient outcome in
arthritis. Arthritis Rheum 1980; 23: 137-45.
2. PINCUS T, SOKKA T, KAUTIAINEN H: Fur-
ther development of a physical function scale
on a multidimensional health assessment
questionnaire for standard care of patients
with rheumatic diseases. J Rheumatol 2005;
32: 1432-9.
3. BRUCE B, FRIES JF: The Health Assessment
Questionnaire (HAQ). Clin Exp Rheumatol
2005; 23 (Suppl. 39): S14-S18.
4. PINCUS T, SUMMEY JA, SORACI SA, JR. ,
WALLSTON KA, HUMMON NP: Assessment
of patient satisfaction in activities of daily
living using a modified Stanford health as-
sessment questionnaire. A rthritis Rheum
1983; 26: 1346-53.
5. WOLFE F, MICHAUD K, PINCUS T: Develop-
ment and validation of the health assessment
questionnaire II: A revised version of the
health assessment questionnaire. A rt h r i t i s
Rheum 2004; 50: 3296-305.
6. PINCUS T, CALLAHAN LF, SALE W G ,
BROOKS AL, PAYNE LE, VAUGHN W K :
Severe functional declines, work disability,
and increased mortality in seventy-five rheu-
matoid arthritis patients studied over nine
years. Arthritis Rheum 1984; 27: 864-72.
7. WOLFE F, CATHEY MA: The assessment and
prediction of functional disability in rheuma-
toid arthritis. J Rheumatol 1991; 18: 1298-
306.
8. C A L L A H A N L F, BLOCH DA, PINCUS T:
Identification of work disability in rheuma-
toid arthritis: Physical, radiographic and lab-
oratory variables do not add explanatory
power to demographic and functional vari-
ables. J Clin Epidemiol 1992; 45: 127-38.
9. WOLFE F, HAWLEY DJ: The longterm out-
comes of rheumatoid arthritis: Work disabili-
ty: A prospective 18 year study of 823 pa-
tients. J Rheumatol 1998; 25: 2108-17.
10. S O K K A T, KAUTIAINEN H, MÖTTÖNEN T,
HANNONEN P:Work disability in rheumatoid
arthritis 10 years after the diagnosis. J
Rheumatol 1999; 26: 1681-5.
11. LUBECK DP, SPITZ PW, FRIES JF, WOLFE F,
MITCHELLDM, ROTH SH:A multicenter stu-
dy of annual health service utilization and
costs in rheumatoid arthritis. Arthritis Rheum
1986; 29: 488-93.
12. W O L F E F, ZWILLICH S H: The long-term
outcomes of rheumatoid arthritis: A 23-year
prospective, longitudinal study of total joint
replacement and its predictors in 1,600 pa-
tients with rheumatoid arthritis. A rt h r i t i s
Rheum 1998; 41: 1072-82.
13. WOLFE F, KLEINHEKSEL SM, CATHEY MA,
HAWLEY DJ, SPITZ PW, FRIES JF: The clini-
cal value of the Stanford health assessment
questionnaire functional disability index in
patients with rheumatoid arthritis. J Rheuma -
tol 1988; 15: 1480-8.
14. LEIGH JP, FRIES JF: Mortality predictors
among 263 patients with rheumatoid arthri-
tis. J Rheumatol 1991; 18: 1307-12.
15. P I N C U S T, BROOKS RH, CALLAHAN LF:
Prediction of long-term mortality in patients
with rheumatoid arthritis according to simple
questionnaire and joint count measures. Ann
Intern Med 1994; 120: 26-34.
16. CALLAHAN LF, CORDRAY DS, WELLS G,
PINCUS T: Formal education and five-year
mortality in rheumatoid arthritis: Mediation
by helplessness scale scores. Arthritis Care
Res 1996; 9: 463-72.
17. CALLAHAN LF, PINCUS T, HUSTON JW, III,
BROOKS RH, NANCE EP, JR, KAYE JJ: Mea-
sures of activity and damage in rheumatoid
arthritis: Depiction of changes and prediction
of mortality over five years. Arthritis Care
Res 1997; 10: 381-94.
18. SÖDERLIN MK, NIEMINEN P, HAKALA M:
Functional status predicts mortality in a com-
munity based rheumatoid arthritis popula-
tion. J Rheumatol 1998; 25:1895-9.
19. S O K K A T, HAKKINEN A, KRISHNAN E,
HANNONEN P: Similar prediction of mortal-
ity by the health assessment questionnaire in
patients with rheumatoid arthritis and the
general population. Ann Rheum Dis 2 0 0 4 ;
63: 494-7.
20. WOLFE F: A brief health status instrument:
CLINHAQ. Arthritis Rheum 1989; 32: S99
(abstract).
21. PINCUS T, CALLAHAN LF, BROOKS RH,
FUCHS HA, OLSEN NJ, KAYE JJ: Self-report
questionnaire scores in rheumatoid arthritis
compared with traditional physical, radio-
graphic, and laboratory measures. Ann Intern
Med 1989; 110: 259-66.
22. STRAND V, COHEN S, SCHIFF M et al.: Treat-
ment of active rheumatoid arthritis with lef-
lunomide compared with placebo and meth-
otrexate. Arch Intern Med 1999; 159: 2542-
50.
23. F E L S O N D T, A N D E R S O N JJ, BOERS M e t
al.: The American College of Rheumatology
preliminary core set of disease activity mea-
sures for rheumatoid arthritis clinical trials.
Arthritis Rheum 1993; 36: 729-40.
24. PINCUS T, SWEARINGEN C, WOLFE F: To-
ward a multidimensional health assessment
questionnaire (MDHAQ): Assessment of
advanced activities of daily living and psy-
chological status in the patient friendly health
assessment questionnaire format. A rt h r i t i s
Rheum 1999; 42: 2220-30.
25. PINCUS T, SOKKA T, KAUTIAINEN H: Pa-
tients seen for standard rheumatoid arthritis
care have significantly better articular, radio-
graphic, laboratory, and functional status in
2000 than in 1985. Arthritis Rheum 2005; 52:
1009-19.
26. BOERS M, TUGWELL P, FELSON DT et al.:
World Health Organization and International
League of Associations for Rheumatology
core endpoints for symptom modifying anti-
rheumatic drugs in rheumatoid arthritis clini-
cal trials. J Rheumatol 1994; 21 (Suppl. 41):
86-9.
27. TUGWELL P, BOERS M: OMERACT Com-
mittee. Proceedings of the OMERACT Con-
ferences on outcome measures in rheumatoid
arthritis clinical trials, Maastrict, Nether-
lands. J Rheumatol 1993; 20: 527-91.
28. STUCKI G, LIANG MH, STUCKI S, BRÜHL-
MANN P, MICHEL B A: A s e l f - a d m i n i s t e r e d
rheumatoid arthritis disease activity index
(RADAI) for epidemiologic research. Arthri -
tis Rheum 1995; 38: 795-8.
29. WOLFE F: Why the HAQ-II can be an effec-
tive substitute for the HAQ. Clin Exp
Rheumatol 2005; 23 (Suppl. 39): S29-S30.
30. S A L A F F I F, STA N C AT I A, NERI R, GRASSI
W, BOMBARDIERI S: Measuring functional
disablity in early rheumatoid arthritis: the
validity, reliability and responsiveness of the
Recent Onset Arthritis Disablity (ROAD)
Index. Clin Exp Rheumatol 2005; 23 (Suppl.
39): S31-S42.
31. PINCUS T: Documenting quality manage-
ment in rheumatic disease: Are patient ques-
tionnaires the best (and only) method? Arth -
ritis Care Res 1996; 9: 339-48.
32. WOLFE F, PINCUS T: Listening to the patient:
A practical guide to self-report question-
naires in clinical care. Arthritis Rheum 1999;
42: 1797-808.
33. PINCUS T, WOLFE F: An infrastructure of
patient questionnaires at each rheumatology
visit: Improving efficiency and documenting
care. J Rheumatol 2000; 27: 2727-30.
34. CALLAHAN LF, SMITH WJ, PINCUS T: Self-
report questionnaires in five rheumatic dis-
eases: Comparisons of health status con-
structs and associations with formal educa-
tion level. A rthritis Care Res 1989; 2: 122-31.
35. WOLFE F, PINCUS T: Data collection in the
clinic. Rheum Dis Clin North Am 1995; 21:
321-58.
36. ZOCHLING J, BRAUN J: Assessment of an-
kylosing spondylitis. Clin Exp Rheumatol
2005; 23 (Suppl. 39): S133-S141.
37. B E N N E T T R: The Fibromyalgia Impact Ques-
tionnaire (FIQ): A reviw of its development,
current version, operating characteristics and
uses. Clin Exp Rheumatol 2005; 23 (Suppl.
39): S152-S162.
38. BELLAMY N: The WOMAC Knee and Hip
Osteoarthritis Indices: Development, valida-
tion, globalization and influence on the dev-
elopment of the AUSCAN Hand Osteoarthri-
tis Indices. Clin Exp Rheumatol 2005; 23
(Suppl. 39): S148-S153.
39. WOLFE F:A brief introduction to the Nation-
al Data Bank for Rheumatic Diseases. Clin
Exp Rheumatol 2005; 23 (Suppl. 39): S168-
S171.
40. H AW L E Y DJ, W O L F E F: Sensitivity to
change of the Health Assessment Question-
naire (HAQ) and other clinical and health
status measures in rheumatoid arthritis: re-
sults of short term clinical trials and observa-
tional studies versus long term observational
studies. Arthritis Care Res 1992; 5: 130-6.
