
2020 ESC Guidelines for the diagnosis and
management of atrial fibrillation developed in
collaboration with the European Association of
Cardio-Thoracic Surgery (EACTS)
The Task Force for the diagnosis and management of atrial
fibrillation of the European Society of Cardiology (ESC)
Developed with the special contribution of the European Heart
Rhythm Association (EHRA) of the ESC
Authors/Task Force Members: Gerhard Hindricks* (Chairperson) (Germany),
Tatjana Potpara* (Chairperson) (Serbia), Nikolaos Dagres (Germany), Elena Arbelo
(Spain), Jeroen J. Bax (Netherlands), Carina Blomstro¨ m-Lundqvist (Sweden),
Giuseppe Boriani (Italy), Manuel Castella
1
(Spain), Gheorghe-Andrei Dan
(Romania), Polychronis E. Dilaveris (Greece), Laurent Fauchier (France),
Gerasimos Filippatos (Greece), Jonathan M. Kalman (Australia), Mark La Meir
1
* Corresponding authors: The two chairpersons contributed equally to the document.
Gerhard Hindricks, University Clinic of Cardiology, Heart Center Leipzig, Department of Cardiology and Electrophysiology, Leipzig Heart Institute, Stru¨mpellstr. 39, 04289
Tatjana Potpara, School of Medicine, Belgrade University, dr Subotica 8, 11000 Belgrade, Serbia, and Cardiology Clinic, Clinical Centre of Serbia, Visegradska 26, 11000 Belgrade,
ESC Committee for Practice Guidelines (CPG) and National Cardiac Societies document reviewers, and Author/Task Force Member affiliations: listed in
the Appendix.
1
Representing the European Association of Cardio-Thoracic Surgery (EACTS)
ESC entities having participated in the development of this document:
Associations: Association for Acute CardioVascular Care (ACVC), Association of Cardiovascular Nursing & Allied Professions (ACNAP), European Association of
Cardiovascular Imaging (EACVI), European Association of Preventive Cardiology (EAPC), European Association of Percutaneous Cardiovascular Interventions (EAPCI), European
Heart Rhythm Association (EHRA), Heart Failure Association (HFA).
Councils: Council on Stroke, Council on Valvular Heart Disease.
Working Groups: Cardiac Cellular Electrophysiology, Cardiovascular Pharmacotherapy, Cardiovascular Surgery, e-Cardiology, Thrombosis.
The content of these European Society of Cardiology (ESC) Guidelines has been published for personal and educational use only. No commercial use is authorized. No part of
the ESC Guidelines may be translated or reproduced in any form without written permission from the ESC. Permission can be obtained upon submission of a written request to
Oxford University Press, the publisher of the European Heart Journal and the party authorized to handle such permissions on behalf of the ESC (jour[email protected]).
Disclaimer The ESC Guidelines represent the views of the ESC and were produced after careful consideration of the scientific and medical knowledge and the evidence avail-
able at the time of their publication. The ESC is not responsible in the event of any contradiction, discrepancy and/or ambiguity between the ESC Guidelines and any other offi-
cial recommendations or guidelines issued by the relevant public health authorities, in particular in relation to good use of healthcare or therapeutic strategies. Health
professionals are encouraged to take the ESC Guidelines fully into account when exercising their clinical judgment, as well as in the determination and the implementation of pre-
ventive, diagnostic or therapeutic medical strategies; however, the ESC Guidelines do not override, in any way whatsoever, the individual responsibility of health professionals to
make appropriate and accurate decisions in consideration of each patient’s health condition and in consultation with that patient and, where appropriate and/or necessary, the
patient’s caregiver. Nor do the ESC Guidelines exempt health professionals from taking into full and careful consideration the relevant official updated recommendations or
guidelines issued by the competent public health authorities, in order to manage each patient’s case in light of the scientifically accepted data pursuant to their respective ethical
and professional obligations. It is also the health professional’s responsibility to verify the applicable rules and regulations relating to drugs and medical devices at the time of
prescription.
V
C
The European Society of Cardiology 2020. All rights reserved. For permissions please email: [email protected].
European Heart Journal (2020) 00,1125 ESC GUIDELINES
doi:10.1093/eurheartj/ehaa612

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
(Belgium), Deirdre A. Lane (United Kingdom), Jean-Pierre Lebeau (France),
Maddalena Lettino (Italy), Gregory Y. H. Lip (United Kingdom), Fausto J. Pinto
(Portugal), G. Neil Thomas (United Kingdom), Marco Valgimigli (Switzerland),
Isabelle C. Van Gelder (Netherlands), Bart P. Van Putte
1
(Netherlands),
Caroline L. Watkins (United Kingdom)
Document Reviewers: Paulus Kirchhof (CPG Review Coordinator) (United Kingdom/Germany), Michael
Ku¨ hne (CP G Review Coordinator) (Switzerland), Victor Aboyans (France), Anders Ahlsson
1
(Sweden),
Pawel Balsam (Poland), Johann Bauersachs (Germany), Stefano Benussi
1
(Italy), Axel Brandes (Denmark),
Frieder Braunschweig (Sweden), A. John Camm (United Kingdom), Davide Capodanno (Italy), Barbara
Casadei (United Kingdom), David Conen (Canada), Harry J. G. M. Crijns (Netherlands), Victoria Delgado
(Netherlands), Dobromir Dobrev (Germany), Heinz Drexel (Austria), Lars Eckardt (Germany), Donna
Fitzsimons (United Kingdom), Thierry Folliguet (France), Chris P. Gale (United Kingdom), Bulent Gorenek
(Turkey), Karl Georg Haeusler (Germany), Hein Heidbuchel (Belgium), Bernard Iung (France), Hugo A.
Katus (Germany), Dipak Kotecha (United Kingdom), Ulf Landmesser (Germany), Christophe Leclercq
(France), Basil S. Lewis (Israel), Julia Mascherbauer (Austria), Jose Luis Merino (Spain), Be´ la Merkely
(Hungary), Llu
ıs Mont (Spain), Christian Mueller (Switzerland), Klaudia V. Nagy (Hungary), Jonas Oldgren
(Sweden), Nikola Pavlovi
c (Croatia), Roberto F. E. Pedretti (Italy), Steffen E. Petersen (United Kingdom),
Jonathan P. Piccini (United States of America), Bogdan A. Popescu (Romania), Helmut Pu¨ rerfellner
(Austria), Dimitrios J. Richter (Greece), Marco Roffi (Switzerland), Andrea Rubboli (Italy), Daniel Scherr
(Austria), Renate B. Schnabel (Germany), Iain A. Simpson (United Kingdom), Evgeny Shlyakhto (Russia),
Moritz F. Sinner (Germany), Jan Steffel (Switzerland), Miguel Sousa-Uva (Portugal), Piotr Suwalski
1
(Poland), Martin Svetlosak (Slovakia), Rhian M. Touyz (United Kingdom)
The disclosure forms of all experts involved in the development of these guidelines are available on the
ESC website www.escardio.org/guidelines
For the Supplementary Data which include background information and detailed discussion of the data
that have provided the basis for the Guidelines see European Heart Journal online.
............................ ............................................ ....................................... ............................... ............. ............................... .........
Keywords
Guidelines
•
atrial fibrillation
•
anticoagulation
•
vitamin K antagonists
•
non-vitamin K antagonist oral antico-
agulants
•
left atrial appendage occlusion
•
rate control
•
rhythm control
•
cardioversion
•
antiarrhythmic
drugs
•
catheter ablation
•
pulmonary vein isolation
•
left atrial ablation
•
AF surgery
•
upstream therapy
•
ABC pathway
•
screening
•
stroke
•
recommendations
Table of contents
1Preamble ..........................................................6
2Introduction .......................................................8
2.1Whatisnewinthe2020Guidelines?............................9
3Definitionanddiagnosisofatrialfibrillation ........................ 13
3.1Definition ................................................... 13
3.2Diagnosticcriteriaforatrialfibrillation ........................ 14
3.3 Diagnosis of atrial high-rate episodes/subclinical atrial
fibrillation....................................................... 14
4Epidemiology .................................................... 14
4.1 Prediction of incident atrial fibrillation . . . . . . . . . . . . . . . . . . . . . . . . . 16
4.2Pathophysiologyofatrialfibrillation ........................... 16
5Clinicalfeaturesofatrialfibrillation................................ 16
6Atrialfibrillationsubtypes,burden,andprogression................ 18
6.1Classificationofatrialfibrillation .............................. 18
6.2 Definition and assessment of atrial fibrillation burden . . . . . . . . . . 19
6.3Atrialfibrillationprogression ................................. 20
6.4 Atrial cardiomyopathy: definition, classification, clinical
implications,anddiagnosticassessment........................... 20
7Screeningforatrialfibrillation..................................... 20
7.1Screeningtools .............................................. 20
7.2Screeningtypesandstrategies ................................ 22
7.3 Benefits from and risks of screening for atrial fibrillation . . . . . . . . 22
7.4 Cost-effectiveness of screening for atrial fibrillation . . . . . . . . . . . . 22
7.5Screeninginhigh-riskpopulations ............................ 23
7.5.1Elderly .................................................. 23
8 Diagnostic assessment in atrial fibrillation . . . . . . . . . . . . . . . . . . . . . . . . . 23
8.1Symptomsandqualityoflife.................................. 23
8.2Substrate.................................................... 23
9 Integrated management of patients with atrial fibrillation . . . . . . . . . . . 26
2 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
9.1 Definitions and components of integrated management
ofatrialfibrillationpatients....................................... 26
9.2Multidisciplinaryatrialfibrillationteams ....................... 26
9.2.1 Role of healthcare systems and budget constraints . . . . . . . . 26
9.3 Patient involvement and shared decision making . . . . . . . . . . . . . . . 26
9.3.1Patientvaluesandpreferences ........................... 26
9.3.2Patienteducation ........................................ 27
9.4Healthcareprofessionaleducation............................ 27
9.5Adherencetotreatment ..................................... 27
9.6 Technology tools supporting atrial fibrillation management . . . . 27
9.7 Advantages of integrated management of atrial
fibrillationpatients............................................... 28
9.8 Measures (or approaches) for implementation of
integratedmanagement ......................................... 28
9.9Treatmentburden ........................................... 28
9.10Patient-reportedoutcomes ................................. 28
10 Patient management: the integrated ABC pathway . . . . . . . . . . . . . . . 29
10.1 ‘A’ Anticoagulation/Avoidstroke ......................... 29
10.1.1Strokeriskassessment.................................. 29
10.1.2Bleedingriskassessment................................ 30
10.1.3 Absolute contraindications to oral anticoagulants . . . . . . . . 32
10.1.4Strokepreventiontherapies ............................ 32
10.1.4.1VitaminKantagonists............................... 32
10.1.4.2 Non-vitamin K antagonist oral anticoagulants . . . . . . . . 33
10.1.4.3Otherantithromboticdrugs ........................ 33
10.1.4.4 Combination therapy with oral anticoagulant and
antiplateletdrugs........................................... 34
10.1.4.5 Left atrial appendage occlusion and exclusion . . . . . . . . 34
10.1.4.5.1 Left atrial appendage occlusion devices . . . . . . . . . . 34
10.1.4.5.2 Surgical left atrial appendage
occlusionorexclusion ................................... 34
10.1.4.6 Long-term oral anticoagulation per atrial
fibrillationburden .......................................... 35
10.1.4.7 Long-term oral anticoagulation per symptom
controlstrategy ............................................ 35
10.1.5 Management of anticoagulation-related bleeding risk . . . . . 35
10.1.5.1 Strategies to minimize the risk of bleeding . . . . . . . . . . . 35
10.1.5.2High-riskgroups ................................... 35
10.1.5Decision-makingtoavoidstroke ........................ 35
10.2 ‘B’ Bettersymptomcontrol............................... 37
10.2.1Ratecontrol ........................................... 37
10.2.1.1 Target/optimal ventricular rate range . . . . . . . . . . . . . . . 37
10.2.1.2Drugs ............................................. 37
10.2.1.3Acuteratecontrol ................................. 38
10.2.1.4 Atrioventricular node ablation and pacing . . . . . . . . . . . 38
10.2.2Rhythmcontrol ........................................ 41
10.2.2.1 Indications for rhythm control . . . . . . . . . . . . . . . . . . . . . . 41
10.2.2.2Cardioversion ..................................... 42
10.2.2.2.1 Immediate cardioversion/elective cardioversion . . . 42
10.2.2.2.2Electricalcardioversion ........................ 42
10.2.2.2.3 Pharmacological cardioversion
(including‘pillinthepocket’) ............................. 42
10.2.2.2.4 Follow-up after cardioversion . . . . . . . . . . . . . . . . . . 42
10.2.2.3 Atrial fibrillation catheter ablation . . . . . . . . . . . . . . . . . . . 45
10.2.2.3.1Indications..................................... 45
10.2.2.3.2 Techniques and technologies . . . . . . . . . . . . . . . . . . . 47
10.2.2.3.3Complications ................................. 47
10.2.2.3.4 AF catheter ablation outcome and impact of
modifiableriskfactors.................................... 47
10.2.2.3.5 Follow-up after atrial fibrillation ablation . . . . . . . . 48
10.2.2.3.7 Risk assessment for recurrence of AF post
catheterablation......................................... 48
10.2.2.4Surgeryforatrialfibrillation ......................... 49
10.2.2.4.1 Concomitant surgery for atrial fibrillation:
indications,outcome,complications ...................... 50
10.2.2.4.2 Stand-alone surgery for atrial fibrillation:
indications,outcome,complications ...................... 50
10.2.2.5 Hybrid surgical/catheter ablation procedures . . . . . . . . 50
10.2.2.6 Peri-procedural stroke risk management in
patients undergoing rhythm control interventions . . . . . . . . . . . 51
10.2.2.6.1 Management of stroke risk and oral anticoagulant
therapy in atrial fibrillation patients undergoing
cardioversion............................................ 51
10.2.2.6.2 Management of stroke risk and oral
anticoagulant therapy in atrial fibrillation patients
undergoing atrial fibrillation catheter ablation . . . . . . . . . . . . . 52
10.2.2.6.3 Postoperative anticoagulation after surgery
foratrialfibrillation ...................................... 52
10.2.2.7 Long-term antiarrhythmic drug therapy for
rhythmcontrol............................................. 52
10.2.2.7.1Antiarrhythmicdrugs .......................... 52
10.3 ‘C Cardiovascular risk factors and concomitant
diseases:detectionandmanagement ............................. 58
10.3.1Lifestyleinterventions .................................. 58
10.3.1.1Obesityandweightloss ............................ 58
10.3.1.2 Alcohol and caffeine use . . . . . . . . . . . . . . . . . . . . . . . . . . . . 59
10.3.1.3Physicalactivity .................................... 59
10.3.2 Specific cardiovascular risk factors/comorbidities . . . . . . . . 59
10.3.2.1Hypertension ...................................... 59
10.3.2.2Heartfailure ....................................... 59
10.3.2.3Coronaryarterydisease............................ 59
10.3.2.4Diabetesmellitus................................... 59
10.3.2.5Sleepapnoea ...................................... 59
11 The ABC pathway in specific clinical settings/conditions/
patientpopulations ................................................ 60
11.1 Atrial fibrillation with haemodynamic instability . . . . . . . . . . . . . . 60
11.2 First-diagnosed (new-onset) atrial fibrillation . . . . . . . . . . . . . . . . . 60
11.3 Acute coronary syndromes, percutaneous coronary
intervention, and chronic coronary syndromes in patients with
atrialfibrillation ................................................. 61
11.4 Acute stroke or intracranial haemorrhage in patients with
atrialfibrillation ................................................. 64
11.4.1 Patients with atrial fibrillation and acute ischaemic
strokeortransientischaemicattack ........................... 64
11.4.2 Cryptogenic stroke/embolic stroke with
undeterminedsource ......................................... 64
11.4.3 Post-stroke patients without known atrial fibrillation . . . . . 65
11.4.4 Management of patients with atrial fibrillation
postintracranialhaemorrhage ................................. 65
11.5 Active bleeding on anticoagulant therapy: management
andreversaldrugs............................................... 67
11.6 Atrial fibrillation and heart failure . . . . . . . . . . . . . . . . . . . . . . . . . . . . 68
11.7 Atrial fibrillation and valvular heart disease . . . . . . . . . . . . . . . . . . . 68
11.8 Atrial fibrillation and chronic kidney disease . . . . . . . . . . . . . . . . . . 69
ESC Guidelines 3

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
11.9Atrialfibrillationandperipheralarterydisease................ 69
11.10 Atrial fibrillation and endocrine disorders . . . . . . . . . . . . . . . . . . . 69
11.11 Atrial fibrillation and gastrointestinal disorders . . . . . . . . . . . . . . 69
11.12 Atrial fibrillation and haematological disorders . . . . . . . . . . . . . . 70
11.13Theelderlyandfrailwithatrialfibrillation ................... 70
11.14 Patients with cognitive impairment/dementia . . . . . . . . . . . . . . . 70
11.15 Atrial fibrillation and congenital heart disease . . . . . . . . . . . . . . . 70
11.16 Atrial fibrillation in inherited cardiomyopathies and
primaryarrhythmiasyndromes .................................. 71
11.17Atrialfibrillationduringpregnancy.......................... 71
11.18 Atrial fibrillation in professional athletes . . . . . . . . . . . . . . . . . . . . 72
11.19Postoperativeatrialfibrillation ............................. 72
11.19.1PreventionofpostoperativeAF........................ 73
11.19.2 Prevention of thrombo-embolic events . . . . . . . . . . . . . . . . 73
12Preventionofatrialfibrillation ................................... 74
12.1Primarypreventionofatrialfibrillation ....................... 74
12.2Secondarypreventionofatrialfibrillation .................... 74
13Sex-relateddifferencesinatrialfibrillation........................ 74
14 Implementation of the atrial fibrillation guidelines . . . . . . . . . . . . . . . . . 75
15 Quality measures and clinical performance indicators
inthemanagementofatrialfibrillation .............................. 75
16 Epidemiology, clinical implications, and management of atrial
high-rateepisodes/subclinicalatrialfibrillation ....................... 75
17 Atrial fibrillation and other atrial tachyarrhythmias (atrial flutter
andatrialtachycardias) ............................................. 78
18Keymessages................................................... 78
19Gapsinevidence ............................................... 79
20 ‘What to do’ and ‘what not to do’ messages from the
Guidelines......................................................... 81
21Supplementarydata............................................. 85
22Appendix ...................................................... 85
23References ..................................................... 86
List of recommendations
Newrecommendations..............................................9
Changesintherecommendations .................................. 11
RecommendationsfordiagnosisofAF .............................. 14
Recommendations for structured characterization of AF . . . . . . . . . . . . 19
RecommendationsforscreeningtodetectAF....................... 23
Recommendations for diagnostic evaluation of patients with AF . . . . . 25
Recommendations about integrated AF management . . . . . . . . . . . . . . . 29
Recommendations for the prevention of thrombo-embolic
eventsinAF ....................................................... 36
Recommendations for ventricular rate control in patients with AF . . . 40
Recommendationsforrhythmcontrol.............................. 42
Recommendationsforcardioversion ............................... 45
Recommendations for rhythm control/catheter ablation of AF . . . . . . . 49
RecommendationsforsurgicalablationofAF ....................... 50
Recommendations for stroke risk management peri-cardioversion . . . 51
Recommendationsforstrokeriskmanagementperi-catheterablation ....52
Recommendations for postoperative anticoagulation after
AFsurgery ........................................................ 52
Recommendationsforlong-termantiarrhythmicdrugs .............. 58
Recommendations for lifestyle interventions and management of
risk factors and concomitant diseases in patients with AF . . . . . . . . . . . . 60
Recommendations for management of AF with haemodynamic
instability .......................................................... 60
Recommendations for patients with AF and an ACS, PCI, or CCS . . . . 63
Recommendations for the search for AF in patients with
cryptogenicstroke................................................. 65
Recommendations for secondary stroke prevention in AF
patientsafteracuteischaemicstroke................................ 65
Recommendations for stroke prevention in AF patients after intracranial
haemorrhage ..........................................................65
Recommendations for the management of active bleeding on OAC . . . . . 68
Recommendations for patients with valvular heart disease and AF . . . . 68
Recommendations for the management of AF in patients with
congenitalheartdisease ............................................ 71
Recommendations for the management of AF during pregnancy . . . . . 72
Recommendations for sports activity in patients with AF . . . . . . . . . . . . 72
RecommendationsforpostoperativeAF............................ 74
Recommendations pertaining to sex-related differences in AF . . . . . . . 75
Recommendations for quality measures in patients with AF . . . . . . . . . . 75
Recommendations for management of patients with AHRE . . . . . . . . . . 78
List of tables
Table1Classesofrecommendations .................................7
Table2Levelsofevidence ...........................................7
Table3Definitionofatrialfibrillation ............................... 13
Table4ClassificationofAF......................................... 18
Table 5 Sensitivity and specificity of various AF screening tools
consideringthe12-leadECGasthegoldstandard ................... 22
Table6EHRAsymptomscale ...................................... 24
Table7StrokeriskfactorsinpatientswithAF ....................... 30
Table 8 CHA
2
DS
2
-VAScscore ..................................... 31
Table 9 Risk factors for bleeding with OAC and antiplatelet
therapy ........................................................... 31
Table10ClinicalriskfactorsintheHAS-BLEDscore ................ 32
Table11DoseselectioncriteriaforNOACs........................ 33
Table 12 Antithrombotic therapy after left atrial appendage
occlusion.......................................................... 34
Table13DrugsforratecontrolinAF............................... 39
Table 14 Antiarrhythmic drugs used for restoration of sinus rhythm . . . 44
Table 15 Goals of follow-up after cardioversion of AF . . . . . . . . . . . . . . . 45
Table 16 Procedure-related complications in catheter ablation and
thoracoscopicablationofAF ....................................... 47
Table 17 Key issues in follow-up after AF catheter ablation . . . . . . . . . . 48
Table18Principlesofantiarrhythmicdrugtherapy .................. 53
Table 19 Rules to initiate antiarrhythmic drugs for long-term
rhythmcontrolinAF .............................................. 53
Table 20 AADs used for long-term maintenance of sinus
rhythminAFpatients .............................................. 54
Table 21 Non-antiarrhythmic drugs with antiarrhythmic
properties(upstreamtherapy) ..................................... 57
Table 22 Summary of quality indicators for the diagnosis
andmanagementofAF............................................. 76
List of figures
Figure1DiagnosisofAHRE/subclinicalAF .......................... 14
4 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Figure 2 Epidemiology of AF: prevalence; and lifetime risk and
projectedriseintheincidenceandprevalence ...................... 15
Figure3SummaryofriskfactorsforincidentAF..................... 16
Figure 4 Clinical presentation of AF and AF-related outcomes . . . . . . . 17
Figure 5 4S-AF scheme as an example of structured
characterizationofAF ............................................. 19
Figure6SystemsusedforAFscreening ............................. 21
Figure 7 Potential benefits from and risks of screening for AF . . . . . . . . . 22
Figure 8 Diagnostic work-up and follow-up in AF patients . . . . . . . . . . . . 24
Figure9ImaginginAF.............................................. 25
Figure 10 Components of integrated AF management . . . . . . . . . . . . . . . 26
Figure 11 Integrated AF management team (an example) . . . . . . . . . . . . 27
Figure 12 ‘A’ - Anticoagulation/Avoid stroke:
The‘AF3-step’pathway ........................................... 36
Figure13Outlineofratecontroltherapy ........................... 38
Figure14Choiceofratecontroldrugs.............................. 40
Figure15Rhythmcontrolstrategy.................................. 41
Figure 16 Flowchart for decision making on cardioversion of AF
depending on clinical presentation, AF onset, oral anticoagulation
intake,andriskfactors ............................................. 43
Figure 17 Indications for catheter ablation of symptomatic AF . . . . . . . . 46
Figure 18 Risk factors for AF contributing to the development
of an abnormal substrate translating into poorer outcomes with
rhythmcontrolstrategies .......................................... 48
Figure19Long-termrhythmcontroltherapy........................ 57
Figure 20 Post-procedural management of patients with AF
andACS/PCI ...................................................... 62
Figure21(Re-)initiationofanticoagulationpost-intracranialbleeding ....66
Figure 22 Management of active bleeding in patients
receivinganticoagulation ........................................... 67
Figure23ManagementofpostoperativeAF ......................... 73
Figure 24 Progression of atrial high-rate episode burden and
stroke rates according to AHRE daily burden and CHA2DS2-VASc
score ............................................................. 77
Figure 25 Proposed management of AHRE/subclinical AF . . . . . . . . . . . . 77
CentralIllustration.ManagementofAF.............................. 80
List of boxes
Box 1 About post-procedural management of patients with AF
andACSand/orPCI ............................................... 61
Box 2 About acute ischaemic stroke in patients with AF . . . . . . . . . . . . . 64
Abbreviations and acronyms
Abbreviations and acronyms
4S-AF Stroke risk, Symptom severity, Severity of AF
burden, Substrate severity
AAD Antiarrhythmic drug
ABC Atrial fibrillation Better Care [includes A (avoid
stroke), B (better symptom control), and C
(cardiovascular risk factors and comorbid
conditions management)]
ABC-bleeding Age, Biomarkers (haemoglobin, cTnT hs T, GDF-
15), and Clinical history (prior bleeding)
ABC-stroke Age, Biomarkers, Clinical history (stroke risk score)
ACS Acute coronary syndromes
ACTIVE W Atrial Fibrillation Clopidogrel Trial with Irbesartan
for Prevention of Vascular Events trial
AF Atrial fibrillation
AFFIRM Atrial Fibrillation Follow-up Investigation of
Rhythm Management
AFL Atrial flutter
AHRE Atrial high-rate episode
AMICA Atrial Fibrillation Management in Congestive
Heart Failure With Ablation
ARCADIA AtRial Cardiopathy and Antithrombotic Drugs In
Prevention After Cryptogenic Stroke
ARISTOTLE Apixaban for Reduction in Stroke and Other
Thromboembolic Events in Atrial Fibrillation
ARREST-AF Aggressive Risk Factor Reduction Study
Implication for AF
AST Aspartate aminotransferase
ATRIA Anticoagulation and Risk Factors in Atrial
Fibrillation (score)
ATTICUS Apixaban for treatment of embolic stroke of
undetermined source
AVERROES Apixaban Versus Acetylsalicylic Acid (ASA) to
Prevent Stroke in Atrial Fibrillation Patients Who
Have Failed or Are Unsuitable for Vitamin K
Antagonist Treatment
b.i.d. bis in die (twice a day)
BP Blood pressure
bpm Beats per minute
C
2
HEST CAD/COPD (1 point each), Hypertension (1
point), Elderly ( >_75 years, 2 points), Systolic
heart failure (2 points), and Thyroid disease
(hyperthyroidism, 1 point) (score)
CABANA Catheter ABlation vs. ANtiarrhythmic Drug
Therapy for Atrial Fibrillation
CAD Coronary artery disease
CAPTAF Catheter Ablation compared with
Pharmacological Therapy for Atrial Fibrillation
CASTLE-AF Catheter Ablation vs. Standard conventional
Treatment in patients with LEft ventricular
dysfunction and Atrial Fibrillation
CATCH-ME Characterizing AF by Translating its Causes into
Health Modifiers in the Elderly
CCB Calcium channel blocker
CCS Chronic coronary syndrome
CHA
2
DS
2
-
VASc
Congestive heart failure, Hypertension, Age >_75
years, Diabetes mellitus, Stroke, Vascular disease,
Age 6574 years, Sex category (female)
CHADS
2
CHF history, Hypertension history, Age >_75 y,
Diabetes mellitus history, Stroke or TIA
symptoms previously
CHF Congestive heart failure
CI Confidence interval
CIED Cardiac implantable electronic device
CKD Chronic kidney disease
COP-AF Colchicine For The Prevention Of Perioperative
Atrial Fibrillation In Patients Undergoing
Thoracic Surgery
ESC Guidelines 5

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
COPD Chronic obstructive pulmonary disease
CPAP Continuous positive airway pressure
CrCl Creatinine clearance
CRT Cardiac resynchronization therapy
CT Computed tomography
CTI Cavotricuspid isthmus
cTnT-hs High-sensitivity troponin T
DAPT Dual antiplatelet therapy
EAST Early treatment of Atrial fibrillation for Stoke
prevention Trial
ECG Electrocardiogram
EHRA European Heart Rhythm Association
ELAN Early versus Late initiation of direct oral
Anticoagulants in post-ischaemic stroke patients
with atrial fibrillatioN
ENGAGE
AF-TIMI 48
Effective aNticoaGulation with factor XA next
GEneration in Atrial Fibrillation-Thrombolysis In
Myocardial Infarction 48
ENTRUST-
AF PCI
Edoxaban Treatment Versus Vitamin K
Antagonist in Patients With Atrial Fibrillation
Undergoing Percutaneous Coronary Intervention
ESC European Society of Cardiology
GARFIELD-AF Global Anticoagulant Registry in the FIELD -
Atrial Fibrillation
GDF-15 Growth differentiation factor-15
HAS-BLED Hypertension, Abnormal renal/liver function,
Stroke, Bleeding history or predisposition, Labile
INR, Elderly (>65 years), Drugs/alcohol
concomitantly
HCM Hypertrophic cardiomyopathy
HF Heart failure
HFpEF Heart failure with preserved ejection fraction
HFrEF Heart failure with reduced ejection fraction
HR Hazard ratio
i.v. intravenous
ICH Intracranial haemorrhage
IMPACT-AF Integrated Management Program Advancing
Community Treatment of Atrial Fibrillation
INR International normalized ratio
LA Left atrium/atrial
LAA Left atrial appendage
LEGACY Long-term Effect of Goal-directed weight
management on an Atrial fibrillation Cohort: a 5-
Year follow-up study
LGE-CMR Late gadolinium contrast-enhanced cardiac
magnetic resonance
LMWH Low-molecular-weight heparin
LV Left ventricular
LVEF Left ventricular ejection fraction
LVH Left ventricular hypertrophy
mAFA Mobile AF App
MANTRA-PAF Medical Antiarrhythmic Treatment or
Radiofrequency Ablation in Paroxysmal Atrial
Fibrillation
MRI Magnetic resonance imaging
NDCC Non-dihydropyridine calcium channel blocker
NOAC Non-vitamin K antagonist oral anticoagulant
NSAID Non-steroidal anti-inflammatory drug
NYHA New York Heart Association
o.d. omni die (once daily)
OAC Oral anticoagulant
OPTIMAS OPtimal TIMing of Anticoagulation after Stroke
OSA Obstructive sleep apnoea
PACES Anticoagulation for New-Onset Post-Operative
Atrial Fibrillation After CABG
PAD Peripheral artery disease
PCI Percutaneous coronary intervention
PCORI Patient-Centred Outcomes Research Institute
PIONEER
AF-PCI
OPen-Label, Randomized, Controlled,
Multicenter Study ExplorIng TwO TreatmeNt
StratEgiEs of Rivaroxaban and a Dose-Adjusted
Oral Vitamin K Antagonist Treatment Strategy in
Subjects with Atrial Fibrillation who Undergo
Percutaneous Coronary Intervention
PREVAIL Watchman LAA Closure Device in Patients With
Atrial Fibrillation Versus Long Term Warfarin
Therapy
PRO Patient-reported outcome
PROTECT AF Watchman Left Atrial Appendage System for
Embolic Protection in Patients With Atrial
Fibrillation
PVI Pulmonary vein isolation
QoL Quality of life
QRS QRS interval
QTc Corrected QT interval
RACE Race Control Efficacy in Permanent Atrial
Fibrillation
RCT Randomized controlled trial
RE-DUAL Randomized Evaluation of Dual Antithrombotic
Therapy with Dabigatran vs. Triple Therapy with
Warfarin in Patients with Nonvalvular Atrial
Fibrillation Undergoing Percutaneous Coronary
Intervention
RE-CIRCUIT Randomized Evaluation of dabigatran etexilate
Compared to warfarIn in pulmonaRy vein
ablation: assessment of different peri-
proCedUral antIcoagulation sTrategies
REHEARSE-AF REmote HEArt Rhythm Sampling using the
AliveCor hear monitor to scrEen for Atrial
Fibrillation
RE-LY Randomized Evaluation of Long Term
Anticoagulant Therapy
ROCKET AF Rivaroxaban Once Daily Oral Direct Factor Xa
Inhibition Compared with Vitamin K Antagonism
for Prevention of Stroke and Embolism Trial in
Atrial Fibrillation
SAMe-TT
2
R
2
Sex (female), Age (<60 years), Medial history,
Treatment, Tobacco use, Race (non-Caucasian)
(score)
SBP Systolic blood pressure
START Optimal Delay Time to Initiate Anticoagulation
After Ischemic Stroke in AF
6 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
STEMI ST-segment elevation myocardial infarction
TIA Transient ischaemic attack
TOE Transoesophageal echocardiography
TTR Time in therapeutic range
UFH Unfractionated heparin
US United States of America
VHD Valvular heart disease
VKA Vitamin K antagonist
WOEST What is the Optimal antiplatElet and
anticoagulant therapy in patients with oral
anticoagulation and coronary StenTing
1 Preamble
Guidelines summarize and evaluate available evidence with the aim of
assisting health professionals in proposing the best management
strategies for an individual patient with a given condition. Guidelines
and their recommendations should facilitate decision making of
health professionals in their daily practice. However, the final deci-
sions concerning an individual patient must be made by the responsi-
ble health professional(s) in consultation with the patient and
caregiver as appropriate.
A great number of Guidelines have been issued in recent years by
the European Society of Cardiology (ESC), as well as by other soci-
eties and organizations. Because of their impact on clinical practice,
quality criteria for the development of guidelines have been estab-
lished in order to make all decisions transparent to the user. The rec-
ommendations for formulating and issuing ESC Guidelines can be
found on the ESC website (https://www.escardio.org/Guidelines/
Clinical-Practice-Guidelines/Guidelines-development/Writing-ESC-
Guidelines). The ESC Guidelines represent the official position of
the ESC on a given topic and are regularly updated.
In addition to the publication of Clinical Practice Guidelines, the ESC
carries out the EurObservational Research Programme of international
registries of cardiovascular diseases and interventions which are essen-
tial to assess, diagnostic/therapeutic processes, use of resources and
adherence to Guidelines. These registries aim at providing a better
understanding of medical practice in Europe and around the world,
based on high-quality data collected during routine clinical practice.
Furthermore, the ESC has developed and embedded, in some of
its guidelines, a set of quality indicators (QIs) which are tools
to evaluate the level of implementation of the Guidelines and may be
used by the ESC, hospitals, healthcare providers and professionals to
measure clinical practice as well as used in educational programmes,
alongside the key messages from the Guidelines, to improve quality
of care and clinical outcomes.
The Members of this Task Force were selected by the ESC, includ-
ing representation from its relevant ESC sub-specialty groups, in
order to represent professionals involved with the medical care of
patients with this pathology. Selected experts in the field undertook a
comprehensive review of the published evidence for management of
a given condition according to ESC Committee for Practice
Guidelines (CPG) policy. A critical evaluation of diagnostic and thera-
peutic procedures was performed, including assessment of the
riskbenefit ratio. The level of evidence and the strength of the rec-
ommendation of particular management options were weighed and
graded according to predefined scales, as outlined below.
The experts of the writing and reviewing panels provided declara-
tion of interest forms for all relationships that might be perceived as
real or potential sources of conflicts of interest. Their declarations of
interest were reviewed according to the ESC declaration of interest
rules and can be found on the ESC website (http://www.escardio.org/
guidelines). This process ensures transparency and prevents potential
biases in the development and review processes. Any changes in dec-
larations of interest that arise during the writing period were notified
to the ESC and updated. The Task Force received its entire financial
support from the ESC without any involvement from the healthcare
industry.
Table 1 Classes of recommendations
Classes of recommendations
Class I Evidence and/or general agreement
that a given treatment or procedure is
Is recommended or is indicated
Wording to use
Class III Evidence or general agreement that the
given treatment or procedure is not
useful/effective, and in some cases
may be harmful.
Is not recommended
Class IIb
established by evidence/opinion.
May be considered
Class IIa Weight of evidence/opinion is in Should be considered
Class II
©
ESC 2020
ESC Guidelines 7

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
The ESC CPG supervises and coordinates the preparation of new
Guidelines. The Committee is also responsible for the endorsement
process of these Guidelines. The ESC Guidelines undergo extensive
review by the CPG and external experts. After appropriate revisions
the Guidelines are approved by all the experts involved in the Task
Force. The finalized document is approved by the CPG for publica-
tion in the European Heart Journal. The Guidelines were developed
after careful consideration of the scientific and medical knowledge
and the evidence available at the time of their dating.
The task of developing ESC Guidelines also includes the crea-
tion of educational tools and implementation programmes for the
recommendations including condensed pocket guideline versions,
summary slides, booklets with essential messages, summary cards
for non-specialists, and an electronic version for digital applications
(smartphones, etc.). These versions are abridged and thus, for
more detailed information, the user should always access the full
text version of the Guidelines, which is freely available via the ESC
website and hosted on the EHJ website. The National Cardiac
Societies of the ESC are encouraged to endorse, adopt, translate,
and implement all ESC Guidelines. Implementation programmes
are needed because it has been shown that the outcome of disease
may be favourably influenced by the thorough application of clini-
cal recommendations.
Health professionals are encouraged to take the ESC Guidelines
fully into account when exercising their clinical judgment, as well as in
the determination and the implementation of preventive, diagnostic
or therapeutic medical strategies. However, the ESC Guidelines do
not override in any way whatsoever the individual responsibility of
health professionals to make appropriate and accurate decisions in
consideration of each patient’s health condition and in consultation
with that patient or the patient’s caregiver where appropriate and/or
necessary. It is also the health professional’s responsibility to verify
the rules and regulations applicable in each country to drugs and devi-
ces at the time of prescription.
2 Introduction
Atrial fibrillation (AF) poses significant burden to patients, physicians,
and healthcare systems globally. Substantial research efforts and
resources are being directed towards gaining detailed information
about the mechanisms underlying AF, its natural course and effective
treatments (see also the ESC Textbook of Cardiovascular Medicine:
CardioMed) and new evidence is continuously generated and
published.
The complexity of AF requires a multifaceted, holistic, and multidisci-
plinary approach to the management of AF patients, with their active
involvement in partnership with clinicians. Streamlining the care of
patients with AF in daily clinical practice is a challenging but essential
requirement for effective management of AF. In recent years, substantial
progresshasbeenmadeinthedetectionofAFanditsmanagement,
and new evidence is timely integrated in this third edition of the ESC
guidelines on AF. The 2016 ESC AF Guidelines introduced the concept
of the five domains to facilitate an integrated structured approach to AF
care and promote consistent, guideline-adherent management for all
patients. The Atrial Fibrillation Better Care (ABC) approach in the 2020
ESC AF Guidelines is a continuum of this approach, with the goal to fur-
ther improve the structured management of AF patients, promote
patient values, and finally improve patient outcomes.
Reflecting the multidisciplinary input into the management of
patients with AF and interpretation of new evidence, the Task Force
includes cardiologists with varying subspecialty expertise, cardiac sur-
geons, methodologists, and specialist nurses amongst its members.
Further to adhering to the standards for generating recommenda-
tions that are common to all ESC guidelines (see preamble), this Task
Force discussed each draft recommendation during web-based con-
ference calls dedicated to specific chapters, followed by consensus
modifications and an online vote on each recommendation. Only rec-
ommendations that were supported by at least 75% of the Task
Force members were included in the Guidelines.
Table 2 Levels of evidence
Level of
evidence A
Data derived from multiple randomized clinical trials
or meta-analyses.
Level of
evidence B
Data derived from a single randomized clinical trial
or large non-randomized studies.
Level of
evidence C
Consensus of opinion of the experts and/or small studies,
retrospective studies, registries.
©ESC 2020
8 ESC Guidelines

2.1 What is new in the 2020 Guidelines?
New recommendations
Recommendations Class
a
Recommendations for diagnosis of AF
ECG documentation is required to establish the diagnosis of AF.
A standard 12-lead ECG recording or a single-lead ECG tracing of >_30 s showing heart rhythm with no discernible repeating P waves
and irregular RR intervals (when atrioventricular conduction is not impaired) is diagnostic of clinical AF.
I
Recommendations for structured characterization of AF
Structured characterization of AF, which includes clinical assessment of stroke risk, symptom status, burden of AF, and evaluation of sub-
strate, should be considered in all AF patients, to streamline the assessment of AF patients at different healthcare levels, inform treatment
decision making, and facilitate optimal management of AF patients.
IIa
Recommendations for screening to detect AF
When screening for AF it is recommended that:
•
The individuals undergoing screening are informed about the significance and treatment implications of detecting AF.
•
A structured referral platform is organized for screen-positive cases for further physician-led clinical evaluation to confirm the diagno-
sis of AF and provide optimal management of patients with confirmed AF.
•
Definite diagnosis of AF in screen-positive cases is established only after the physician reviews the single-lead ECG recording of >_30 s
or 12-lead ECG and confirms that it shows AF.
I
Recommendations about integrated AF management
It is recommended to routinely collect PROs to measure treatment success and improve patient care.
I
Recommendations for the prevention of thrombo-embolic events in AF
For a formal risk-score-based assessment of bleeding risk, the HAS-BLED score should be considered to help address modifiable bleeding
risk factors, and to identify patients at high risk of bleeding (HAS-BLED score >_3) for early and more frequent clinical review and follow-
up.
IIa
Stroke and bleeding risk reassessment at periodic intervals is recommended to inform treatment decisions (e.g. initiation of OAC in
patients no longer at low risk of stroke) and address potentially modifiable bleeding risk factors
I
In patients with AF initially at low risk of stroke, first reassessment of stroke risk should be made 4 - 6 months after the index evaluation.
IIa
Estimated bleeding risk, in the absence of absolute contraindications to OAC, should not in itself guide treatment decisions to use OAC
for stroke prevention.
III
Clinical pattern of AF (i.e. first detected, paroxysmal, persistent, long-standing persistent, permanent) should not condition the indication
to thromboprophylaxis.
III
Recommendations for cardioversion
Pharmacological cardioversion of AF is indicated only in a haemodynamically stable patient, after consideration of the thrombo-embolic
risk.
I
For patients with sick-sinus syndrome, atrioventricular conduction disturbances or prolonged QTc (>500 ms), pharmacological cardio-
version should not be attempted unless risks for proarrhythmia and bradycardia have been considered.
III
Recommendations for rhythm control/catheter ablation of AF
General recommendations
For the decision on AF catheter ablation, it is recommended to take into consideration the procedural risks and the major risk factors
for AF recurrence following the procedure and discuss them with the patient.
I
Repeated PVI procedures should be considered in patients with AF recurrence provided the patient’s symptoms were improved after
the initial PVI.
IIa
AF catheter ablation after antiarrhythmic drug therapy failure
AF catheter ablation for PVI should be considered for rhythm control after one failed or intolerant to beta-blocker treatment to improve
symptoms of AF recurrences in patients with paroxysmal and persistent AF.
IIa
First-line therapy
AF catheter ablation for PVI should/may be considered as first-line rhythm control therapy to improve symptoms in selected patients
with symptomatic:
•
Paroxysmal AF episodes, or
IIa
•
Persistent AF without major risk factors for AF recurrence as an alternative to AAD class I or III, considering patient choice, benefit,
and risk.
IIb
Continued
ESC Guidelines 9

Techniques and technologies
Use of additional ablation lesions beyond PVI (low voltage areas, lines, fragmented activity, ectopic foci, rotors, and others) may be con-
sidered but is not well established.
IIb
Lifestyle modification and other strategies to improve outcomes of ablation
Strict control of risk factors and avoidance of triggers are recommended as part of rhythm control strategy.
I
Recommendations for stroke risk management peri-cardioversion
It is recommended that the importance of adherence and persistence to NOAC treatment both before and after cardioversion is
strongly emphasized to patients.
I
In patients with AF duration of >24 h undergoing cardioversion, therapeutic anticoagulation should be continued for at least 4 weeks
even after successful cardioversion to sinus rhythm (beyond 4 weeks, the decision about long-term OAC treatment is determined by the
presence of stroke risk factors).
IIa
In patients with a definite duration of AF <_24 h and a very low stroke risk (CHA
2
DS
2
-VASc of 0 in men or 1 in women) post-cardiover-
sion anticoagulation for 4 weeks may be omitted.
IIb
Recommendations for stroke risk management peri-catheter ablation
In AF patients with stroke risk factors not taking OAC before ablation, it is recommended that pre-procedural management of stroke
risk includes initiation of anticoagulation and:
•
Preferably, therapeutic OAC for at least 3 weeks before ablation, or
•
Alternatively, the use of TOE to exclude LA thrombus before ablation.
I
IIa
For patients undergoing AF catheter ablation who have been therapeutically anticoagulated with warfarin, dabigatran, rivaroxaban, apixa-
ban, or edoxaban, performance of the ablation procedure without OAC interruption is recommended.
I
Recommendations for long-term AADs
In AF patients treated with sotalol, close monitoring of QT interval, serum potassium levels, CrCl, and other proarrhythmia risk factors is
recommended.
I
In AF patients treated with flecainide for long-term rhythm control, concomitant use of an atrioventricular nodal-blocking drug (if toler-
ated) should be considered.
IIa
Sotalol may be considered for long-term rhythm control in patients with normal LV function or with ischaemic heart disease if close
monitoring of QT interval, serum potassium levels, CrCl, and other proarrhythmia risk factors is provided.
IIb
Recommendations for lifestyle interventions and management of risk factors and concomitant diseases in AF
Identification and management of risk factors and concomitant diseases is recommended as an integral part of treatment in AF patients.
I
Modification of unhealthy lifestyle and targeted therapy of intercurrent conditions is recommended to reduce AF burden and symptom
severity.
I
Opportunistic screening for AF is recommended in hypertensive patients.
I
Opportunistic screening for AF should be considered in patients with OSA.
IIa
Recommendations for patients with AF and an ACS, PCI, or CCS
Recommendations for AF patients with ACS
In AF patients with ACS undergoing an uncomplicated PCI, early cessation (<_1 week) of aspirin and continuation of dual therapy with an
OAC and a P2Y
12
inhibitor (preferably clopidogrel) for up to 12 months is recommended if the risk of stent thrombosis is low or if con-
cerns about bleeding risk prevail over concerns about risk of stent thrombosis, irrespective of the type of stent used.
I
Recommendations in AF patients with a CCS undergoing PCI
After uncomplicated PCI, early cessation (<_1 week) of aspirin and continuation of dual therapy with OAC for up to 6 months and clopi-
dogrel is recommended if the risk of stent thrombosis is low or if concerns about bleeding risk prevail over concerns about risk of stent
thrombosis, irrespective of the type of stent used.
I
Recommendations for the management of active bleeding on OAC
Four-factor prothrombin complex concentrates should be considered in AF patients on VKA who develop a severe bleeding
complication.
IIa
Recommendations for the management of AF during pregnancy
Acute management
In pregnant women with HCM, cardioversion should be considered for persistent AF.
IIa
Ibutilide or flecainide i.v. may be considered for termination of AF in stable patients with structurally normal hearts.
IIb
Long-term management (oral administration of drugs)
Flecainide, propafenone, or sotalol should be considered to prevent AF if atrioventricular nodal-blocking drugs fail.
IIa
Digoxin or verapamil should be considered for rate control if beta-blockers fail.
IIa
Continued
10 ESC Guidelines

Recommendations for postoperative AF
Long-term OAC therapy to prevent thrombo-embolic events should be considered in patients at risk for stroke with postoperative AF
after non-cardiac surgery, considering the anticipated net clinical benefit of OAC and informed patient preferences.
IIa
Beta-blockers should not be used routinely for the prevention of postoperative AF in patients undergoing non-cardiac surgery.
III
Recommendations pertaining to sex-related differences in AF
Women with symptomatic paroxysmal or persistent AF should be offered timely access to rhythm control therapies, including AF cathe-
ter ablation, when appropriate for medical reasons.
IIa
Recommendations for quality measures in AF
The introduction of tools to measure quality of care and identify opportunities for improved treatment quality and AF patient outcome
should be considered by practitioners and institutions.
IIa
AAD = antiarrhythmic drug; ACS = acute coronary syndrome; AF = atrial fibrillation; CCS = chronic coronary syndrome; CHA
2
DS
2
-VASc = Congestive heart failure,
Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 6574 years, Sex category (female); CrCl = creatinine clearance; ECG = electrocardiogram;
HAS-BLED = Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile INR, Elderly (>65 years), Drugs/alcohol concomitantly; HCM =
hypertrophic cardiomyopathy; i.v. = intravenous; LA = left atrium/atrial; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagulant; OSA = obstructive
sleep apnoea; PCI = percutaneous coronary intervention; PRO = patient-reported outcome; PVI = pulmonary vein isolation; QTc = corrected QT interval; TOE = transoeso-
phageal echocardiography; VKA = vitamin K antagonist therapy.
a
Class of recommendation.
Changes in the recommendations
Recommendations about integrated AF management
2020 Class
a
2016 Class
a
To optimize shared decision making about specific AF treatment
option(s) in consideration, it is recommended that:
•
Physicians inform the patient about advantages/limitations and
benefit/risks associated with considered treatment option(s);
and
•
Discuss the potential burden of the treatment with the patient
and include the patient’s perception of treatment burden in
the treatment decision.
I
Placing patients in a central role in decision making should be con-
sidered in order to tailor management to patient preferences and
improve adherence to long-term therapy
IIa
Recommendations for the prevention of thrombo-embolic events in AF
For bleeding risk assessment, a formal structured risk-score-
based bleeding risk assessment is recommended to help identify
non-modifiable and address modifiable bleeding risk factors in all
AF patients, and to identify patients potentially at high risk of
bleeding who should be scheduled for early and more frequent
clinical review and follow-up.
I
Bleeding risk scores should be considered in AF patients on oral
anticoagulation to identify modifiable risk factors for major
bleeding.
IIa
In patients on VKAs with low time in INR therapeutic range (e.g.
TTR<70%), recommended options are:
•
Switching to a NOAC but ensuring good adherence and per-
sistence with therapy; or
•
Efforts to improve TTR (e.g. education/counselling and more
frequent INR checks).
I
AF patients already on treatment with a VKAs may be considered
for NOAC treatment if TTR is not well controlled despite good
adherence, or if patient preference without contraindications to
NOAC (e.g. prosthetic valve).
IIb
IIa
Recommendations for rhythm control/catheter ablation of AF
AF catheter ablation after drug therapy failure
AF catheter ablation for PVI is recommended for rhythm control
after one failed or intolerant class I or III AAD, to improve symp-
toms of AF recurrences in patients with:
•
Paroxysmal AF, or
•
Persistent AF without major risk factors for AF recurrence, or
•
Persistent AF with major risk factors for AF recurrence.
I
Catheter or surgical ablation should be considered in patients with
symptomatic persistent or long-standing persistent AF refractory
to AAD therapy to improve symptoms, considering patient choice,
benefit and risk, supported by an AF Heart Team.
IIa
Continued
ESC Guidelines 11

First-line therapy
AF catheter ablation:
•
Is recommended to reverse LV dysfunction in AF patients
when tachycardia-induced cardiomyopathy is highly probable,
independent of their symptom status.
I
AF ablation should be considered in symptomatic patients with AF
and HFrEF to improve symptoms and cardiac function when tachy-
cardiomyopathy is suspected.
IIa
•
Should be considered in selected AF patients with HFrEF to
improve survival and reduce HF hospitalization.
IIa
Techniques and technologies
Complete electrical isolation of the pulmonary veins is recom-
mended during all AF catheter-ablation procedures.
I
Catheter ablation should target isolation of the pulmonary veins
using radiofrequency ablation or cryothermy balloon catheters.
IIa
If patient has a history of CTI-dependent atrial flutter or if typical
atrial flutter is induced at the time of AF ablation, delivery of a
CTI lesion may be considered.
IIb
Ablation of common atrial flutter should be considered to prevent
recurrent flutter as part of an AF ablation procedure if docu-
mented or occurring during the AF ablation
IIa
Lifestyle modification and other strategies to improve outcomes of ablation
Weight loss is recommended in obese patients with AF, particu-
larly those who are being evaluated to undergo AF ablation.
I
In obese patients with AF, weight loss together with management
of other risk factors should be considered to reduce AF burden
and symptoms.
IIa
Recommendations for stroke risk management peri-cardioversion
In patients with AF undergoing cardioversion, NOACs are rec-
ommended with at least similar efficacy and safety as warfarin.
I
Anticoagulation with heparin or a NOAC should be initiated as
soon as possible before every cardioversion of AF or atrial flutter.
IIa
Recommendations for stroke risk management peri-catheter ablation
After AF catheter ablation, it is recommended that:
•
Systemic anticoagulation with warfarin or a NOAC is contin-
ued for at least 2 months post ablation, and
•
Long-term continuation of systemic anticoagulation beyond 2
months post ablation is based on the patient’s stroke risk pro-
file and not on the apparent success or failure of the ablation
procedure.
I
All patients should receive oral anticoagulation for at least 8 weeks
after catheter ablation.
IIa
Recommendations for long-term antiarrhythmic drugs
Amiodarone is recommended for long-term rhythm control in all
AF patients, including those with HFrEF. However, owing to its
extracardiac toxicity, other AADs should be considered first
whenever possible.
I
Amiodarone is more effective in preventing AF recurrences than
other AAD, but extracardiac toxic effects are common and
increase with time. For this reason, other AAD should be consid-
ered first.
IIa
Recommendations for lifestyle interventions and management of risk factors and concomitant diseases in patients with AF
Attention to good BP control is recommended in AF patients
with hypertension to reduce AF recurrences and risk of stroke
and bleeding.
I
BP control in anticoagulated patients with hypertension should be
considered to reduce the risk of bleeding
IIa
Physical activity should be considered to help prevent AF inci-
dence or recurrence, with the exception of excessive endurance
exercise, which may promote AF.
IIa
Moderate regular physical activity is recommended to prevent AF,
while athletes should be counselled that long-lasting intense sports
participation can promote AF
I
Optimal management of OSA may be considered, to reduce AF
incidence, AF progression, AF recurrences, and symptoms.
IIb
OSA treatment should be optimized to reduce AF recurrences and
improve AF treatment results.
IIa
Recommendations for stroke prevention in AF patients after ICH
In AF patients at high risk of ischaemic stroke, (re-)initiation of
OAC, with preference for NOACs over VKAs in NOAC-eligible
patients, should be considered in consultation with a neurologist/
stroke specialist after:
•
A trauma-related ICH
•
Acute spontaneous ICH (which includes subdural, subarach-
noid, or intracerebral haemorrhage), after careful considera-
tion of risks and benefits
IIa
After ICH oral anticoagulation in patients with AF may be reiniti-
ated after 48 weeks provided the cause of bleeding or the rele-
vant risk factor has been treated or controlled.
IIb
Continued
12 ESC Guidelines

3 Definition and diagnosis of atrial
fibrillation
3.1 Definition
Recommendations for postoperative AF
Long-term OAC therapy to prevent thrombo-embolic events
may be considered in patients at risk for stroke with postopera-
tive AF after cardiac surgery, considering the anticipated net clini-
cal benefit of OAC therapy and informed patient preferences.
IIb
Long-term anticoagulation should be considered in patients with
AF after cardiac surgery at risk for stroke, considering individual
stroke and bleeding risk.
IIa
AAD = antiarrhythmic drug; AF = atrial fibrillation; BP = blood pressure; CTI = cavotricuspid isthmus; HFrEF = heart failure with reduced ejection fraction; ICH = intracranial
haemorrhage; INR = international normalized ratio; LV = left ventricular; LVEF = left ventricular ejection fraction; NOAC = non-vitamin K antagonist oral anticoagulant; OAC
= oral anticoagulant or oral anticoagulation; PVI = pulmonary vein isolation; TTR = time in therapeutic range; VKA = vitamin K antagonist.
a
Class of recommendation.
Table 3 Definition of atrial fibrillation
Definition
AF A supraventricular tachyarrhythmia with uncoordinated atrial electrical activation and consequently ineffective atrial contrac-
tion.
Electrocardiographic characteristics of AF include:
•
Irregularly irregular R-R intervals (when atrioventricular conduction is not impaired),
•
Absence of distinct repeating P waves, and
•
Irregular atrial activations.
Currently used terms
Clinical AF Symptomatic or asymptomatic AF that is documented by surface ECG.
The minimum duration of an ECG tracing of AF required to establish the diagnosis of clinical AF is at least 30 seconds, or
entire 12-lead ECG.
1,2
AHRE, subclinical AF Refers to individuals without symptoms attributable to AF, in whom clinical AF is NOT previously detected (that is, there is no surface
ECG tracing of AF), see also section 3.3.
AHRE - events fulfilling programmed or specified criteria for AHRE that are detected by CIEDs with an atrial lead allowing
automated continuous monitoring of atrial rhythm and tracings storage. CIED-recorded AHRE need to be visually inspected
because some AHRE may be electrical artefacts/false positives.
Subclinical AF includes AHRE confirmed to be AF, AFL, or an AT, or AF episodes detected by insertable cardiac monitor or
wearable monitor and confirmed by visually reviewed intracardiac electrograms or ECG-recorded rhythm.
Device-programmed rate criterion for AHRE is >_175 bpm, whereas there is no specific rate limit for subclinical AF.
The criterion for AHRE duration is usually set at >_5 min (mainly to reduce the inclusion of artefacts), whereas a wide range of subclinical AF duration cut-
offs (from 10 - 20 seconds to >24 hours) is reported in studies of the association of subclinical AF with thromboembolism. The reported duration refers to
either the longest single episode or, more commonly, total duration of AHRE/subclinical AF during the specified monitoring period.
Although not completely identical, the terms AHRE and subclinical AF are often used interchangeably (in this document the amalgamated term AHRE/sub-
clinical AF will be used for practicality).
35
Whereas a large body of high-quality evidence from RCTs informing the management of AF patients pertains
exclusively to ‘clinical’ AF (that is, the ECG documentation of AF was a mandatory inclusion criterion in those RCTs), data on optimal management of AHRE
and subclinical AF are lacking. For this reason, AF is currently described as either ‘clinical’ or ‘AHRE/subclinical’, until the results of several ongoing RCTs
expected to inform the management of AHRE and ‘subclinical’ AF are available.
AHRE = atrial high-rate episode; AF = atrial fibrillation; ECG = electrocardiogram; AFL = atrial flutter; AT = atrial tachycardia; bpm = beats per minute; CIED = cardiac implant-
able electronic device; ECG = electrocardiogram; RCT = randomized controlled trial.
ESC Guidelines 13

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
3.2 Diagnostic criteria for atrial
fibrillation
The diagnosis of AF requires rhythm documentation with an electro-
cardiogram (ECG) tracing showing AF. By convention, an episode
lasting at least 30 s is diagnostic for clinical AF.
6
3.3 Diagnosis of atrial high-rate episodes/
subclinical atrial fibrillation
Various implanted devices and wearable monitors allow detection
of atrial high-rate episodes (AHRE) /subclinical AF (Figure 1).
3
Owing to a short monitoring, detection of AHRE/subclinical AF via
external ECG is less likely.
7
When AHRE/subclinical AF is detected by a device/wearable,
inspection of the stored electrograms/ECG rhythm strips is recom-
mended to exclude artefacts or other causes of inappropriate
detection.
8,9
4 Epidemiology
Worldwide, AF is the most common sustained cardiac arrhythmia in
adults
10
(Figure 2, upper panel). AF is associated with substantial mor-
bidity and mortality, thus portending significant burden to patients,
societal health, and health economy (Figure 2,lowerpanel)
(Supplementary section 1).
Recommendations for diagnosis of AF
Recommendations Class
a
Level
b
ECG documentation is required to establish the
diagnosis of AF.
•
A standard 12-lead ECG recording or a sin-
gle-lead ECG tracing of >_30 s showing heart
rhythm with no discernible repeating P waves
and irregular RR intervals (when atrioventric-
ular conduction is not impaired) is diagnostic
of clinical AF.
6
IB
AF = atrial fibrillation; ECG = electrocardiogram.
a
Class of recommendation.
b
Level of evidence.
©ESC 2020
Pacemaker/implantable defibrillator
Figure 1 Diagnosis of AHRE/subclinical AF. CIEDs with an atrial lead can monitor atrial rhythm and store the tracings. ICMs have no intracardiac leads
but continuously monitor cardiac electrical activity by recording and analysing a single-lead bipolar surface ECG based on a specific algorithm. Left-bottom
image: pacemaker with a right atrial lead, and a ventricular lead in the right ventricular apex. In addition to pacing at either site, these leads can sense activity
in the respective cardiac chamber. The device can also detect pre-programmed events, such as AHRE. Right-bottom image: subcutaneous ICM: these devi-
ces have no intra-cardiac leads and essentially record a single, bipolar, surface ECG, with inbuilt algorithms for detection of AHRE or AF. AF = atrial fibrilla-
tion; AHRE = atrial high rate episode; CIED = cardiac implantable electronic device; ECG = electrocardiogram; ICM = insertable cardiac monitor; RCT =
randomized clinical trial.
14 ESC Guidelines

Figure 2 Epidemiology of AF: prevalence (upper panel)
1020
; and lifetime risk and projected rise in the incidence and prevalence (lower panel).
2134
AF = atrial fibrillation; AFL = atrial flutter; BP = blood pressure; CI = confidence interval; EU = European Union.
a
Smoking, alcohol consumption, body
mass index, BP, diabetes mellitus (type 1 or 2), and history of myocardial infarction or heart failure.
b
Risk profile: optimal - all risk factors are negative or
within the normal range; borderline - no elevated risk factors but >1 borderline risk factor; elevated - >1 elevated risk factor.
ESC Guidelines 15

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
The currently estimated prevalence of AF in adults is between 2%
and 4%,
10
and a 2.3-fold rise
11
is expected,
12,13
owing to extended
longevity in the general population and intensifying search for undiag-
nosed AF.
15
Increasing age is a prominent AF risk factor, but increas-
ing burden of other comorbidities including hypertension, diabetes
mellitus, heart failure (HF), coronary artery disease (CAD), chronic
kidney disease (CKD),
21
obesity, and obstructive sleep apnoea
(OSA) is also important;
2226
modifiable risk factors are potent con-
tributors to AF development and progression
27,28
(Figure 3). The age-
adjusted incidence, prevalence, and lifetime risk of AF are lower in
women vs. men and in non-Caucasian vs. Caucasian cohorts.
10,1420
A previous lifetime AF risk estimate of 1 in 4 individuals
29,30
was
recently revised to 1 in 3 individuals of European ancestry at index
age of 55 years.
31,32
The AF lifetime risk depends on age, genetic, and
(sub)clinical factors.
10,33,34
The observed impact of clinical risk factor
burden/multiple comorbidity on AF risk (Figure 3,lowerpanel
31
) sug-
gests that an early intervention and modifiable risk factor control
could reduce incident AF.
4.1 Prediction of incident atrial
fibrillation
Identifying individuals at higher risk of developing AF in the commun-
ity could facilitate targeting of preventive interventions and screening
programmes for early AF detection, for example in high-risk sub-
groups such as post-stroke patients.
73
Various predictive scores for
new-onset AF have been proposed (Supplementary Table 2), but
none has been widely used in clinical practice.
4.2 Pathophysiology of atrial fibrillation
A complex interplay of triggers, perpetuators, and substrate develop-
ment eventually resulting in AF occurrence is shown in Supplementary
Figure 1.
5 Clinical features of atrial
fibrillation
Clinical presentation of AF and AF-related outcomes are shown
in Figure 4 (see also Supplementary section 2 and Su pplementary
Box 1).
6 Atrial fibrillation subtypes,
burden, and progression
6.1 Classification of atrial fibrillation
Different AF classifications have been proposed but, tradition-
ally, five patterns of AF are distinguished, based on presentation,
duration, and spontaneous termination of AF episodes
(Table 4).
143
In patients experiencing both paroxysmal and persistent AF epi-
sodes, the more common type should be used for classification.
However, clinically determined AF patterns do not correspond
well to the AF burden measured by long-term ECG
monitoring.
144146
Other classifications of AF reflect the presence of symptoms
(asymptomatic AF is diagnosed with an opportune 12-lead ECG or
rhythm strip in asymptomatic patients) or underlying cause of AF
©ESC 2020
Figure 3 Summary of risk factors for incident AF
10,22,33,3572
(Supplementary Table 1 for full list). AF = atrial fibrillation; COPD = chronic obstructive pul-
monary disease.
16 ESC Guidelines

©ESC 2020
Figure 4 Clinical presentation of AF and AF-related outcomes.
10,31,74140
AF = atrial fibrillation; HF = heart failure; HR = Hazard Ratio; LV = left ven-
tricle; MI = myocardial infarction; QoL = quality of life.
Patients with AF may have various symptoms
92,108,109,128,131
but 50 - 87% are initially asymptomatic,
75,82,88,111,117,120,125,127
with possibly a less favourable progno-
sis.
79,82,87,88,117,119,127,134,139
First-onset AF symptoms are less well studied,
92,105,108,109,
,
127
may change with treatment
119
and AF recurrences are commonly asymptomatic.
113
Stroke/systolic embolism: annual AF-related stroke risk in AF patients depends on comorbidities.
78,84,85,91,106,112
Cardioembolic strokes associated with AF are usually
severe, highly recurrent, often fatal, or with permanent disability.
10,83,115
In a population-based registry, patients with new-onset AF also had increased rates of systemic embo-
lism.
89
ESC Guidelines 17

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
(e.g. postoperative AF, see section 11.19). Classifying AF by underlying
drivers could inform management, but the evidence in support of the
clinical use of such classification is lacking (Supplementary Table 3).
Terms that should no longer be used to describe AF are listed in
Table 4.
Recommendations for AF management are not based on the tem-
poral AF patterns, except for the restoration of sinus
rhythm.
143,149,150
It is very unlikely that a simple but comprehensive
AF classification will be proposed, given the multiplicity of factors rel-
evant for its management, advances in AF monitoring, multiplicity of
risk assessment tools, evolving treatments, and complexity of AF
itself. Indeed, a paradigm shift from classification towards a structured
characterization of AF, addressing specific domains with treatment and
prognostic implications has been recently proposed.
151
Such a
scheme would streamline the assessment of AF patients at any
healthcare level, thus facilitating communication among physicians,
Figure 4 Continued
Left ventricular (LV) dysfunction and HF: multiple AF-associated mechanisms/myocardial alterations may lead to LV dysfunction and HF,
102,138
resulting in a high prev-
alence and incidence of HF among AF patients. Sharing common risk factors, AF and HF often coexist, or may precipitate/exacerbate each other, resulting in significantly greater
mortality than either condition alone.
140
Hospitalization: approximately 30% of AF patients have at least one, and 10% have >_2, hospital admissions annually,
99,110,129
being twice as likely to be hospitalized as age-
and sex-matched non-AF individuals (37.5% vs. 17.5%, respectively).
98
In a nationwide cohort, AF was the main cause for admission in 14% of hospitalized patients but their in-
hospital mortality was <1%.
101
The most common reasons for hospitalization of AF patients were cardiovascular disorders (49%), non-cardiovascular causes (43%) and bleeding
(8%).
129
Quality of life (QoL) and functional status: >60% of AF patients have significantly impaired QoL/exercise tolerance,
81,88,136
but only 17% have disabling symptoms.
88
QoL is significantly lower in women,
81,107,114,124
young individuals, and those with comorbidities.
118
AF burden
100
may also affect QoL, but only psychological functioning consis-
tently predicted symptoms and QoL.
136
Patients with AF more often developed anxiety disorders,
126
had a higher burden of depressive symptoms,
123
and poorer QoL with a
Distressed personality type (Type D).
103
Key symptom and QoL drivers are important to identify optimal AF treatment. It is also important to confirm that symptoms are
related to AF or, if absent, to exclude a subconscious adaptation to living with suboptimal physical capacity by asking for breathlessness or fatigue on exertion and recording pos-
sible improvements after cardioversion.
Cognitive impairment/dementia: AF may lead to cognitive impairment ranging from mild dysfunction to dementia
97,104,141
via clinically apparent or silent stroke or insuf-
ficiently understood stroke-independent pathways.
94,96,97,122
Magnetic resonance imaging (MRI) studies have shown that AF is associated with a greater than twofold increase in
the odds of having silent cerebral ischaemia.
90,121,142
A recent expert consensus paper summarized the available data.
86
Mortality: AF is independently associated with a twofold increased risk of all-cause mortality in women and a 1.5-fold increase in men,
77,80,130,137
with an overall 3.5-fold
mortality risk increase.
31
Whereas the mechanistic explanation for this association is multifaceted, associated comorbidities play an important role.
95
In a recent study, the most
common causes of death among AF patients were HF (14.5%), malignancy (23.1%), and infection/sepsis (17.3%), whereas stroke-related mortality was only 6.5%.
76
These and
other recent data indicate that, in addition to anticoagulation and HF treatment, comorbid conditions need to be actively treated in the endeavour to reduce AF-related
mortality.
77,93,116,133
Table 4 Classification of AF
AF pattern Definition
First diagnosed AF not diagnosed before, irrespective of its duration or the presence/severity of AF-related symptoms.
Paroxysmal AF that terminates spontaneously or with intervention within 7 days of onset.
Persistent AF that is continuously sustained beyond 7 days, including episodes terminated by cardioversion (drugs or electrical cardioversion)
after >_7 days
Long-standing
persistent
Continuous AF of >12 months’ duration when decided to adopt a rhythm control strategy.
Permanent AF that is accepted by the patient and physician, and no further attempts to restore/maintain sinus rhythm will be undertaken.
Permanent AF represents a therapeutic attitude of the patient and physician rather than an inherent pathophysiological
attribute of AF, and the term should not be used in the context of a rhythm control strategy with antiarrhythmic drug
therapy or AF ablation. Should a rhythm control strategy be adopted, the arrhythmia would be re-classified as ‘long-standing persis-
tent AF’.
Terminology that should be abandoned
Lone AF A historical descriptor. Increasing knowledge about the pathophysiology of AF shows that in every patient a cause is present. Hence, this
term is potentially confusing and should be abandoned.
147
Valvular/non-
valvular AF
Differentiates patients with moderate/severe mitral stenosis and those with mechanical prosthetic heart valve(s) from other patients
with AF, but may be confusing
148
and should not be used.
Chronic AF Has variable definitions and should not be used to describe populations of AF patients.
AF = atrial fibrillation.
18 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
treatment decision making, and optimal management of AF patients,
and should become a standard in clinical practice when reporting an
AF case.
The proposed 4S-AF scheme (Stroke risk, Symptom severity,
Severity of AF burden, Substrate severity) includes four AF-related
domains (Figure 5).
151
The currently used assessment tools/classifica-
tions pertinent to specific domains (e.g. stroke risk scores, symptom
scores, clinical factors, imaging modalities, etc.) can be easily fitted in,
but the 4S-AF has great potential for future refinements guided by
advances in technology, and the most appropriate descriptors of AF
domains are yet to be defined. Given the descriptors of AF included
in the 4S-AF scheme, the structured characterization of AF patients
using 4S-AF could also provide prognostic information, but the clini-
cal utility and prognostic value of the 4S-AF scheme needs extensive
validation in different AF cohorts and clinical settings.
6.2 Definition and assessment of atrial
fibrillation burden
The term ‘burden’ refers to various AF aspects (e.g. epidemiological,
economic).
144
Regarding continuous device-based monitoring, ‘AF
burden’ is currently defined as the overall time spent in AHRE/sub-
clinical AF during a specified monitoring period (e.g. 1 day). Both the
time in AF and the monitoring period should be acknowledged when
reporting AF burden (most studies reported the maximum time
spent in AF over a 24-h period), but optimal measures are yet to be
determined.
152
The term ‘AF burden’ is different from ‘burden of AF’,
the latter referring to AF consequences.
Clinical AF burden is routinely determined by AF temporal pat-
tern
146
(Tab le 4) and intermittent ECG monitoring,
153
neither corre-
sponding well to the long-term ECG monitoring. The relationship of
clinical AF burden with specific outcomes is not well characterized,
154
but may be associated with higher risk of incident HF
155
and all-cause
mortality,
156
while the association with quality of life (QoL) is complex
and data about cognitive impairment/dementia are lacking.
86
Recent
randomized controlled trial (RCT) data consistently showed signifi-
cantly lower residual thrombo-embolic risk among anticoagulated
patients with paroxysmal vs. persistent AF,
156159
whereas earlier
trial-based
160
and observational data
161,162
are contradictory. Among
non-anticoagulated patients, stroke risk was lower with paroxysmal
than non-paroxysmal AF,
156
and a greater total AF burden (but not the
longest AF episode) was independently associated with higher
thrombo-embolic event rates.
163
Clinical AF burden may influence the
response to rhythm control therapy.
164,165
The presence of >6 h of AF
per week (especially when progressing to >24 h weekly) was associ-
ated with increased mortality, especially in women.
166
©ESC 2020
Figure 5 4S-AF scheme as an example of structured characterization of AF.
151
AF = atrial fibrillation; CHA
2
DS
2
-VASc = Congestive heart failure,
Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 65 - 74 years, Sex category (female); CT = computed tomography; EHRA =
European Heart Rhythm Association; LA = left atrium; MRI = magnetic resonance imaging; QoL = quality of life; TOE = transoesophageal echocardiogra-
phy; TTE = transthoracic echocardiography.
Recommendations for structured characterization of AF
Recommendations Class
a
Level
b
Structured characterization of AF, which
includes clinical assessment of stroke risk, symp-
tom status, burden of AF, and evaluation of sub-
strate, should be considered in all AF patients,
to streamline the assessment of AF patients at
different healthcare levels, inform treatment
decision-making, and facilitate optimal manage-
ment of AF patients.
151
IIa C
AF = atrial fibrillation
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 19

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Available evidence on the association of AF burden with AF-
related outcomes is insufficient to guide treatment and should not be
a major factor in treatment decisions. Comprehensive management
of modifiable cardiovascular risk factors/comorbidity reduces AF bur-
den (section 10.3).
6.3 Atrial fibrillation progression
Transition from paroxysmal to non-paroxysmal AF (or from subclini-
cal to clinical AF)
154,167169
is often characterized by advancing atrial
structural remodelling or worsening of atrial cardiomyopathy.
170,171
Assessment of AF progression depends on duration of rhythm
monitoring and underlying substrate.
172,173
Reported annual rates of
paroxysmal AF progression range from <1% to 15% (up to 27 - 36%
in studies with >_10-year follow-up).
169,174
Risk factors for AF pro-
gression include age, HF, hypertension, CKD, chronic pulmonary dis-
eases, diabetes mellitus, previous stroke, and left atrial (LA) size,
167
whereas the added predictive value of biomarkers is presently not
well defined. Older age is associated with permanent AF,
82,117,154
and
various triggers may also play a role, with different progression pat-
terns resulting from their interaction with substrate remodelling.
171
Progression to persistent/permanent AF is associated with adverse
cardiovascular events, hospitalizations, and death,
166
but it is unclear
whether AF progression is a determinant of adverse prognosis or
rather a marker of an underlying progressive disease/substrate.
175,176
The true impact of different therapeutic interventions at different dis-
ease stages on AF progression and associated outcomes is also less
well defined.
6.4 Atrial cardiomyopathy: definition,
classification, clinical implications, and
diagnostic assessment
Important progress in understanding AF mechanisms and thrombo-
genicity reconsiders the role of atrial cardiomyopathy (i.e. atrial struc-
tural, architectural, contractile, or electrophysiological changes with
potentially relevant clinical manifestations).
170
Clinical classification of atrial cardiomyopathy should be based on
the atrial structure, morphology, electrical and mechanical function,
and the diagnosis could be based on easily accessible parameters (e.g.
aetiology, the prothrombotic state,
177
and abnormal LA volume/
function).
178
Major clinical issues in AF (i.e. prevention of thrombo-
embolic complications and AF progression) are influenced by atrial
remodelling; and, importantly, AF is not only a risk factor for but also
a marker of atrial cardiomyopathy, which could explain the lack of
temporal relationship between detected AF and stroke.
179
The diagnostic algorithm for atrial cardiomyopathy should follow a
stepwise approach, identifying risk factors for atrial cardiomyop-
athy,
170
atrial electrical and mechanical dysfunction,
180
and increased
thrombotic risk.
181
More data are needed to define prognostic and
treatment implications of different atrial cardiomyopathy morpho-
functional forms.
7 Screening for atrial fibrillation
Multiple factors (i.e. increasing AF prevalence, previously unknown
AF detection in about 10% of all ischaemic strokes,
4,182
high preva-
lence of asymptomatic AF,
117
potential to prevent AF-related strokes
with appropriate treatment and increasing availability of AF detection
tools) have fuelled international initiatives to implement screening for
AF in clinical practice.
172
Asymptomatic clinical AF has been independently associated with
increased risk of stroke and mortality compared with symptomatic
AF.
82,117,127,183
Data derived from studies of incidentally detected
asymptomatic AF are the closest possible approximation of the risk
of stroke and death in screen-detected AF subjects, because delaying
treatment to discern a natural history would be unethical.
Observational data suggest that screen-detected AF responds to
treatment similarly to AF detected by routine care,
183
thus favouring
AF screening.
Although AF fulfils many of the criteria for disease screening
184
(Supplementary Figure 2), RCT data to confirm the health benefits
from screening for AF and inform the choice of optimal screening
programmes and strategies for its implementation are scarce.
185,186
Advances in wearable technology will likely yield inexpensive and
practical options for AF detection and AF burden assessment in the
near future.
7.1 Screening tools
The systems used for AF screening are shown in Table 5 and
Figure 6.
173,187
Mobile health technologies are rapidly developing for AF detection
and other purposes (>100 000 mHealth apps and >_400 wearable
activity monitors are currently available).
197
Cautionisneededin
their clinical use, as many are not clinically validated. Several studies
evaluated AF detection using smartwatches,
198,199
thus opening new
perspectives for AF detection targeting specific populations at risk.
Machine learning and artificial intelligence may be capable of identify-
ing individuals with previous AF episodes from a sinus rhythm ECG
recording,
200
which would be a major technological breakthrough in
AF detection.
200
The Apple Heart study
201
included 419 297 self-enrolled smart-
watch app users (mean age 40 years) in the United States of America
(USA), of whom 0.5% received an irregular pulse notification (0.15%
of those aged <40 years, 3.2% among those aged >65 years).
Subsequent (notification-triggered) 1-week ECG patch monitoring
revealed AF in 34% of monitored participants. The Huawei Heart
study
202
included 187 912 individuals (mean age 35 years, 86.7%
male), of whom 0.23% received a ‘suspected AF’ notification. Of
those effectively followed up, 87.0% were confirmed as having AF,
with the positive predictive value of photoplethysmography signals
being 91.6% [95% confidence interval (CI) 91.5 - 91.8]. Of those with
identified AF, 95.1% entered an integrated AF management pro-
gramme using a mobile AF App (mAFA).
When AF is detected by a screening tool, including mobile or
wearable devices, a single-lead ECG tracing of >_30 s or 12-lead ECG
showing AF analysed by a physician with expertise in ECG rhythm
interpretation is necessary to establish a definitive diagnosis of AF
(devices capable of ECG recording enable direct analysis of the
device-provided tracings). When AF detection is not based on an
ECG recording (e.g. with devices using photoplethysmography) or in
case of uncertainty in the interpretation of device-provided ECG
tracing, a confirmatory ECG diagnosis has to be obtained using addi-
tional ECG recording (e.g. 12-lead ECG, Holter monitoring, etc.)
20 ESC Guidelines

©ESC 2020
Figure 6 Systems used for AF screening. Pulse palpation, automated BP monitors, single-lead ECG devices, PPG devices, other sensors (using seismocar-
diography, accelerometers, and gyroscopes, etc.) used in applications for smartphones, wrist bands, and watches. Intermittent smartwatch detection of AF
is possible through PPG or ECG recordings. Smartwatches and other ‘wearables’ can passively measure pulse rate from the wrist using an optical sensor
for PPG and alerting the consumer of a pulse irregularity (based on a specific algorithm for AF detection analysing pulse irregularity and varia-
bility).
172,173,188196
AF = atrial fibrillation; BP = blood pressure; ECG = electrocardiogram; PPG = photoplethysmography.
ESC Guidelines 21

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
The data reported in Table 5 should be interpreted with caution,
as assessment of sensitivity and specificity in many studies was based
on small observational cohorts, with a substantial risk of bias due to
signal selection. Moreover, there is a continuous evolution of algo-
rithms and technologies available in commercial devices.
Two recent meta-analyses reported that screening for AF using an
ECG would not detect more cases than would screening with pulse
palpation.
215
7.2 Screening types and strategies
Commonly used AF screening types and strategies
172,173,216
include
opportunistic or systematic screening of individuals above a certain
age (usually >_65 years) or with other characteristics suggestive of
increased stroke risk, using intermittent single-point or repeated 30-s
ECG recording over 2 weeks. The appropriate frequency of monitor-
ing using smartphones or watches is undefined. Primary care, phar-
macies, or community screening during special events is a good
setting for AF screening.
172,173
Overall, there was no significant differ-
ence between systematic vs. opportunistic or general practice vs.
community screening in a meta-analysis, but repeated heart associ-
ated with significantly better effectiveness compared with single
assessment.
215
Importantly, a structured referral of screen-detected
or suspected AF cases for further clinical evaluation should be organ-
ized, to provide an appropriate management.
7.3 Benefits from and risks of screening
for atrial fibrillation
Potential advantages and disadvantages of detecting a previously
undiagnosed AF through screening are shown in Figure 7.
173
Screening can also highlight cases of known suboptimally managed
AF.
217
Intermittent ECG recording increased new AF detection four-
fold.
217
In the REHEARSE-AF (REmote HEArt Rhythm Sampling using
the AliveCor heart monitor to scrEen for Atrial Fibrillation) con-
trolled study using a smartphone/tablet-based single-lead ECG
system twice weekly over 12 months vs. routine care resulted in a
3.9-fold increase in AF detection in patients aged >_65 years.
218
Appropriate patient information and screening programme organiza-
tion with rapid ECG clarification may reduce anxiety induced by sus-
picion of abnormality.
7.4 Cost-effectiveness of screening for
atrial fibrillation
Higher AF-related medical costs justify strategies to identify and
treat undiagnosed AF.
219
Opportunistic AF screening is associated
with lower costs than systematic screening.
173
Appropriate choice
of the screening tool and setting is important,
220
and a favourable
cost-effectiveness profile has been estimated for screening pro-
grammes based on pulse palpation, hand-held ECG devices, and
Table 5 Sensitivity and specificity of various AF screening tools considering the 12-lead ECG as the gold standard
173
Sensitivity Specificity
Pulse taking
203
87 - 97% 70 - 81%
Automated BP monitors
204207
93 - 100% 86 - 92%
Single lead ECG
208211
94 - 98% 76 - 95%
Smartphone apps
188,189,191,195,212,213
91.5 - 98.5% 91.4 - 100%
Watches
196,198,213,214
97 - 99% 83 - 94%
AF = atrial fibrillation; BP = blood pressure; ECG = electrocardiogram.
©ESC 2020
Figure 7 Potential benefits from and risks of screening for AF. AF = atrial fibrillation; ECG = electrocardiogram; OAC = oral anticoagulant; SE =systemic
embolism.
22 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
smartphones with pulse photoplethysmography algorithms.
172
Both systematic and opportunistic screening are more cost-
effective than routine practice for patients >_65 years, with oppor-
tunistic screening more likely to be cost-effective than systematic
population screening.
1491
7.5 Screening in high-risk populations
7.5.1 Elderly
The risk of AF (often asymptomatic) and stroke increase with
age,
82,127,221
thus justifying AF screening in the elderly. Opportunistic
AF screening seems to be cost-effective in elderly populations (>_65
years)
222
and among 75 - 76-year-old individuals undergoing a 2-
week intermittent ECG screening.
223
Pulse palpation and/or short-term ECG among the elderly (>_65
years) yielded an AF prevalence of 4.4%, with previously undiagnosed
AF in 1.4%, suggesting a number needed to screen of 70.
224
Repeated
hand-held ECG recordings over 2 weeks in an unselected population
aged 75 - 76 years increased the detection of asymptomatic AF up to
7.4% in subjects with >_2 stroke risk factors.
225
8 Diagnostic assessment in atrial
fibrillation
Often occurring in patients with cardiovascular risk factors/comor-
bidities, AF may sometimes be a marker of undiagnosed conditions.
Hence, all AF patients will benefit from a comprehensive cardiovascu-
lar assessment (Figure 8).
The ‘standard package’ for diagnostic evaluation of AF patients
should include complete medical history and assessment of concomi-
tant conditions, AF pattern, stroke risk, AF-related symptoms,
thrombo-embolism, and LV dysfunction.
143
A 12-lead ECG is recom-
mended in all AF patients, to establish the diagnosis of AF, assess ven-
tricular rate during AF, and check for the presence of conduction
defects, ischaemia, or signs of structural heart disease. Laboratory
tests (thyroid and kidney function, serum electrolytes, full blood
count) and transthoracic echocardiography (LV size and function, LA
size, valvular disease, and right heart size and systolic function) are
needed to guide treatment. Based on the patient’s characteristics,
specific additional information can be obtained. Most AF patients
need regular follow-up (primary care) to ensure continued optimal
management.
8.1 Symptoms and quality of life
As symptoms related to AF may range from none to disabling, and
rhythm control treatment decisions (including catheter ablation) are
influenced by symptom severity, symptom status should be charac-
terized using the European Heart Rhythm Association (EHRA) symp-
tom scale
228
(Table 6), and the relation of symptoms (especially if
non-specific, such as shortness of breath, fatigue, chest discomfort,
etc.) to AF should be elucidated because symptoms may also result
from undiagnosed or suboptimally managed concomitant cardiovas-
cular risk factors or pathological conditions.
229
In selected AF patients, long-term ECG monitoring is recom-
mended to assess the adequacy of rate control or to relate symp-
toms with AF episodes. Sometimes the association of symptoms with
AF can be established only retrospectively, after successful rhythm
control intervention. In selected patients, a trial of sinus rhythm using
cardioversion and a quantified patient perception of symptoms using
a validated assessment tool (Supplementary Table 4) may inform the
decision about subsequent AF catheter ablation (section 10.2).
Symptomatic and functional improvement with rhythm control
therapies (cardioversion,
232234
antiarrhythmic medications, and AF
catheter-ablation procedures
235242
) largely depends on sinus
rhythm maintenance
243
; however, QoL may improve despite AF
recurrences, unless AF burden is high
244
(e.g. >2 h daily
100
)owingto
optimized management of cardiovascular risk factors or comorbid-
ities
245
or a treatment expectancy effect. The effect of AF treat-
ment
246,247
is supported by reports of persistently improved QoL 10
years after paroxysmal AF catheter ablation in patients with a low AF
progression rate.
248
8.2 Substrate
The substrate for AF relates to LA dilation and fibrosis with subse-
quent LA dysfunction and delay in electromechanical conduction.
Recommendations for screening to detect AF
Recommendation Class
a
Level
b
Opportunistic screening for AF by pulse taking
or ECG rhythm strip is recommended in
patients >_65 years of age.
188,211,223,225
IB
It is recommended to interrogate pacemakers
and implantable cardioverter defibrillators on a
regular basis for AHRE.
c224,226
IB
When screening for AF it is recommended
that:
217,218
•
The individuals undergoing screening are
informed about the significance and treatment
implications of detecting AF.
•
A structured referral platform is organized for
screen-positive cases for further physician-led
clinical evaluation to confirm the diagnosis of
AF and provide optimal management of
patients with confirmed AF.
•
Definite diagnosis of AF in screen-positive
cases is established only after physician
reviews the single-lead ECG recording of
>_30 s or 12-lead ECG and confirms that it
shows AF.
IB
Systematic ECG screening should be considered
to detect AF in individuals aged >_75 years, or
those at high risk of stroke.
212,224,227
IIa B
AF = atrial fibrillation; AHRE = atrial high-rate episode; ECG =
electrocardiogram.
a
Class of recommendation.
b
Level of evidence.
c
See sections 3.2 and 3.3 for diagnostic criteria for AF and AHRE, and section 16
for the management of patients with AHRE.
ESC Guidelines 23

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Non-invasive, multimodality imaging can provide all needed informa-
tion (Figure 9).
249,250
In selected patients, transoesophageal echocardiography (TOE)
can be used to evaluate valvular heart disease (VHD) or left atrial
appendage (LAA) thrombus; CT coronary angiography can be
performed for assessment of CAD; CT/MRI of the brain can be per-
formed when stroke is suspected. Specific predictors of stroke have
been suggested: LA dilation, spontaneous LA contrast, reduced LA
strain, LAA thrombus, low peak LAA velocity (<20 cm/s), and LAA
non-chicken wing configuration (on CT).
250
©ESC 2020
Figure 8 Diagnostic work-up and follow-up in AF patients. AF = atrial fibrillation; BNP = B-type natriuretic peptide; CHA
2
DS
2
-VASc = Congestive heart
failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 65 - 74 years, Sex category (female); CAD = coronary artery disease;
CRP = C-reactive protein; CT = computed tomography; CTA = computed tomography angiography; cTnT-hs = high-sensitivity cardiac troponin T; ECG
= electrocardiogram; LAA = left atrial appendage; LGE-CMR = late gadolinium contrast-enhanced cardiac magnetic resonance; MRI = magnetic resonance
imaging; NT-ProBNP = N-terminal (NT)-prohormone B-type natriuretic peptide.
Table 6 EHRA symptom scale
Score Symptoms Description
1 None AF does not cause any symptoms
2a Mild Normal daily activity not affected by symptoms related to AF
2b Moderate Normal daily activity not affected by symptoms related to AF, but patient troubled by symptoms
3 Severe Normal daily activity affected by symptoms related to AF
4 Disabling Normal daily activity discontinued
Six symptoms, including palpitations, fatigue, dizziness, dyspnoea, chest pain, and anxiety during AF, are evaluated with regard to how it affects the patient’s daily activity, ranging
from none to symptom frequency or severity that leads to a discontinuation of daily activities.
To measure treatment effects, QoL and symptom questionnaires should be sensitive to changes in AF burden. The EHRA symptom scale is a physician-assessed tool for quanti-
fication of AF-related symptoms that is used to guide symptom-driven AF treatment decisions,
228
and has been related to adverse outcomes in more symptomatic patients
(score 3 - 4) versus those with a score of 1 - 2.
228,230
However, it does not consider the symptom dimensions such as anxiety, treatment concerns, and medication adverse
effects that are captured by general QoL scales,
230
or the patient-reported symptom-related outcomes. As discrepancies between patient-reported and physician-assessed out-
comes are frequently observed,
231
the AF-related treatment decisions also need to be informed by a quantified patient perception of symptoms, but further research is needed
to identify optimal tool(s) for capturing this information.
AF = atrial fibrillation; EHRA = European Heart Rhythm Association; QoL = quality of life.
24 ESC Guidelines

©ESC 2020
Figure 9 Imaging in AF. Anatomical imaging provides the LA size, shape, and fibrosis. Most accurate assessment of LA dilation is obtained by CMR or
CT. For routine assessment, two-dimensional (2D) or (preferably) three-dimensional (3D) transthoracic echocardiography is used. The 3D echocardio-
graphic normal volume values are 15 - 42 mL/m
2
for men and 15 - 39 mL/m
2
for women.
250
Assessment of LA fibrosis with LGE-CMR has been described
but only rarely applied in clinical practice.
251
Functional imaging includes TDI and strain. TDI measures the velocities of the myocardium in diastole and sys-
tole, whereas LA strain reflects active LA contraction. The PA-TDI interval reflects the atrial electromechanical delay (total LA conduction time, the time
interval between the P-wave on the ECG and the A’ [atrial peak velocity] on TDI) and reflects LA strain.
252
LA wall infiltration by epicardial fat is a potential
early marker of inflammation and can be detected with CT or cardiac MRI.
253
Before AF ablation, the pulmonary vein anatomy can be visualized with CT
or CMR. AF = atrial fibrillation; CT = computed tomography; EP = electrophysiology; LA = left atrium; LAA = left atrial appendage; LV = left ventricular;
LGE-CMR = late gadolinium contrast-enhanced cardiac magnetic resonance; MRI = magnetic resonance imaging; TDI = tissue doppler imaging; TOE =
transoesophageal echocardiography; TTE = transthoracic echocardiography.
Recommendations for diagnostic evaluation of patients with AF
Recommendation Class
a
Level
b
In patients with AF, it is recommended to:
•
Evaluate AF-related symptoms (including fatigue, tiredness, exertional shortness of breath, palpitations, and chest pain) and
quantify the patient symptom status using the modified EHRA symptom scale before and after initiation of treatment.
230,232
•
Evaluate AF-related symptoms before and after cardioversion of persistent AF to aid rhythm control treatment
decisions.
230,232
IC
AF = atrial fibrillation; EHRA = European Heart Rhythm Association.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 25

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
9 Integrated management of
patients with atrial fibrillation
9.1 Definitions and components of
integrated management of atrial
fibrillation patients
Integrated management of AF patients requires a coordinated and
agreed patient-individualized care pathway to deliver optimized treat-
ment (Figure 10) by an interdisciplinary team (Figure 11). Central to
this approach is the patient; treatment options should be discussed,
and the management plan agreed in discussion with healthcare pro-
fessionals. Treatment is subject to change over time with the devel-
opment of new risk factors, symptoms, disease progression, and the
advent of new treatments.
9.2 Multidisciplinary atrial fibrillation
teams
Integrated AF management requires a coordinated multidisciplinary
team (Figure 11) composed according to individual patient needs and
local availability of services. Complex patients would benefit from a
multidisciplinary team that includes relevant specialists, as well as
their primary care physician (for post-discharge care) and their fam-
ily/carer. Involvement of patient and family/carers is integral to the
success of AF management.
9.2.1 Role of healthcare systems and budget constraints
Optimized AF treatment requires a well-structured healthcare sys-
tem and significant financial resources.
254
Allocation of resources will
vary due to differing healthcare system structures and budget con-
straints in diverse geographies. The significant inequalities in the
access to AF management-related resources are documented in the
recent ESC Atlas on Cardiovascular Disease.
255
It is important to
consider optimizing use of available resources to reduce stroke,
improve symptoms, and treat comorbidities.
9.3 Patient involvement and shared
decision making
9.3.1 Patient values and preferences
Exploring patient’s values, goals, and preferences should be the first
step of shared decision making.
256,257
Qualitative research demon-
strates recurring discordance between caregivers reporting shared
decision making and patients experiencing a paternalistic mod-
el,
109,258261
and a misperception that many prefer not to be
involved in decision making, rather deferring to their phys-
ician.
259,262266
For shared decision making,
261
the importance
attached by the patient to stroke prevention and rhythm control and
the respective risk of death, stroke, and major bleeding, as well as the
burden of treatment, should be thoroughly assessed and
respected.
257,264,266268
©ESC 2020
Figure 10 Components of integrated AF management. AF = atrial fibrillation; HCP = healthcare professional; MDT = multidisciplinary team.
26 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
9.3.2 Patient education
Patient knowledge about AF and its management is often limit-
ed
257,269272
particularly when first diagnosed, when the majority of
treatment decisions are discussed and made.
Information on useful resources to help educate AF patients
273
can be found in the ESC Textbook of Cardiovascular Medicine,butedu-
cation alone is often insufficient to produce and maintain medication
adherence and lifestyle modifications.
9.4 Healthcare professional education
A mixed-methods approach has been used when targeting health-
care professionals including individual needs assessment followed
by bespoke education and training, whether by smart technology,
online resources, or upskilling face-to-face workshops or a combi-
nation.
274
The mAFA, integrating clinical-decision support and
education for healthcare professionals, has been successfully
piloted and subsequently tested in an outcome RCT.
275
Education
alone is insufficient to change healthcare-professional behav-
iour.
276
In the Integrated Management Program Advancing
Community Treatment of Atrial Fibrillation (IMPACT-AF) trial,
277
a multifaceted educational intervention including healthcare-
professional education and feedback resulted in a significant
increase in the proportion of patients treated with oral anticoagu-
lant (OAC) therapy.
9.5 Adherence to treatment
Factors affecting adherence to treatment can be grouped into patient-
related (e.g. demographics, comorbidities, cognitive impairment,
polypharmacy, treatment side-effects, psychological health, patient
understanding of the treatment regimen), physician-related (knowl-
edge, awareness of guidelines, expertise, multidisciplinary team
approach), and healthcare system-related (work-setting, access to
treatments, cost) factors.
278
Ensuring patients are appropriately informed about treatment
options, how to adhere to treatment, potential consequences of
non-adherence, in addition to managing patient’s expectations of
treatment goals, are crucial to promote adherence. Regular review
by any member of the multidisciplinary team is important to identify
non-adherence and implement strategies to improve adherence
where appropriate.
9.6 Technology tools supporting atrial
fibrillation management
Clinical decision support systems are intelligent systems that digitize
and provide evidence-based guidelines, clinical pathways, and algo-
rithms facilitating personalized, timely, and evidence-based
treatment.
The MobiGuide project
279
and several applications
280283
(Supplementa ry Tables 5 and 6) have been used to enhance patient
©ESC 2020
Figure 11 Integrated AF management team (an example). The figure gives an example on the potential composition of AF teams showing a variety of
different specialists supporting individual patients as needed. AF = atrial fibrillation.
a
According to local standards, this could be a general cardiologist with
special interest in arrhythmias/AF or an electrophysiologist.
ESC Guidelines 27

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
education, improve communication between patients and healthcare
professionals, and encourage active patient involvement. The ESC/
CATCH-ME (Characterizing AF by Translating its Causes into Health
Modifiers in the Elderly) consortium also has a smartphone/tablet
app
281
for AF patients, but this is yet to be tested prospectively. A
Cochrane review
284
demonstrated that patient decision-support aids
reduce decision conflict.
285288
Nevertheless, contradictory
results
277,289,290
illustrate the need for more carefully designed stud-
ies, including assessment of the intervention’s effect on clinical events.
9.7 Advantages of integrated
management of atrial fibrillation patients
Limited evidence exists on the effectiveness of integrated manage-
ment of AF. Available intervention studies vary widely in number and
content of ‘integrated care’ employed. Six studies—one cluster
RCT,
291
four RCTs,
277,292295
and one before-and-after study
294
—
of integrated AF management have demonstrated mixed findings
(Supplementary Table 7). Two studies
292,294
and one meta-analysis
296
report significantly lower rates of cardiovascular hospitalization and
death with nurse-led, integrated care, whereas others reported no
effect of integrated care on these outcomes. One multifaceted
study
277
demonstrated improved OAC rates in the intervention
group at 12 months. The IMPACT-AF study
277
found no significant
difference in the composite efficacy outcome (unplanned emergency
department visit or cardiovascular hospitalization) or the primary
safety outcome of major bleeding between intervention and usual
care.
9.8 Measures (or approaches) for
implementation of integrated
management
Integrated management of AF requires a change in the current
approach to patient care, to focus on moving from a multidisciplinary
team to interdisciplinary working, including behaviour change for all
AF team members and key stakeholders including patients and their
family
297,298
(Supplementary Figure 3).
To understand whether integrated AF management has been
implemented into clinical practice and had an impact on important
outcomes (mortality, stroke, hospitalization, QoL, symptom reduc-
tion, etc.), a specific international standard set of outcome measures
should be collected (Supplementary Figure 4).
299
This would also high-
light areas requiring further development.
9.9 Treatment burden
Patient-perceived treatment burden
300
is defined as the workload
imposed by healthcare on patients and its effect on patient function-
ing and well-being apart from specific treatment side-effects.
301,302
It
includes everything patients do for their health (drug management,
self-monitoring, visits to the doctor, laboratory tests, lifestyle
changes) and healthcare impact on their social relationships, poten-
tially affecting adherence to treatment,
303,304
QoL, and outcomes
(e.g. hospitalization and survival).
305,306
Patient-perceived treatment
burden is influenced by their knowledge about disease.
302
Patients
with similar treatment regimens may have very different treatment
burden,
307
with only a weak agreement between patient’s and physi-
cians’ treatment burden evaluation, suggesting that the patient’s
experience is not shared in depth during consultations.
302,308,309
Treatment burden can be overwhelming for patients with multi-
ple chronic conditions
301
(e.g. those with three chronic conditions
would have to take 6 - 12 medications daily, visit a healthcare giver
1.2 - 5.9 times per month, and spend 49.6 - 71.0 h monthly in
healthcare-related activities
310
). Treatment burden in AF patients
is largely unknown. In a single-centre prospective study, AF
patient-perceived total treatment burden was higher than in
patients with other chronic conditions (27.6% vs. 24.3%, P =0.011),
and 1 in 5 AF patients reported a high treatment burden that could
question the sustainability of their treatment. Notably, AF patients
attributed the highest proportion of treatment burden to health-
care system-related aspects (e.g. attending appointments etc.) and
lifestyle modification requirements. Female sex and younger age
were independently significantly associated with a higher treat-
ment burden, whereas non-vitamin K antagonist oral anticoagu-
lants (NOACs) and rhythm control reduced the odds for high
treatment burden by >50%.
311
The discussion of treatment burden should be an integral part of
shared, informed treatment decision making, and treatment burden
can be assessed using a validated questionnaire.
312
9.10 Patient-reported outcomes
There is increasing advocacy for including patient-reported outcomes
(PROs) as endpoints in clinical trials
313
and their routine
collection
314316
to improve care and assess treatment success from
the patient’s perspective. Patients’ experience of AF and its manage-
ment is highly subjective; AF management has become increasingly
complex, potentially resulting in significant treatment burden and
poorer health-related QoL.
Measuring outcomes that are important to patients, in addition to
‘hard’ clinical endpoints (death, stroke, major bleeding, etc.), can
inform AF management. An international consortium of AF patients
and healthcare professionals has identified the following PROs as
important to measure for AF: health-related QoL, physical and emo-
tional functioning, cognitive function, symptom severity, exercise tol-
erance, and ability to work (Supplem entary Figure 4)
299
;PRO
measures can be used to assess these factors and the international
standard set of AF outcome measures proposes some tools for
assessing PROs.
299
Health informatics systems could help capture
PRO data. Despite increasing support for the role of PRO measures
in healthcare management, few studies and registries report collect-
ing PRO data using validated tools.
313
Implementation of PRO meas-
ures in the management of AF patients is addressed in a dedicated
expert consensus paper developed in collaboration with patient rep-
resentatives by the EHRA.
317
28 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
10 Patient management: the
integrated ABC pathway
The simple Atrial fibrillation Better Care (ABC) holistic pathway (’A’
Anticoagulation/Avoid stroke; ‘B’ Better symptom management; ‘C’
Cardiovascular and Comorbidity optimization
318
) streamlines inte-
grated care of AF patients across all healthcare levels and among dif-
ferent specialties. Compared with usual care, implementation of the
ABC pathway has been significantly associated with lower risk of all-
cause death, composite outcome of stroke/major bleeding/cardiovas-
cular death and first hospitalization,
319
lower rates of cardiovascular
events,
320,321
and lower health-related costs.
322
In the prospective,
randomized mAFA-II trial, the composite outcome was significantly
lowered with ABC pathway management intervention compared
with usual care [1.9% vs. 6.0%; hazard ratio (HR) 0.39; 95% CI
0.22 - 0.67; P <0.001].
323
10. 1 ‘A’ Anticoagulation/Avoid stroke
This section refers to AF in the absence of severe mitral stenosis or
prosthetic heart valves (for AF with concomitant VHD see section
11.7).
148
10.1.1 Stroke risk assessment
Overall, AF increases the risk of stroke five-fold, but this risk is not
homogeneous, depending on the presence of specific stroke risk fac-
tors/modifiers. Main clinical stroke risk factors have been identified
from non-anticoagulated arms of the historical RCTs conducted >20
years ago, notwithstanding that these trials only randomized <10% of
patients screened, whereas many common risk factors were not
recorded or consistently defined.
324
These data have been supple-
mented by evidence from large observational cohorts also studying
patients who would not have been included in the RCTs.
Subsequently, various imaging, blood, and urine biological markers
(biomarkers) have been associated with stroke risk (Table 7).
324,325
In
addition, non-paroxysmal AF is associated with an increase in
thrombo-embolism (multivariable adjusted HR 1.38; 95% CI
1.19 - 1.61; P <0.001) compared with paroxysmal AF.
156
Notably,
many of the risk factors for AF-related complications are also risk fac-
tors for incident AF.
33
Common stroke risk factors are summarized in the clinical risk-fac-
tor-based CHA
2
DS
2
-VASc [Congestive heart failure, Hypertension,
Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age
6574 years, Sex category (female)] score (Table 8).
334
Stroke risk scores have to balance simplicity and practicality against
precision.
354356
As any clinical risk-factor-based score, CHA
2
DS
2
-
VASc performs only modestly in predicting high-risk patients who
will sustain thrombo-embolic events, but those identified as low-risk
[CHA
2
DS
2
-VASc 0 (males), or score of 1 (females)] consistently
have low ischaemic stroke or mortality rates (<1%/year) and do not
need any stroke prevention treatment.
Female sex is an age-dependent stroke risk modifier rather than a
risk factor per se.
357,358
Observational studies showed that women
with no other risk factors (CHA
2
DS
2
-VASc score of 1) have a low
stroke risk, similar to men with a CHA
2
DS
2
-VASc score of 0.
359
The
simplified CHA
2
DS
2
-VA score could guide the initial decision about
OAC in AF patients, but not considering the sex component would
underestimate stroke risk in women with AF.
360,361
In the presence
of >1 non-sex stroke risk factor, women with AF consistently have
significantly higher stroke risk than men.
353,362
Many clinical stroke risk factors (e.g. renal impairment, OSA, LA
dilatation
291,326,363365
) are closely related to the CHA
2
DS
2
-VASc
components, and their consideration does not improve its predic-
tive value (the relationship of smoking or obesity to stroke risk in
AF is also contentious).
366
Various biomarkers [e.g. troponin,
natriuretic peptides, growth differentiation factor (GDF)-15, von
Willebrand factor] have shown improved performance of
biomarker-based over clinical scores in the assessment of residual
stroke risk among anticoagulated AF patients
329,367
; notwithstand-
ing, many of these biomarkers (as well as some clinical risk factors)
are predictive of both stroke and bleeding
329
or non-AF and non-
cardiovascular conditions, often (non-specifically) reflecting simply
a sick heart or patient.
More complex clinical scores [e.g. Global Anticoagulant Registry in
the FIELD - Atrial Fibrillation (GARFIELD-AF)]
368
and those inclusive
of biomarkers [e.g. Anticoagulation and Risk Factors in Atrial
Fibrillation (ATRIA),
369,370
Intermountain Risk Score,
371
ABC-stroke
(Age, Biomarkers, Clinical history)]
372
improve stroke risk prediction
modestly but statistically significantly. The ABC-stroke risk score that
considers age, previous stroke/transient ischaemic attack (TIA), high-
sensitivity troponin T (cTnT-hs) and N-terminal (NT)-prohormone
Recommendations about integrated AF management
Recommendations Class
a
Level
b
To optimize shared decision making about specific AF treatment option(s) in consideration, it is recommended that physicians:
•
Inform the patient about the advantages/limitations and benefit/risks associated with the treatment option(s) being considered;
and
•
Discuss the potential burden of the treatment with the patient and include the patient’s perception of treatment burden in the
treatment decision.
IC
It is recommended to routinely collect PROs to measure treatment success and improve patient care.
IC
Integrated management with a structured multidisciplinary approach including healthcare professionals, patients, and their family/
carers, should be used in all AF patients to improve clinical outcomes.
277,292294,296,297
IIa B
AF = atrial fibrillation; PRO = patient-reported outcome.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 29

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
B-type natriuretic peptide has been validated in the cohorts of land-
mark NOAC trials.
373375
A biomarker score-guided treatment
strategy to reduce stroke and mortality in AF patients is being eval-
uated in an ongoing RCT (the ABC-AF Study, NCT03753490).
Whereas the routine use of biomarker-based risk scores currently
would not substantially add to initial stroke prevention treatment
decisions in patients already qualifying for treatment based on the
CHA
2
DS
2
-VASc score (and a limited practicality would be accompa-
nied by increased healthcare costs),
355,376,377
biomarkers could fur-
ther refine stroke risk differentiation among patients initially classified
as low risk and those with a single non-sex CHA
2
DS
2
-VASc risk
factor.
378
Studies of the CHA
2
DS
2
-VASc score report a broad range of
stroke rates depending on study setting (community vs. hospital),
methodology (e.g. excluding patients subsequently treated with
OAC would bias stroke rates towards lower levels), ethnicity, and
prevalence of specific stroke risk factors in the study population (dif-
ferent risk factors carry different weight, and age thresholds for ini-
tiating NOACs may even differ for patients with a different single
non-sex stroke risk factor, as follows: age 35 years for HF, 50 years
for hypertension or diabetes, and 55 years for vascular disease).
379,380
No RCT has specifically addressed the need for OAC in patients with
a single non-sex CHA
2
DS
2
-VASc risk factor (to obtain high event
rates and timely complete the study, anticoagulation trials have pref-
erentially included high-risk patients), but an overview of subgroup
analyses and observational data suggests that OAC use in such
patients confers a positive net clinical benefit when balancing the
reduction in stroke against the potential for harm with serious
bleeding.
339,381
For many risk factors (e.g. age), stroke risk is a continuum rather
than an artificial low-, moderate-, or high-risk category. Risk factors
are dynamic and, given the elderly AF population with multiple (often
changing) comorbidities, stroke risk needs to be re-evaluated at each
clinical review. Recent studies have shown that patients with a change
in their risk profile are more likely to sustain strokes.
382,383
Many ini-
tially low-risk patients (>15%) would have >_1 non-sex CHA
2
DS
2
-
VASc risk factor at 1 year after incident AF,
384386
and 90% of new
comorbidities were evident at 4.4 months after AF was diagnosed.
387
A Patient-Centred Outcomes Research Institute (PCORI)-com-
missioned systematic review of 61 studies compared diagnostic accu-
racy and impact on clinical decision making of available clinical and
imaging tools and associated risk factors for predicting thrombo-
embolic and bleeding risk in AF patients.
388
The authors concluded
that the CHADS
2
(CHF history, Hypertension history, Age >_75 y,
Diabetes mellitus history, Stroke or TIA symptoms previously),
CHA
2
DS
2
-VASc, and ABC risk scores have the best evidence for
predicting thrombo-embolic risk (moderate strength of evidence for
limited prediction ability of each score).
10.1.2 Bleeding risk assessment
When initiating antithrombotic therapy, potential risk for bleeding
also needs to be assessed. Non-modifiable and partially modifiable
bleeding risks (Table 9) are important drivers of bleeding events in
synergy with modifiable factors.
389
Notably, a history of falls is not an
independent predictor of bleeding on OAC (a modelling study esti-
mated that a patient would need to fall 295 times per year for the
benefits of ischaemic stroke reduction with OAC to be outweighed
by the potential for serious bleeding).
390
Modifiable and non-modifiable bleeding risk factors have been
used to formulate various bleeding risk scores,
368,391395
generally
with a modest predictive ability for bleeding events.
396,397
Studies
comparing specific bleeding risk scores provided conflicting find-
ings.
393,394,398
Various biomarkers have been proposed as bleeding
risk predictors, but many have been studied in anticoagulated trial
cohorts (while bleeding risk assessment is needed at all parts of the
patient pathway—when initially not using OAC, if taking aspirin, and,
subsequently, on OAC). Additionally, biomarkers are non-specifically
predictive of stroke, death, HF, etc.
399,400
or even non-cardiovascular
conditions (e.g. glaucoma),
401
and the availability of some biomarkers
is limited in routine clinical practice.
The biomarker-based ABC-bleeding risk score [Age, Biomarkers
(GDF-15, cTnT-hs, haemoglobin) and Clinical history (prior
Table 7 Stroke risk factors in patients with AF
Most commonly studied
clinical risk factors
(a systematic review)
324
Positive
studies/All
studies
Other clinical risk
factors
325
Imaging
biomarkers
291,326328
Blood/urine
biomarkers
329332
Stroke/TIA/systemic embolism 15/16 Impaired renal function/
CKD
Echocardiography Cardiac troponin T and I
Natriuretic peptides
Cystatin C
Proteinuria
CrCl/eGFR
CRP
IL-6
GDF-15
von Willebrand factor
D-dimer
Hypertension 11/20 OSA LA dilatation
Spontaneous contrast or
thrombus in LA
Low LAA velocities
Complex aortic plaque
Ageing (per decade) 9/13 HCM
Structural heart disease 9/13 Amyloidosis in degenerative
cerebral and heart diseases
Diabetes mellitus 9/14 Hyperlipidaemia
Vascular disease 6/17 Smoking Cerebral imaging
CHF/LV dysfunction 7/18 Metabolic syndrome
333
Small-vessel disease
Sex category (female) 8/22 Malignancy
CHF = congestive heart failure; CKD = chronic kidney disease; CrCl = creatinine clearance; CRP = C-reactive protein; eGFR = estimated glomerular filtration rate; GDF-15 =
growth differentiation factor-15; IL-6 = interleukin 6; LA = left atrium; LAA = left atrial appendage; LV = left ventricular; OSA = obstructive sleep apnoea; TIA = transient
ischaemic attack.
30 ESC Guidelines

Table 8 CHA
2
DS
2
-VASc score
334
CHA
2
DS
2
-VASc score
Risk factors and definitions Points
awarded
Comment
C Congestive heart failure
Clinical HF, or objective evi-
dence of moderate to severe
LV dysfunction, or HCM
1 Recent decompensated HF irrespective of LVEF (thus incorporating HFrEF or HFpEF), or the
presence (even if asymptomatic) of moderate-severe LV systolic impairment on cardiac imag-
ing
335
; HCM confers a high stroke risk
336
and OAC is beneficial for stroke reduction.
337
H Hypertension
or on antihypertensive therapy
1 History of hypertension may result in vascular changes that predispose to stroke, and a well-
controlled BP today may not be well-controlled over time.
324
Uncontrolled BP - the optimal BP
target associated with the lowest risk of ischaemic stroke, death, and other cardiovascular out-
comes is 120 - 129/<80 mmHg.
338
A Age 75 years or older 2 Age is a powerful driver of stroke risk, and most population cohorts show that the risk rises
from age 65 years upwards.
339
Age-related risk is a continuum, but for reasons of simplicity and
practicality, 1 point is given for age 65 - 74 years and 2 points for age >_75 years.
D Diabetes mellitus
Treatment with oral hypogly-
caemic drugs and/or insulin or
fasting blood glucose
>125 mg/dL (7 mmol/L)
1 Diabetes mellitus is a well-established risk factor for stroke, and more recently stroke risk has
been related to duration of diabetes mellitus (the longer the duration of diabetes mellitus, the
higher the risk of thromboembolism
340
) and presence of diabetic target organ damage, e.g. retin-
opathy.
341
Both type 1 and type 2 diabetes mellitus confer broadly similar thromboembolic risk
in AF, although the risk may be slightly higher in patients aged <65 years with type 2 diabetes
mellitus compared to patients with type 1 diabetes mellitus.
342
S StrokePrevious stroke, TIA, or
thromboembolism
2 Previous stroke, systemic embolism, or TIA confers a particularly high risk of ischaemic stroke,
hence weighted 2 points. Although excluded from RCTs, AF patients with ICH (including hae-
morrhagic stroke) are at very high risk of subsequent ischaemic stroke, and recent observational
studies suggest that such patients would benefit from oral anticoagulation.
343345
V Vascular disease
Angiographically significant
CAD, previous myocardial
infarction, PAD, or aortic
plaque
1 Vascular disease (PAD or myocardial infarction) confers a 17 - 22% excess risk, particularly in
Asian patients.
346348
Angiographically significant CAD is also an independent risk factor for
ischaemic stroke among AF patients (adjusted incidence rate ratio 1.29, 95% CI 1.08 - 1.53).
349
Complex aortic plaque on the descending aorta, as an indicator of significant vascular disease, is
also a strong predictor of ischaemic stroke.
350
A Age 65 2 74 years 1 See above. Recent data from Asia suggest that the risk of stroke may rise from age 50 - 55 years
upwards and that a modified CHA
2
DS
2
-VASc score may be used in Asian patients.
351,352
Sc Sex category (female) 1 A stroke risk modifier rather than a risk factor.
353
Maximum score 9
AF = atrial fibrillation; BP = blood pressure; CAD = coronary artery disease; CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus,
Stroke, Vascular disease, Age 65-74 years, Sex category (female); CI = confidence interval; EF = ejection fraction; HCM = hypertrophic cardiomyopathy; HF = heart failure;
HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction; ICH = intracranial haemorrhage; LV = left ventricular; LVEF = left
ventricular ejection fraction; OAC = oral anticoagulant; PAD = peripheral artery disease; RCT = randomized controlled trial; TIA = transient ischaemic attack.
Table 9 Risk factors for bleeding with OAC and antiplatelet therapy
Non-modifiable Potentially modifiable Modifiable Biomarkers
Age >65 years
Previous major bleeding
Severe renal impairment (on dialysis or renal
transplant)
Severe hepatic dysfunction (cirrhosis)
Malignancy
Genetic factors (e.g. CYP 2C9 polymor-
phisms)
Previous stroke, small-vessel disease, etc.
Diabetes mellitus
Cognitive impairment/dementia
Extreme frailty ± excessive risk of
falls
a
Anaemia
Reduced platelet count or function
Renal impairment with CrCl <60
mL/min
VKA management strategy
b
Hypertension/elevated SBP
Concomitant antiplatelet/NSAID
Excessive alcohol intake
Non-adherence to OAC
Hazardous hobbies/occupations
Bridging therapy with heparin
INR control (target 2.0 - 3.0), target
TTR >70%
c
Appropriate choice of OAC and
correct dosing
d
GDF-15
Cystatin C/CKD-EPI
cTnT-hs
von Willebrand factor (þ
other coagulation markers)
CKD-EPI= Chronic Kidney Disease Epidemiology Collaboration; CrCl = creatinine clearance; cTnT-hs = high-sensitivity troponin T; CYP = cytochrome P; GDF-15 = growth
differentiation factor-15; INR = international normalized ratio; NSAID = non-steroidal anti-inflammatory drug; OAC = oral anticoagulant; SBP = systolic blood pressure; TTR =
time in therapeutic range; VKA = vitamin K antagonist.
a
Walking aids; appropriate footwear; home review to remove trip hazards; neurological assessment where appropriate.
b
Increased INR monitoring, dedicated OAC clinicals, self-monitoring/self-management, educational/behavioural interventions.
c
For patients receiving VKA treatment.
d
Dose adaptation based on patient’s age, body weight, and serum creatinine level.
ESC Guidelines 31

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
bleeding)]
375,402
reportedly outperformed clinical scores, but in
another study there was no long-term advantage of ABC-bleeding
over HAS-BLED score (Table 10), whereas HAS-BLED was better in
identifying patients at low risk of bleeding (HAS-BLED 0 - 2).
403
In the
PCORI-commissioned systematic review,
388
encompassing 38 stud-
ies of bleeding risk prediction, the HAS-BLED score had the best evi-
dence for predicting bleeding risk (moderate strength of evidence),
consistent with other systematic reviews and meta-analyses compar-
ing bleeding risk prediction approaches.
404406
A high bleeding risk score should not lead to withholding OAC, as
the net clinical benefit of OAC is even greater amongst such patients.
However, the formal assessment of bleeding risk informs manage-
ment of patients taking OAC, focusing attention on modifiable bleed-
ing risk factors that should be managed and (re)assessed at every
patient contact, and identifying high-risk patients with non-modifiable
bleeding risk factors who should be reviewed earlier (for instance in
4 weeks rather than 4 - 6 months) and more frequently.
389,407
Identification of ‘high bleeding risk’ patients is also needed when
determining the antithrombotic strategy in specific AF patient groups,
such as those undergoing percutaneous coronary intervention (PCI).
Overall, bleeding risk assessment based solely on modifiable bleed-
ing risk factors is an inferior strategy compared with formal bleeding
risk assessment using a bleeding risk score,
408410
thus also consider-
ing the interaction between modifiable and non-modifiable bleeding
risk factors. Bleeding risk is dynamic, and attention to the change in
bleeding risk profile is a stronger predictor of major bleeding events
compared with simply relying on baseline bleeding risk. In a recent
study, there was a 3.5-fold higher risk of major bleeding in the first 3
months amongst patients who had a change in their bleeding risk
profile.
389
In the mAFA-II trial, prospective dynamic monitoring and reassess-
ment using the HAS-BLED score (together with holistic App-based man-
agement) was associated with fewer major bleeding events, mitigated
modifiable bleeding risk factors, and increased OAC uptake; in contrast,
bleeding rates were higher and OAC use overall decreased by 25% in
the ‘usual care’ arm when comparing baseline with 12 months.
411
10.1.3 Absolute contraindications to oral anticoagulants
The few absolute contraindications to OAC include active serious
bleeding (where the source should be identified and treated), associ-
ated comorbidities (e.g. severe thrombocytopenia <50 platelets/lL,
severe anaemia under investigation, etc.), or a recent high-risk bleed-
ing event such as intracranial haemorrhage (ICH). Non-drug options
may be considered in such cases (section 11.4.3).
10.1.4 Stroke prevention therapies
10.1.4.1 Vitamin K antagonists
Compared with control or placebo, vitamin K antagonist (VKA) ther-
apy (mostly warfarin) reduces stroke risk by 64% and mortality by
26%,
412
and is still used in many AF patients worldwide. VKAs are
currently the only treatment with established safety in AF patients
with rheumatic mitral valve disease and/or an artificial heart valve.
The use of VKAs is limited by the narrow therapeutic interval, necessi-
tating frequent international normalized ratio (INR) monitoring and dose
adjustments.
413
At adequate time in therapeutic range [(TTR) >70%],
VKAs are effective and relatively safe drugs. Quality of VKA management
(quantified using the TTR based on the Rosendaal method, or the per-
centage of INRs in range) correlates with haemorrhagic and thrombo-
............................................. ........................................................................... ..........................................
Table 10 Clinical risk factors in the HAS-BLED score
395
Risk factors and definitions Points awarded
H Uncontrolled hypertension
SBP >160 mmHg
1
A Abnormal renal and/or hepatic function
Dialysis, transplant, serum creatinine >200 mmol/L, cirrhosis, bilirubin > 2 upper limit of normal,
AST/ALT/ALP >3 upper limit of normal
1 point for each
S Stroke
Previous ischaemic or haemorrhagic
a
stroke
1
B Bleeding history or predisposition
Previous major haemorrhage or anaemia or severe thrombocytopenia
1
L Labile INR
b
TTR <60% in patient receiving VKA
1
E Elderly
Aged >65 years or extreme frailty
1
D Drugs or excessive alcohol drinking
Concomitant use of antiplatelet or NSAID; and/or excessive
c
alcohol per week
1 point for each
Maximum score 9
ALP = alkaline phosphatase; ALT = alanine aminotransferase; AST = aspartate aminotransferase; SBP = systolic blood pressure; INR = international normalized ratio; NSAID =
Non-steroidal anti-inflammatory drug; TTR = time in therapeutic range; VKA = vitamin K antagonist.
a
Haemorrhagic stroke would also score 1 point under the ‘B’ criterion.
b
Only relevant if patient receiving a VKA.
c
Alcohol excess or abuse refers to a high intake (e.g. >14 units per week), where the clinician assesses there would be an impact on health or bleeding risk.
32 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
embolic rates.
414
At high TTR values, the efficacy of VKAs in stroke pre-
vention may be similar to NOACs, whereas the relative safety benefit
with NOACs is less affected by TTR, with consistently lower serious
bleeding rates (e.g. ICH) seen with NOACs compared with warfarin,
notwithstanding that the absolute difference is small.
415,416
Numerous factors (including genetics, concomitant drugs, etc.) influ-
ence the intensity of VKA anticoagulant effect; the more common ones
have been used to derive and validate the SAMe-TT
2
R
2
fSex [female],
Age [<60 years], Medical history of >_2 comorbidities [hypertension,
diabetes mellitus, CAD/myocardial infarction, peripheral artery disease
(PAD), HF, previous stroke, pulmonary disease, and hepatic or renal dis-
ease], Treatment [interacting drugs, e.g. amiodarone], Tobacco use,
Race [non-Caucasian]g score,
417
which can help to identify patients
who are less likely to achieve a good TTR on VKA therapy (score >2)
and would do better with a NOAC. If such patients with SAMe-
TT
2
R
2
>2 are prescribed a VKA, greater efforts to improve TTR, such
as more intense regular reviews, education/counselling, and frequent
INR monitoring are needed or, more conveniently, the use of a NOAC
should be reconsidered.
418
10.1.4.2 Non-vitamin K antagonist oral anticoagulants
In four pivotal RCTs, apixaban, dabigatran, edoxaban, and rivaroxaban
have shown non-inferiority to warfarin in the prevention of stroke/sys-
temic embolism.
419422
In a meta-analysis of these RCTs, NOACs
were associated with a 19% significant stroke/systemic embolism risk
reduction, a 51% reduction in haemorrhagic stroke,
423
and similar
ischaemic stroke risk reduction compared with VKAs, but NOACs
were associated with a significant 10% reduction in all-cause mortality
(Sup plementary Table 8). There was a non-significant 14% reduction in
major bleeding risk, significant 52% reduction in ICH, and 25% increase
in gastrointestinal bleeding with NOACs vs. warfarin.
423
The major bleeding relative risk reduction with NOACs was signifi-
cantly greater when INR control was poor (i.e. centre-based
TTR<66%). A meta-analysis of the five NOAC trials [RE-LY
(Randomized Evaluation of Long Term Anticoagulant Therapy),
ROCKET-AF (Rivaroxaban Once Daily Oral Direct Factor Xa
Inhibition Compared with Vitamin K Antagonism for Prevention of
Stroke and Embolism Trial in Atrial Fibrillation), J-ROCKET AF,
ARISTOTLE (Apixaban for Reduction in Stroke and Other
Thromboembolic Events in Atrial Fibrillation), and ENGAGE AF TIMI
48 (Effective Anticoagulation with Factor Xa Next Generation in Atrial
FibrillationThrombolysis in Myocardial Infarction 48)] showed that,
compared with warfarin, standard-dose NOACs were more effective
and safer in Asians than in non-Asians.
424
In the AVERROES [Apixaban
Versus Acetylsalicylic Acid (ASA) to Prevent Stroke in Atrial
Fibrillation Patients Who Have Failed or Are Unsuitable for Vitamin K
Antagonist Treatment] trial of AF patients who refused or were
deemed ineligible for VKA therapy, apixaban 5 mg b.i.d. (twice a day)
significantly reduced the risk of stroke/systemic embolism with no sig-
nificant difference in major bleeding or ICH compared with aspirin.
425
Post-marketing observational data on the effectiveness and safety
of dabigatran,
426,427
rivaroxaban,
428,429
apixaban,
430
and edoxaban
431
vs. warfarin show general consistency with the respective RCT.
Given the compelling evidence about NOACs, AF patients should be
informed of this treatment option.
Persistence to NOAC therapy is generally higher than to VKAs,
being facilitated by a better pharmacokinetic profile of NOACs
432
(Supplementary Table 9) and favourable safety and efficacy, especially
amongst vulnerable patients including the elderly, those with renal
dysfunction or previous stroke, and so on.
433
Whereas patients with
end-stage renal dysfunction were excluded from the pivotal RCTs,
reduced dose regimens of rivaroxaban, edoxaban, and apixaban are
feasible options for severe CKD [creatinine clearance (CrCl)
15 - 30 mL/min using the Cockcroft-Gault equation].
434,435
Considering that inappropriate dose reductions are frequent in clini-
cal practice,
436
thus increasing the risks of stroke/systemic embolism,
hospitalization, and death, but without decreasing bleeding risk,
437
NOAC therapy should be optimized based on the efficacy and safety
profile of each NOAC in different patient subgroups (Table 11).
10.1.4.3 Other antithrombotic drugs
In the ACTIVE W (Atrial Fibrillation Clopidogrel Trial with Irbesartan
for Prevention of Vascular Events) trial, dual antiplatelet therapy
(DAPT) with aspirin and clopidogrel was less effective than warfarin
for prevention of stroke, systemic embolism, myocardial infarction,
and vascular death (the annual risk of events was 5.6% vs. 3.9%,
P =0.0003), with a similar rate of major bleeding.
438
In the ACTIVE-A
trial, patients unsuitable for anticoagulation had a lower rate of
thrombo-embolic complications when clopidogrel was added to
aspirin compared with aspirin alone, but with a significant increase in
major bleeding.
439
Aspirin monotherapy was ineffective for stroke
prevention compared with no antithrombotic treatment and was
Table 11 Dose selection criteria for NOACs
Dabigatran Rivaroxaban Apixaban Edoxaban
Standard dose 150 mg b.i.d. 20 mg o.d. 5 mg b.i.d. 60 mg o.d.
Lower dose 110 mg b.i.d. 30 mg o.d.
Reduced dose 15 mg o.d. 2.5 mg b.i.d. 30 mg o.d./15 mg o.d.
Dose-reduction
criteria
Dabigatran 110 mg b.i.d. in patients with:
•
Age >_80 years
•
Concomitant use of verapamil, or
•
Increased bleeding risk
CrCl 15 - 49 mL/min At least 2 of 3 criteria:
•
Age >_80 years,
•
Body weight <_60 kg, or
•
Serum creatinine
>_1.5 mg/dL (133 lmol/L)
If any of the following:
•
CrCl 30 - 50 mL/min,
•
Body weight <_60 kg,
•
Concomitant use of verapamil,
quinidine, or dronedarone
b.i.d. = bis in die (twice a day); CrCl = creatinine clearance; o.d. = omni die (once daily).
ESC Guidelines 33

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
associated with a higher risk of ischaemic stroke in elderly
patients.
440
Overall, antiplatelet monotherapy is ineffective for stroke preven-
tion and is potentially harmful, (especially amongst elderly AF
patients),
441,442
whereas DAPT is associated with a bleeding risk simi-
lar to OAC therapy. Hence, antiplatelet therapy should not be used
for stroke prevention in AF patients.
10.1.4.4 Combination therapy with oral anticoagulant and antiplatelet
drugs
The use of antiplatelet therapy remains common in clinical practice,
often in patients without an indication (e.g. PAD, CAD, or cerebro-
vascular disease) beyond AF.
443
There is limited evidence to support
the combination therapy solely for stroke prevention in AF, with no
effect on reductions in stroke, myocardial infarction, or death, but
with a substantial increase in the risk of major bleeding and
ICH.
441,442
10.1.4.5 Left atrial appendage occlusion and exclusion
10.1.4.5.1 Left atrial appendage occlusion devices. Only the
Watchman device has been compared with VKA therapy in RCTs
[the PROTECT AF (WATCHMAN Left Atrial Appendage System
for Embolic Protection in Patients With Atrial Fibrillation) and
PREVAIL (Watchman LAA Closure Device in Patients With Atrial
Fibrillation Versus Long Term Warfarin Therapy)],
444446
where
LAA occlusion was non-inferior to VKA stroke prevention treatment
in AF patients with moderate stroke risk, with a possibility of lower
bleeding rates on longer follow-up.
447
The LAA occlusion may also
reduce stroke risk in patients with contraindications to OAC.
448,449
A large European registry reported a high implantation success
rate (98%), with an acceptable procedure-related complication rate
of 4% at 30 days.
450
Nevertheless, the implantation procedure can
cause serious complications (higher event rates have been reported
in real-world analyses compared with industry-sponsored studies,
possibly identifying some reporting bias) and device-related throm-
bosis may not be a benign finding.
451454
Antithrombotic manage-
ment after LAA occlusion has never been evaluated in a randomized
manner and is based on historical studies, at least including aspirin
(Table 12). For patients who do not tolerate any antiplatelet therapy,
either an epicardial catheter approach (e.g. Lariat system) or thoraco-
scopic clipping of the LAA may be an option.
455,456
Notably, the non-inferiority of LAA occlusion to VKA treatment
was mostly driven by the prevention of haemorrhagic stroke, with a
trend for more ischaemic strokes. The limitations of LAA occlusion
as a strategy to reduce the risk of stroke associated with AF also
include the consideration that AF acts as a risk marker of stroke.
Withholding OAC after LAA occlusion is likely to result in under-
treating the overall risk of stroke related to atrial cardiomyopathy.
10.1.4.5.2 Surgical left atrial appendage occlusion or exclusion. Multiple
observational studies indicate the feasibility and safety of surgical LAA
occlusion/exclusion, but only limited controlled trial data are
available.
457459
Residual LAA flow or incomplete LAA occlusion
may be associated with an increased risk of stroke.
460
In most studies,
LAA occlusion/exclusion was performed during other open heart
surgery, and in more recent years in combination with surgical abla-
tion of AF
459,461
or as an isolated thoracoscopic procedure. A large
RCT in patients with an associated cardiac surgical procedure is
ongoing.
462
The most common justification for LAA occlusion/exclusion in
clinical practice is a perceived high bleeding risk or, less often, contra-
indications for OAC.
450
However, LAA occluders have not been ran-
domly tested in such populations. Most patients who some years ago
would be considered unsuitable for OAC therapy with VKA now
seem to do relatively well on NOAC,
433,463,464
and LAA occluders
have not been compared with NOAC therapy in patients at risk for
bleeding, or with surgical LAA occlusion/exclusion. Long-term aspirin
is a common strategy in these patients,
465
and one may question
whether a NOAC would not be a better strategy if aspirin is toler-
ated. There is the need for adequately powered trials to define the
best indications of LAA occlusion/exclusion compared with NOAC
therapy in patients with relative or absolute contraindications for
anticoagulation, in those suffering from an ischaemic stroke on anti-
coagulant therapy, and for assessment of the appropriate antithrom-
botic therapy after LAA occlusion.
Table 12 Antithrombotic therapy after left atrial appendage occlusion
Device/patient Aspirin OAC Clopidogrel Comments
Watchman/low
bleeding risk
75 - 325 mg/day
indefinitely
Start warfarin after procedure (tar-
get INR 2 - 3) until 45 days or con-
tinue until adequate LAA sealing is
confirmed
a
by TOE. NOAC is a
possible alternative
Start 75 mg/day when OAC
stopped, continue until 6 months
after the procedure
Some centres do not withhold
OAC at the time of procedure (no
data to support/deny this
approach)
Watchman/high
bleeding risk
75 - 325 mg/day
indefinitely
None 75 mg/day for 1 - 6 months while
ensuring adequate LAA sealing
a
Clopidogrel often given for shorter
time in very high-risk situations
ACP/Amulet 75 - 325 mg/day
indefinitely
None 75 mg/day for 1 - 6 months while
ensuring adequate LAA sealing
a
Clopidogrel may replace long-term
aspirin if better tolerated
ACP = Amplatzer
TM
Cardiac Plug; INR = international normalized ratio; LAA = left atrial appendage; LMWH = low-molecular-weight heparin; NOAC = non-vitamin K antago-
nist oral anticoagulant; OAC = oral anticoagulant ; TOE = transoesophageal echocardiography.
Note: Load aspirin or clopidogrel before procedure if untreated. Heparin with activated clotting time >250 seconds before or immediately after trans-septal punctures for all
patients, followed by LMWH when warfarin needed.
a
Less than 5 mm leak.
34 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
10.1.4.6 Long-term oral anticoagulation per atrial fibrillation burden
Although the risk of ischaemic stroke/systemic embolism is higher
with non-paroxysmal vs. paroxysmal AF, and AF progression is asso-
ciated with an excess of adverse outcomes,
169,466
the clinically deter-
mined temporal pattern of AF should not affect the decision
regarding long-term OAC, which is driven by the presence of stroke
risk factors.
156
Management of patients with AHRE/subclinical AF is
reviewed in section 16. Stroke risk in AHRE patients may be lower
than in patients with diagnosed AF,
467
and strokes often occur with-
out a clear temporal relationship with AHRE/subclinical AF,
179,226
underscoring its role as a risk marker rather than a stroke risk fac-
tor.
4,172
Whether AHRE and subclinical AF have the same therapeu-
tic requirements as clinical AF
7
is presently unclear, and the net
clinical benefit of OAC for AHRE/subclinical AF>24 h is currently
being studied in several RCTs.
4
Notably, patients with subclinical AF/AHRE may develop atrial
tachyarrhythmias lasting more than 24 h
468
or clinical AF; hence care-
ful monitoring of these patients is recommended, even considering
remote monitoring, especially with longer AHRE and higher risk pro-
file.
469
Given the dynamic nature of AF as well as stroke risk, a
recorded duration in one monitoring period would not necessarily
be the same in the next.
10.1.4.7 Long-term oral anticoagulation per symptom control strategy
Symptom control focuses on patient-centred and symptom-directed
approaches to rate or rhythm control. Again, symptom control strat-
egy should not affect the decision regarding long-term OAC, which is
driven by the presence of stroke risk factors, and not the estimated
success in maintaining sinus rhythm.
10.1.5 Management of anticoagulation-related bleeding
risk
10.1.5.1 Strategies to minimize the risk of bleeding
Ensuring good quality of VKA treatment (TTR>70%) and selecting the
appropriatedoseofaNOAC(asperthedosereductioncriteriaspeci-
fied on the respective drug label) are important considerations to mini-
mize bleeding risk. As discussed in se ctio n 10.1.2, attention to modifiable
bleeding risk factors should be made at every patient contact, and for-
mal bleeding risk assessment is needed to help identify high-risk patients
whoshouldbefolloweduporreviewedearlier(e.g.4weeksrather
than 4 - 6 months).
407
Concomitant regular administration of antiplate-
let drugs or non-steroidal anti-inflammatory drug (NSAID) should be
avoided in anticoagulated patients. Bleeding risk is dynamic, and
attention to the change in bleeding risk profile is a stronger predictor of
major bleeding events, especially in the first 3 months.
389
10.1.5.2 High-risk groups
Certain high-risk AF populations have been under-represented in
RCTs, including the extreme elderly (>_90 years), those with cognitive
impairment/dementia, recent bleeding or previous ICH, end-stage
renal failure, liver impairment, cancer, and so on. Observational data
suggest that such patients are at high risk for ischaemic stroke and
death, and many would benefit from OAC.
Patients with liver function abnormalities may be at higher risk of
bleeding on VKA, possibly less so on NOACs. Observational data in
cirrhotic patients suggest that ischaemic stroke reduction may out-
weigh bleeding risk.
470472
In patients with a recent bleeding event, attention should be
directed towards addressing the predisposing pathology (e.g. bleed-
ing ulcer or polyp in a patient with gastrointestinal bleeding), and the
reintroduction of OAC as soon as feasible, as part of a multidiscipli-
nary team decision. Consideration should be made for drugs such as
apixaban or dabigatran 110 mg b.i.d., which are not associated with
an excess of gastrointestinal bleeding compared with warfarin.
Where OAC is not reintroduced, there is a higher risk of stroke and
death compared with restarting OAC, although the risk of re-
bleeding may be higher.
473
Similarly, thromboprophylaxis in cancer
may require a multidisciplinary team decision balancing stroke reduc-
tion against serious bleeding, which may be dependent on cancer
type, site(s), staging, anti-cancer therapy and so on.
Thromboprophylaxis in specific high-risk groups is discussed in
detail throughout secti on 11.
10.1.6 Decision making to avoid stroke
In observational population cohorts, both stroke and death are rele-
vant endpoints, as some deaths could be due to fatal strokes (given
that endpoints are not adjudicated in population cohorts, and cere-
bral imaging or post-mortems are not mandated). As OAC signifi-
cantly reduces stroke (by 64%) and all-cause mortality (by 26%)
compared with control or placebo,
412
the endpoints of stroke and/or
mortality are relevant in relation to decision making for
thromboprophylaxis.
The threshold for initiating OAC for stroke prevention, balancing
ischaemic stroke reduction against the risk of ICH and associated
QoL, has been estimated to be 1.7%/year for warfarin and 0.9%/year
for a NOAC (dabigatran data were used for the modelling analy-
sis).
474
The threshold for warfarin may be even lower, if good-quality
anticoagulation control is achieved, with average TTR>70%.
475
Given the limitations of clinical risk scores, the dynamic nature of
stroke risk, the greater risk of stroke and death among AF patients
with >_1 non-sex stroke risk factor, and the positive net clinical ben-
efit of OAC among such patients, we recommend a risk-fac-
torbased approach to stroke prevention rather than undue focus
on (artificially defined) ‘high-risk’ patients. As the default is to offer
stroke prevention unless the patient is low risk, the CHA
2
DS
2
-
VASc score should be applied in a reductionist manner, to decide
on OAC or not.
476
Thus, the first step in decision making (‘A’ Anticoagulation/Avoid
stroke) is to identify low-risk patients who do not need antithrom-
botic therapy. Step 2 is to offer stroke prevention (i.e. OAC) to those
with >_1 non-sex stroke risk factors (the strength of evidence differs,
with multiple clinical trials for patients with >_2 stroke risk factors,
and subgroups from trials/observational data on patients with 1 non-
sex stroke risk factor). Step 3 is the choice of OAC—a NOAC (given
their relative effectiveness, safety and convenience, these drugs are
generally first choice as OAC for stroke prevention in AF) or VKA
(with good TTR at >70%). This ‘AF 3-step’ patient pathway
182,477
for
stroke risk stratification and treatment decision making is shown in
Figure 12.
ESC Guidelines 35

©ESC 2020
Figure 12 ‘A’ - Anticoagulation/Avoid stroke: The ‘AF 3-step’ pathway. AF = atrial fibrillation; CHA
2
DS
2
-VASc = Congestive heart failure,
Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 65 - 74 years, Sex category (female); HAS-BLED = Hypertension, Abnormal
renal/liver function, Stroke, Bleeding history or predisposition, Labile INR, Elderly (>65 years), Drugs/alcohol concomitantly; INR = international normal-
ized ratio; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagulant; SAMe-TT
2
R
2
= Sex (female), Age (<60 years), Medical history,
Treatment (interacting drug(s)), Tobacco use, Race (non-Caucasian) (score); TTR = time in therapeutic range; VKA = vitamin K antagonist.
a
If a VKA being considered, calculate SAMe-TT
2
R
2
score: if score 02, may consider VKA treatment (e.g. warfarin) or NOAC; if score >2, should arrange
regular review/frequent INR checks/ counselling for VKA users to help good anticoagulation control, or reconsider the use of NOAC instead; TTR ideally
>70%.
Recommendations for the prevention of thrombo-embolic events in AF
Recommendations Class
a
Level
b
For stroke prevention in AF patients who are eligible for OAC, NOACs are recommended in preference to VKAs (excluding
patients with mechanical heart valves or moderate-to-severe mitral stenosis).
423,424
IA
For stroke risk assessment, a risk-factor-based approach is recommended, using the CHA
2
DS
2
-VASc clinical stroke risk score to
initially identify patients at ‘low stroke risk’ (CHA
2
DS
2
-VASc score = 0 in men, or 1 in women) who should not be offered antith-
rombotic therapy.
334,388
IA
OAC is recommended for stroke prevention in AF patients with CHA
2
DS
2
-VASc score >_2 in men or >_3 in women.
412
IA
OAC should be considered for stroke prevention in AF patients with a CHA
2
DS
2
-VASc score of 1 in men or 2 in women.
Treatment should be individualized based on net clinical benefit and consideration of patient values and preferences.
338,378,380
IIa B
For bleeding risk assessment, a formal structured risk-score-based bleeding risk assessment is recommended to help identify non-
modifiable and address modifiable bleeding risk factors in all AF patients, and to identify patients potentially at high risk of bleeding
who should be scheduled for early and more frequent clinical review and follow-up.
388,395,404,406
IB
Continued
36 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
10.2 ‘B’ Better symptom control
10.2.1 Rate control
Rate control is an integral part of AF management, and is often suffi-
cient to improve AF-related symptoms. Very little robust evidence
exists to inform the best type and intensity of rate control
treatment.
484486
10.2.1.1 Target/optimal ventricular rate range
The optimal heart-rate target in AF patients is unclear. In the RACE
(Race Control Efficacy in Permanent Atrial Fibrillation) II RCT of per-
manent AF patients, there was no difference in a composite of clinical
events, New York Heart Association (NYHA) class, or hospitaliza-
tions between the strict [target heart rate <80 beats per minute
(bpm) at rest and <110 bpm during moderate exercise] and lenient
(heart-rate target <110 bpm) arm,
487,488
similar to an analysis from
the AFFIRM (Atrial Fibrillation Follow-up Investigation of Rhythm
Management) and RACE trials.
489
Therefore, lenient rate control is
an acceptable initial approach, regardless of HF status (with the
exception of tachycardia-induced cardiomyopathy), unless symptoms
call for stricter rate control (Figure 13).
10.2.1.2 Drugs
Pharmacological rate control can be achieved with beta-blockers,
digoxin, diltiazem, and verapamil, or combination therapy (Table 13).
Some antiarrhythmic drugs (AADs) also have rate-limiting properties
(e.g. amiodarone, dronedarone, sotalol) but generally they should be
used only for rhythm control. The choice of rate control drugs
depends on symptoms, comorbidities, and potential side-effects
(Table 13).
Beta-blockers are often first-line rate-controlling agents, largely
based on better acute rate control. Interestingly, the prognostic ben-
efit of beta-blockers seen in HF with reduced ejection fraction
(HFrEF) patients with sinus rhythm has been questioned in patients
with AF.
491
Non-dihydropyridine calcium channel blockers (NDCC)
verapamil and diltiazem provide reasonable rate control
492
and
can improve AF-related symptoms
486
compared with beta-
blockers. In one small trial of patients with preserved LVEF, NDCC
preserved exercise capacity and reduced B-type natriuretic
peptide.
493,494
Digoxin and digitoxin are not effective in patients with increased
sympathetic drive. Observational studies have associated digoxin use
with excess mortality in AF patients.
495497
This finding was likely
due to selection and prescription biases rather than harm caused by
digoxin,
498501
particularly as digoxin is commonly prescribed to
sicker patients.
502
Lower doses of digoxin may be associated with
For a formal risk-score-based assessment of bleeding risk, the HAS-BLED score should be considered to help address modifiable
bleeding risk factors, and to identify patients at high risk of bleeding (HAS-BLED score >_3) for early and more frequent clinical
review and follow-up.
388,395,404,406
IIa B
Stroke and bleeding risk reassessment at periodic intervals is recommended to inform treatment decisions (e.g. initiation of OAC
in patients no longer at low risk of stroke) and address potentially modifiable bleeding risk factors.
c389,478,479
IB
In patients with AF initially at low risk of stroke, first reassessment of stroke risk should be made at 4 - 6 months after the index
evaluation.
385387
IIa B
If a VKA is used, a target INR of 2.0 - 3.0 is recommended, with individual TTR>_70%.
414
IB
In patients on VKAs with low time in INR therapeutic range (e.g. TTR<70%), recommended options are:
•
Switching to a NOAC but ensuring good adherence and persistence with therapy
415,416
;or
IB
•
Efforts to improve TTR (e.g. education/counselling and more frequent INR checks).
480
IIa B
Antiplatelet therapy alone (monotherapy or aspirin in combination with clopidogrel) is not recommended for stroke prevention
in AF.
440,441,480,481
III A
Estimated bleeding risk, in the absence of absolute contraindications to OAC, should not in itself guide treatment decisions to use
OAC for stroke prevention.
III A
Clinical pattern of AF (i.e. first detected, paroxysmal, persistent, long-standing persistent, permanent) should not condition the
indication to thromboprophylaxis.
160
III B
Recommendations for occlusion or exclusion of the LAA
LAA occlusion may be considered for stroke prevention in patients with AF and contraindications for long-term anticoagulant
treatment (e.g. intracranial bleeding without a reversible cause).
448,449,481,482
IIb B
Surgical occlusion or exclusion of the LAA may be considered for stroke prevention in patients with AF undergoing cardiac
surgery.
459,483
IIb C
AF = atrial fibrillation; BP = blood pressure; CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 65 - 74
years, Sex category (female); HAS-BLED = Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile INR, Elderly (>65 years), Drugs/alco-
hol concomitantly; INR = international normalized ratio; LAA = left atrial appendage; NOAC = non-vitamin K antagonist oral anticoagulant; NSAID = non-steroidal anti-inflam-
matory drug; OAC = oral anticoagulant ; TTR = time in therapeutic range; VKA = vitamin K antagonist.
a
Class of recommendation.
b
Level of evidence.
c
Including uncontrolled BP; labile INRs (in a patient taking VKA); alcohol excess; concomitant use of NSAIDs or aspirin in an anticoagulated patient; bleeding tendency or predis-
position (e.g. treat gastric ulcer, optimize renal or liver function, etc.).
ESC Guidelines 37

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
better prognosis.
502
An ongoing RCT is addressing digitoxin use in
patients with HFrEF.
503
Amiodarone can be useful as a last resort when heart rate cannot
be controlled with combination therapy in patients who do not qual-
ify for non-pharmacological rate control, i.e. atrioventricular node
ablation and pacing, notwithstanding the extracardiac adverse effects
of the drug
504
(Table 13).
10.2.1.3 Acute rate control
In acute settings, physicians should always evaluate underlying causes,
such as infection or anaemia. Beta-blockers and diltiazem/verapamil
are preferred over digoxin because of their rapid onset of action and
effectiveness at high sympathetic tone.
507511
The choice of drug
(Table 13 and Figure 14) and target heart rate will depend on the
patient characteristics, symptoms, LVEF value, and haemodynamics,
but a lenient initial heart-rate approach seems acceptable (Figure 13).
Combination therapy may be required. In patients with HFrEF, beta-
blockers, digitalis, or their combination should be used.
512,513
In crit-
ically ill patients and those with severely impaired LV systolic function,
i.v. amiodarone can be used.
504,514,515
In unstable patients, urgent car-
dioversion should be considered (section 11.1).
10.2.1.4 Atrioventricular node ablation and pacing
Ablation of the atrioventricular node and pacemaker implantation
can control ventricular rate when medication fails. The procedure is
relatively simple and has a low complication rate and low long-term
mortality risk,
516,517
especially when the pacemaker is implanted a
few weeks before the atrioventricular node ablation and the initial
pacing rate after ablation is set at 7090 bpm.
518,519
The procedure
does not worsen LV function
520
and may even improve LVEF in
selected patients.
521523
Most studies have included older patients
with limited life expectancy. For younger patients, ablation of the
atrioventricular node should only be considered if there is urgent
need for rate control and all other pharmacological and non-
pharmacological treatment options have been carefully considered.
The choice of pacing therapy (right ventricular or biventricular pac-
ing) will depend on patient characteristics.
524,525
His-bundle pacing
after atrioventricular node ablation may evolve as an attractive alter-
native pacing mode,
526
as currently tested in ongoing clinical trials
(NCT02805465, NCT02700425).
In severely symptomatic patients with permanent AF and at
least one hospitalization for HF, atrioventricular node ablation
combined with cardiac resynchronization therapy (CRT) may be
preferred. In a small RCT, the primary composite outcome (death
©ESC 2020
Figure 13 Outline of rate control therapy.
490
AF = atrial fibrillation; AVN = atrioventricular node; bpm = beats per minute; BV = biventricular; CRT =
cardiac resynchronization therapy; CRT-D: cardiac resynchronization therapy defibrillator; CRT-P = cardiac resynchronization therapy pacemaker; ECG
= electrocardiogram; LV = left ventricular; SR = sinus rhythm.
38 ESC Guidelines
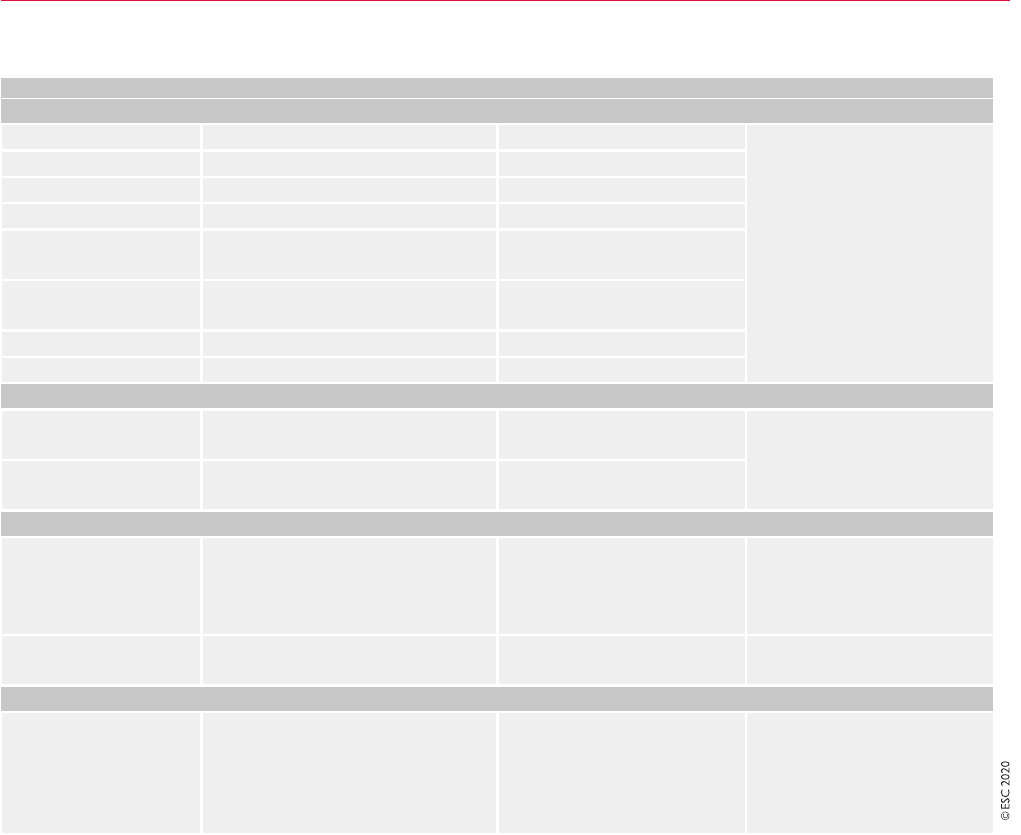
.
.
.
.
.
.
.
.
.
.
or hospitalization for HF, or worsening HF) was significantly less
commonintheablationþ CRT group vs. the drug arm (P =0.013),
and ablation þ CRT patients showed a 36% decrease in symptoms
and physical limitations at 1-year follow-up (P =0.004).
527
Emerging evidence suggest that His-bundle pacing could be an
alternative in these patients.
528
Table 13 Drugs for rate control in AF
a
Intravenous administration Usual oral maintenance dose Contraindicated
Beta-blockers
b
Metoprolol tartrate 2.5 - 5 mg i.v. bolus; up to 4 doses 25 - 100 mg b.i.d. In case of asthma use beta-1-
blockers
Contraindicated in acute HF and
history of severe bronchospasm
Metoprolol XL (succinate) N/A 50 - 400 mg o.d.
Bisoprolol N/A 1.25 - 20 mg o.d.
Atenolol
c
N/A 25 - 100 mg o.d.
Esmolol 500 mg/kg i.v. bolus over 1 min; followed by
50 - 300 mg/kg/min
N/A
Landiolol 100 mg/kg i.v. bolus over 1 min; followed by
10 - 40 mg/kg/min
505
N/A
Nebivolol N/A 2.5 - 10 mg o.d.
Carvedilol N/A 3.125 - 50 mg b.i.d.
Non-dihydropyridine calcium channel antagonists
Verapamil 2.5 - 10 mg i.v. bolusover 5 min 40 mg b.i.d. to 480 mg (extended
release) o.d.
Contraindicated in HFrEF
Adapt doses in hepatic and renal
impairment
Diltiazem 0.25 mg/kg i.v. bolus over 5 min, then 5 - 15
mg/h
60 mg t.i.d. to 360 mg (extended
release) o.d.
Digitalis glycosides
Digoxin 0.5 mg i.v. bolus (0.75 - 1.5 mg over 24
hours in divided doses)
0.0625 - 0.25 mg o.d. High plasma levels associated with
increased mortality
Check renal function before start-
ing and adapt dose in CKD patients
Digitoxin 0.4 - 0.6 mg 0.05 - 0.1 mg o.d. High plasma levels associated with
increased mortality
Other
Amiodarone 300 mg i.v. diluted in 250 mL 5% dextrose
over 30 - 60 min (preferably via central
venous cannula), followed by 900 - 1200
mg i.v. over 24 hours diluted in 500 - 1000
mL via a central venous cannula
200 mg o.d. after loading
3 200 mg daily over 4 weeks,
then 200 mg daily
536 d
(reduce other
rate controlling drugs according to
heart rate)
In case of thyroid disease, only if no
other options
AF = atrial fibrillation; b.i.d. = bis in die (twice a day); CKD = chronic kidney disease; HF = heart failure; HFrEF = HF with reduced ejection fraction; i.v. = intravenous; min =
minutes; N/A = not available or not widely available; o.d. = omni die (once daily); t.i.d. = ter in die (three times a day).
a
All rate control drugs are contraindicated in Wolff-Parkinson-White syndrome, also i.v. amiodarone.
b
Other beta-blockers are available but not recommended as specific rate control therapy in AF and therefore not mentioned here (e.g. propranolol and labetalol).
c
No data on atenolol; should not be used in HFrEF.
d
Loading regimen may vary; i.v. dosage should be considered when calculating total load.
ESC Guidelines 39

©ESC 2020
Figure 14 Choice of rate control drugs.
490
AF = atrial fibrillation; AFL = atrial flutter; COPD = chronic obstructive pulmonary disease; CRT-D = cardiac
resynchronization therapy defibrillator; CRT-P = cardiac resynchronization therapy pacemaker; HFpEF = heart failure with preserved ejection fraction; HFrEF =
heart failure with reduced ejection fraction; NDCC = Non-dihydropyridine calcium channel blocker.
a
Clinical reassessment should be focused on evaluation of
resting heart rate, AF/AFL-related symptoms and quality of life. In case suboptimal rate control (resting heart rate >110 bpm), worsening of symptomsorquality
of life consider 2nd line and, if necessary, 3rd line treatment options.
b
Careful institution of beta-blocker and NDCC, 24-hour Holter to check for bradycardia.
Recommendations for ventricular rate control in patients with AF
a
Recommendations Class
b
Level
c
Beta-blockers, diltiazem, or verapamil are recommended as first-choice drugs to control heart rate in AF patients with
LVEF>_40%.
492,507,511,529
IB
Beta-blockers and/or digoxin are recommended to control heart rate in AF patients with LVEF<40%.
486,491,502,512,530532
IB
Combination therapy comprising different rate controlling drugs
d
should be considered if a single drug does not achieve the target
heart rate.
533,534
IIa B
A resting heart rate of <110 bpm (i.e. lenient rate control) should be considered as the initial heart rate target for rate control therapy.
488
IIa B
Atrioventricular node ablation should be considered to control heart rate in patients unresponsive or intolerant to intensive rate
and rhythm control therapy, and not eligible for rhythm control by LA ablation, accepting that these patients will become pace-
maker dependent.
516,523,535,536
IIa B
In patients with haemodynamic instability or severely depressed LVEF, intravenous amiodarone may be considered for acute con-
trol of heart rate.
504,514,515
IIb B
AF = atrial fibrillation; bpm = beats per minute; ECG = electrocardiogram; LA = left atrial; LVEF = left ventricular ejection fraction.
a
See section 11 for ventricular rate control in various concomitant conditions and AF populations
b
Class of recommendation.
c
Level of evidence.
d
Combining beta-blocker with verapamil or diltiazem should be performed with careful monitoring of heart rate by 24-h ECG to check for bradycardia.
488
40 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
10.2.2 Rhythm control
The ‘rhythm control strategy’ refers to attempts to restore and main-
tain sinus rhythm, and may engage a combination of treatment
approaches, including cardioversion,
164,234
antiarrhythmic medica-
tion,
233,537,538
and catheter ablation,
539541
along with an adequate
rate control, anticoagulation therapy (section 10.2.2.6) and compre-
hensive cardiovascular prophylactic therapy (upstream therapy,
including lifestyle and sleep apnoea management) (Figure 15).
10.2.2.1 Indications for rhythm control
Based on the currently available evidence from RCTs, the primary
indication for rhythm control is to reduce AF-related symptoms and
improve QoL (Figure 15). In case of uncertainty, an attempt to
restore sinus rhythm in order to evaluate the response to therapy
may be a rational first step. Factors that may favour an attempt at
rhythm control should be considered
542,543
(Figure 15).
As AF progression is associated with a decrease in QoL
544
and,
with time, becomes irreversible or less amenable to treatment,
176
rhythm control may be a relevant choice, although currently there is
no substantial evidence that this may result in a different outcome.
Reportedly, rates of AF progression were significantly lower with
rhythm control than rate control.
545
Older age, persistent AF, and
previous stroke/TIA independently predicted AF progression,
545
which may be considered when deciding the treatment strategy. For
many patients, an early intervention to prevent AF progression may
be worth considering,
546
including optimal risk-factor manage-
ment.
245
Ongoing trials in patients with newly diagnosed sympto-
matic AF will assess whether early rhythm control interventions such
as AF catheter ablation offer an opportunity to halt the progressive
patho-anatomical changes associated with AF.
547
However, there is
evidence that, at least in some patients, a successful rhythm control
strategy with AF catheter ablation may not affect atrial substrate
©ESC 2020
Figure 15 Rhythm control strategy. AAD = antiarrhythmic drug; AF = atrial fibrillation; CMP = cardiomyopathy; CV = cardioversion; LAVI = left atrial
volume index; PAF = paroxysmal atrial fibrillation; PVI = pulmonary vein isolation; QoL = quality of life; SR = sinus rhythm.
a
Consider cardioversion to con-
firm that the absence of symptoms is not due to unconscious adaptation to reduced physical and/or mental capacity.
ESC Guidelines 41

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
development.
548
Important evidence regarding the effect of early
rhythm control therapy on clinical outcomes are expected in 2020
from the ongoing EAST (Early treatment of Atrial fibrillation for
Stoke prevention Trial) trial.
549
General recommendations regarding active informed patient
involvement in shared decision making (section 9) also apply for rhythm
control strategies. The same principles should be applied in female and
male AF patients when considering rhythm control therapy.
550
10.2.2.2 Cardioversion
10.2.2.2.1 Immediate cardioversion/elective cardioversion. Acute
rhythm control can be performed as an emergency cardioversion in a
haemodynamically unstable AF patient or in a non-emergency situa-
tion. Synchronized direct current electrical cardioversion is the pre-
ferred choice in haemodynamically compromised AF patients as it is
more effective than pharmacological cardioversion and results in
immediate restoration of sinus rhythm.
554,555
In stable patients, either
pharmacological cardioversion or electrical cardioversion can be
attempted; pharmacological cardioversion is less effective but does
not require sedation. Of note, pre-treatment with AADs can
improve the efficacy of elective electrical cardioversion.
556
ARCT
showed maximum fixed-energy electrical cardioversion was more
effective than an energy-escalation strategy.
557
In a RCT, a wait-and-watch approach with rate control medication
only and cardioversion when needed within 48 h of symptom onset
was as safe as and non-inferior to immediate cardioversion of parox-
ysmal AF, which often resolves spontaneously within 24 h.
558
Elective cardioversion refers to the situation when cardioversion
can be planned beyond the nearest hours. Observational data
243
showed that cardioversion did not result in improved AF-related
QoL or halted AF progression, but many of these patients did not
receive adjunctive rhythm control therapies.
243
Other studies
reported significant QoL improvement in patients who maintain sinus
rhythm after electrical cardioversion and the only variable independ-
ently associated with a moderate to large effect size was sinus rhythm
at 3 months.
232
Factors associated with an increased risk for AF recurrence after
elective cardioversion include older age, female sex, previous cardio-
version, chronic obstructive pulmonary disease (COPD), renal
impairment, structural heart disease, larger LA volume index, and
HF.
164,559,560
Treatment of potentially modifiable conditions should
be considered before cardioversion to facilitate maintenance of sinus
rhythm (Figure 15).
245
In case of AF recurrence after cardioversion in
patients with persistent AF, an early re-cardioversion may prolong
subsequent duration of sinus rhythm.
561
Non-emergency cardioversion is contraindicated in the presence
of known LA thrombus. Peri-procedural thrombo-embolic risk
should be evaluated and peri-procedural and long-term OAC use
considered irrespective of cardioversion mode (i.e. pharmacological
cardioversion or electrical cardioversion) (section 10.2.2.6). A flow-
chart for decision making on cardioversion is shown in Fig ure 16.
10.2.2.2.2 Electrical cardioversion. Electrical cardioversion can be per-
formed safely in sedated patients treated with i.v. midazolam and/or
propofol or etomidate.
562
BP monitoring and oximetry during the pro-
cedure should be used routinely. Skin burns may occasionally be
observed. Intravenous atropine or isoproterenol, or temporary trans-
cutaneous pacing, should be available in case of post-cardioversion bra-
dycardia. Biphasic defibrillators are standard because of their superior
efficacy compared with monophasic defibrillators.
563,564
Anterior
posterior electrode positions restore sinus rhythm more effec-
tively,
554,555
while other reports suggest that specific electrical pad
positioning is not critically important for successful cardioversion.
565
10.2.2.2.3 Pharmacological cardioversion (including ‘pill in the pocket’).
Pharmacological cardioversion to sinus rhythm is an elective proce-
dure indicated in haemodynamically stable patients. Its true efficacy is
biased by the spontaneous restoration of sinus rhythm within 48 h of
hospitalization in 76 - 83% of patients with recent onset AF (10 - 18%
within first 3 h, 55 - 66% within 24 h, and 69% within 48 h).
566568
Therefore, a ‘wait-and-watch’ strategy (usually for <24 h) may be
considered in patients with recent-onset AF as a non-inferior alterna-
tive to early cardioversion.
558
The choice of a specific drug is based on the type and severity of
associated heart disease (Table 14), and pharmacological cardiover-
sion is more effective in recent onset AF. Flecainide (and other class
Ic agents), indicated in patients without significant LV hypertrophy
(LVH), LV systolic dysfunction, or ischaemic heart disease, results in
prompt (3 - 5 h) and safe
569
restoration of sinus rhythm in >50% of
patients,
570574
while i.v. amiodarone, mainly indicated in HF patients,
has a limited and delayed effect but can slow heart rate within
12 h.
570,575577
Intravenous vernakalant is the most rapidly cardio-
verting drug, including patients with mild HF and ischaemic heart dis-
ease, and is more effective than amiodarone
578583
or flecainide.
584
Dofetilide is not used in Europe and is rarely used outside Europe.
Ibutilide is effective to convert atrial flutter (AFL) to sinus rhythm.
585
In selected outpatients with rare paroxysmal AF episodes, a self-
administered oral dose of flecainide or propafenone is slightly less
effective than in-hospital pharmacological cardioversion but may be
preferred (permitting an earlier conversion), provided that the drug
safety and efficacy has previously been established in the hospital set-
ting.
586
An atrioventricular node-blocking drug should be instituted in
patients treated with class Ic AADs (especially flecainide) to avoid
transformation to AFL with 1:1 conduction.
587
10.2.2.2.4 Follow-up after cardioversion. The goals of follow-up after
cardioversion are shown in Table 15. When assessing the efficacy of a
rhythm control strategy, it is important to balance symptoms and
AAD side-effects. Patients should be reviewed after cardioversion to
detect whether an alternative rhythm control strategy including AF
catheter ablation, or a rate control approach is needed instead of cur-
rent treatment.
Recommendations for rhythm control
Recommendations Class
a
Level
b
Rhythm control therapy is recommended for
symptom and QoL improvement in sympto-
matic patients with AF.
551553
IA
AF = atrial fibrillation; QoL = quality of life.
a
Class of recommendation.
b
Level of evidence.
42 ESC Guidelines

©ESC 2020
Figure 16 Flowchart for decision making on cardioversion of AF depending on clinical presentation, AF onset, oral anticoagulation intake, and risk factors
for stroke. AF = atrial fibrillation; CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age
65 - 74 years, Sex category (female); cardioversion = cardioversion; ECV = electrical cardioversion; h = hour; LA = left atrium; LAA = left atrial appendage;
LMWH = low-molecular-weight heparin; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagulant; TE = thromboembolism; TOE
= transoesophageal echocardiography; UFH = unfractionated heparin; VKA = vitamin K antagonist.
ESC Guidelines 43

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
................................................................................................................................................................................................................................................................................................
Table 14 Antiarrhythmic drugs used for restoration of sinus rhythm
Antiarrhythmic drugs for restoration of sinus rhythm (pharmacological cardioversion)
Drug Administration
route
Initial dose for
cardioversion
Further dosing for
cardioversion
Acute success rate and
expected time to sinus
rhythm
Contraindications/precautions/comments
Flecainide
a
Oral
b
i.v.
200300 mg
2 mg/kg over 10 min
- Overall: 5978%
(51% at 3 h, 72% at 8 h)
•
Should not be used in ischaemic heart disease and/or signifi-
cant structural heart disease
•
May induce hypotension, AFL with 1:1 conduction (in
3.5 - 5.0% of patients)
•
Flecainide may induce mild QRS complex widening
•
Do NOT use for pharmacological cardioversion of AFL
Propafenone
a
Oral
b
i.v.
450600 mg
1.5 - 2 mg/kg over 10 min
- Oral: 4555% at 3 h,
6978% at 8 h;
i.v.: 4389%
Up to 6 h
Vernakalant
c
i.v. 3 mg/kg over 10 min 2 mg/kg over 10 min
(10 - 15 min after the initial
dose)
<1 h (50% conversion
within 10 min)
•
Should not be used in patients with arterial hypotension (SBP
<100 mmHg), recent ACS (within 1 month), NYHA III or IV
HF, prolonged QT, or severe aortic stenosis
•
May cause arterial hypotension, QT prolongation, QRS wid-
ening, or non-sustained ventricular tachycardia
Amiodarone
a
i.v. 5 - 7 mg/kg over 1 - 2 h 50 mg/h (maximum 1.2 g for
24 h)
44%
(812 h to several days)
•
May cause phlebitis (use a large peripheral vein, avoid i.v.
administration >24 hours and use preferably volumetric
pump)
•
May cause hypotension, bradycardia/atrioventricular block,
QT prolongation
•
Only if no other options in patients with hyperthyroidism
(risk of thyrotoxicosis)
Ibutilide
c
i.v. 1 mg over 10 min
0.01 mg/kg if body
weight <60 kg
1 mg over 10 min
(10 - 20 min after the initial
dose)
3151% (AF)
6373% (AFL)
1h
•
Effective for conversion of AFL
•
Should not be used in patients with prolonged QT, severe
LVH, or low LVEF
•
Should be used in the setting of a cardiac care unit as it may
cause QT prolongation, polymorphic ventricular tachycardia
(torsades de pointes)
•
ECG monitoring for at least 4 hours after administration to
detect a proarrhythmic event
AAD = antiarrhythmic drug; ACS = acute coronary syndrome; AF = atrial fibrillation; AFL = atrial flutter; b.i.d. ¼ bis in die (twice a day); CrCl = creatinine clearance; CYP2D6 = cytochrome P450 2D6; ECG = electrocardiogram; EHRA =
European Heart Rhythm Association; HCM = hypertrophic cardiomyopathy; HF = heart failure; i.v. = intravenous; LV = left ventricular; LVEF = left ventricular ejection fraction; LVH = LV hypertrophy; NYHA = New York Heart
Association; QRS = QRS interval; QT = QT interval; SA = sinoatrial; SBP = systolic blood pressure; VKA = vitamin K antagonist.
a
Most frequently used for cardioversion of AF, available in most countries.
b
May be self-administered by selected outpatients as a ‘pill-in-the-pocket’ treatment strategy.
c
Not available in some countries.
For more details regarding pharmacokinetic or pharmacodynamic properties refer to EHRA AADsclinical use and clinical decision making: a consensus document.
568
44 ESC Guidelines

10.2.2.3 Atrial fibrillation catheter ablation
AF catheter ablation is a well-established treatment for the preven-
tion of AF recurrences.
1,602604
When performed by appropriately
trained operators, AF catheter ablation is a safe and superior alterna-
tive to AADs for maintenance of sinus rhythm and symptom
improvement.
165,235242,246,247,605618
It is advised to discuss the effi-
cacy and complication rates of AF catheter ablation and AADs with
the patient once rhythm control as long-term management has been
selected.
10.2.2.3.1 Indications. In the following section, indications for AF cath-
eter ablation are presented for paroxysmal and persistent AF in
patients with and without risk factors for post-ablation AF recur-
rence. Differentiation of persistent and long-standing persistent AF
was omitted because the latter only expresses the duration of persis-
tent AF above an arbitrary and artificial cut-off at 12 months’ dura-
tion. The significance of such a cut-off as a single measure has never
been substantially proven.
A number of risk factors for AF recurrence after AF ablation have
been identified, including LA size, AF duration, patient age, renal dys-
function, and substrate visualization by means of MRI.
619625
Recent
systematic reviews on prediction models for AF recurrence after
catheter ablation showed the potential benefits of risk predictions,
but a more robust evaluation of such models is desirable.
167,626
The
model variables can be measured before ablation; therefore models
could be used pre-procedurally to predict the likelihood of
recurrence.
627635
However, no single score has been presently
identified as consistently superior to others. Thus, at present, for an
improved and more balanced indication for ablation in patients with
persistent AF and risk factors for recurrence, the most intensely eval-
uated risk predictors (including duration of AF) should be considered,
and adjusted to the individual patient’s situation including their prefer-
ences. Notably, patients must also be explicitly informed about the
importance of treating modifiable risk factors to reduce risk of recur-
rent AF.
621,636652
The indications for AF catheter ablation are summarized in
Figure 17. AF catheter ablation is effective in maintaining sinus rhythm
in patients with paroxysmal and persistent AF.
165,235242,605616
The
main clinical benefit of AF catheter ablation is the reduction of
arrhythmia-related symptoms.
246,247,603,604,607,617,653,654
This has
been confirmed in a recent RCT showing that the improvement in
QoL was significantly higher in the ablation vs. medical therapy group,
Table 15 Goals of follow-up after cardioversion of AF
Goals
Early recognition of AF recurrence by ECG recording after cardioversion
Evaluation of the efficacy of rhythm control by symptom assessment
Monitoring of risk for proarrhythmia by regular control of PR, QRS, and QTc intervals in patients on Class I or III AADs
Evaluation of balance between symptoms and side-effects of therapy considering QoL and symptoms
Evaluation of AF-related morbidities and AAD-related side-effects on concomitant cardiovascular conditions and LV function
Optimization of conditions for maintenance of sinus rhythm including cardiovascular risk management (BP control, HF treatment, increasing cardiorespira-
tory fitness, and other measures, see section 11).
AAD = antiarrhythmic drug; AF = atrial fibrillation; BP = blood pressure; ECG = electrocardiogram; HF = heart failure; LV = left ventricular; PR = PR interval; QoL = quality of
life; QRS = QRS interval; QTc = corrected QT interval.
Recommendations for cardioversion
Recommendations Class
a
Level
b
For pharmacological cardioversion of recent-
onset AF, i.v. vernakalant (excluding patients
with recent ACS or severe HF) or flecainide or
propafenone (excluding patients with severe
structural heart disease) is
recommended.
569,573,579,582,588590
IA
Intravenous amiodarone is recommended for
cardioversion of AF in patients with HF or struc-
tural heart disease, if delayed cardioversion is
consistent with clinical situation.
515,591,592
IA
Cardioversion of AF (either electrical or phar-
macological) is recommended in symptomatic
patients with persistent AF as part of rhythm
control therapy.
232,233,593,594
IB
Pharmacological cardioversion of AF is
indicated only in a haemodynamically stable
patient, after consideration of the thrombo-
embolic risk.
595
IB
Pre-treatment with amiodarone, flecainide, ibu-
tilide, or propafenone should be considered to
facilitate the success of electrical
cardioversion.
556,596599
IIa B
In selected patients with infrequent and recent-
onset AF and no significant structural or ischae-
mic heart disease, a single self-administered oral
dose of flecainide or propafenone (‘pill in the
pocket’ approach) should be considered for
patient-led cardioversion, but only following effi-
cacy and safety assessment.
574,586,600,601
IIa B
For patients with sick-sinus syndrome, atrioven-
tricular conduction disturbances or prolonged
QTc (>500 ms), pharmacological cardioversion
should not be attempted unless risks for proar-
rhythmia and bradycardia have been considered.
III C
ACS = acute coronary syndrome; AF = atrial fibrillation; HF = heart failure; ms =
milliseconds; i.v. = intravenous; QTc = corrected QT interval. Note: For cardio-
version in various specific conditions and AF populations see section 11.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 45

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
as was the associated reduction in AF burden.
246
Symptom improve-
ment has also been confirmed in the recent large CABANA
(Catheter ABlation vs. ANtiarrhythmic Drug Therapy for Atrial
Fibrillation) RCT,
655
but the trial showed that the strategy of AF cath-
eter ablation did not significantly reduce the primary composite out-
come of death, disabling stroke, serious bleeding, or cardiac arrest
compared with medical therapy.
617
As no RCT has yet demonstrated
a significant reduction in all-cause mortality, stroke, or major bleeding
with AF catheter ablation in the ’general’ AF population, the indica-
tions for the procedure have not been broadened beyond symptom
relief,
617
and AF catheter ablation is generally not indicated in asymp-
tomatic patients. Further important evidence regarding the impact of
ablation on major cardiovascular events is expected from the EAST
trial.
656
In selected patients with HF and reduced LVEF, two RCTs have
shown a reduction in all-cause mortality and hospitalizations with AF
catheter ablation,
611,657
although combined mortality and HF hospi-
talization was a primary endpoint only in the CASTLE-AF (Catheter
Ablation vs. Standard conventional Treatment in patients with LEft
ventricular dysfunction and Atrial Fibrillation) trial.
657
The generaliz-
ability of the trial has recently been evaluated in a large HF patient
population.
658
This analysis showed that only a small number of
patients met the trial inclusion criteria (<10%) and patients who met
the CASTLE-AF inclusion criteria had a significant benefit from treat-
ment as demonstrated in the trial.
658
The smaller AMICA (Atrial
Fibrillation Management in Congestive Heart Failure With Ablation)
RCT, which included patients with more advanced HFrEF, did not
show benefits gained by AF catheter ablation at 1-year follow-up,
659
whereas a recent CABANA subgroup analysis supported the benefits
of AF catheter ablation in patients with HFrEF, showing a significant
reduction in the study primary endpoint (death, stroke, bleeding, car-
diac arrest) and reduced mortality in the ablation group.
617,660
Overall, AF catheter ablation in patients with HFrEF results in higher
rates of preserved sinus rhythm and greater improvement in LVEF,
exercise performance, and QoL compared with AAD and rate con-
trol.
611,657,661671
Accordingly, ablation should be considered in
patients with HFrEF who have been selected for rhythm control
treatment to improve QoL and LV function, and to reduce HF hospi-
talization and, potentially, mortality.
When AF-mediated tachycardia-induced cardiomyopathy (i.e. ven-
tricular dysfunction secondary to rapid and/or asynchronous/irregu-
lar myocardial contraction, partially or completely reversed after
treatment of the causative arrhythmia) is highly suspected, AF cathe-
ter ablation is recommended to restore LV function.
672676
Ablation is recommended, in general, as a second-line therapy
after failure (or intolerance) of class I or class III AADs. This
recommendation is based on the results of multiple RCTs showing
superiority of AF catheter ablation vs. AADs regarding freedom from
recurrent arrhythmia or improvement in symptoms, exercise
capacity, and QoL after medication
failure.
235239,246,247,605607,609,611,613617
Clinical trials considering AF catheter ablation before any AAD
suggest that AF catheter ablation is more effective in maintaining sinus
rhythm, with comparable complication rates in experienced cen-
tres.
240242,614
The 5-year follow-up in the MANTRA-PAF (Medical
Antiarrhythmic Treatment or Radiofrequency Ablation in
Paroxysmal Atrial Fibrillation) trial showed a significantly lower AF
burden in the ablation arm that did not, however, translate into
improved QoL compared with AAD treatment,
615
whereas the
CAPTAF (Catheter Ablation compared with Pharmacological
©ESC 2020
Figure 17 Indications for catheter ablation of symptomatic AF. The arrows from AAD to ablation indicate failed drug therapy. AAD = antiarrhythmic
drug; AF = atrial fibrillation; EF = ejection fraction; LA = left atrial.
a
Significantly enlarged LA volume, advanced age, long AF duration, renal dysfunction, and
other cardiovascular risk factors.
b
In rare individual circumstances, catheter ablation may be carefully considered as first-line therapy.
c
Recommended to
reverse LV dysfunction when tachycardiomyopathy is highly probably.
d
To improve survival and reduce hospitalization.
46 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Therapy for Atrial Fibrillation) study showed that, in AF patients
mostly naive to class I and III AADs, the greater improvement in QoL
in the ablation arm was directly associated with greater reduction in
AF burden compared with the AAD arm.
246
Based on these studies
and patient preferences, AF catheter ablation should be considered
before a trial of AAD in patients with paroxysmal AF episodes (class
IIa), or may be considered in patients with persistent AF without risk
factors for recurrence (class IIb).
10.2.2.3.2 Techniques and technologies. The cornerstone of AF cathe-
ter ablation is the complete isolation of pulmonary veins by linear
lesions around their antrum, either using point-by-point
radiofrequency ablation or single-shot ablation
devices.
235,237,239,607609,612,613,654,677686
Unfortunately, persistent
pulmonary vein electrical isolation is difficult to achieve (pulmonary
vein reconnection rates of >70% are reported
683,687697
, but could
be significantly lower with the newer generation of catheters
698700
).
Particularly in persistent and long-standing persistent AF, more
extensive ablation has been advocated. This may include linear
lesions in the atria, isolation of the LAA or of the superior vena cava,
ablation of complex fractionated electrograms, rotors, non-
pulmonary foci, or ganglionated plexi, fibrosis-guided voltage and/or
MRI-mapping, or ablation of high dominant frequency sites.
701710
However, additional benefit vs. pulmonary vein isolation (PVI) alone,
justifying its use during the first procedure, is yet to be con-
firmed.
677,680,711730
A RCT-based data suggest improved outcome
with targeting extrapulmonary (particularly the LAA) foci and selec-
tive ablation of low-voltage areas as adjunct to PVI.
708,725
In patients
with documented cavotricuspid isthmus (CTI)-dependent flutter
undergoing AF catheter ablation, right isthmus ablation may be con-
sidered.
731734
In case of non-CTI-dependent atrial tachycardia, the
ablation technique depends on the underlying mechanism and tachy-
cardia focus or circuit.
1,614
Several RCTs and observational studies have compared point-by-
point radiofrequency and cryoballoon ablation, mostly in the first
procedure for paroxysmal AF.
612,681,735755
They reported broadly
similar arrhythmia-free survival and overall complications with either
technique, with slightly shorter procedure duration but longer
fluoroscopy time with cryoballoon ablation.
612,681,735755
However,
some studies showed reduced hospitalization and lower complica-
tion rates with cryoballoon ablation.
746,756,757
The choice of energy
source may depend on centre availability, operator preference/expe-
rience, and patient preference. Alternative catheter designs and
energy sources have been developed in an attempt to simplify the
ablation procedure and improve outcomes,
613,755,758761
but further
evidence is required before changing current recommendations.
10.2.2.3.3 Complications. Prospective, registry-based data show that
approximately 4 - 14% of patients undergoing AF catheter ablation
experience complications, 2 - 3% of which are potentially life-threat-
ening.
602604,762765
In the recent CABANA trial, mostly including
experienced high-volume centres, complications occurred in the
lower range of these rates.
617
Complications occur mostly within the
first 24 h after the procedure, but some may appear 1 - 2 months
after ablation
1,602604
(Table 16 and Supplementary Table 10). Peri-
procedural death is rare (<0.2%) and usually related to cardiac
tamponade.
603,604,766770
10.2.2.3.4 AF catheter ablation outcome and impact of modifiable risk
factors. Multiple RCTs have compared AADs with AF catheter abla-
tion using different technologies/energy sources, either as ‘first-line’
therapy or after AAD failure, showing superiority of AF catheter abla-
tion in arrhythmia-free survival.
165,235242,605616
However, many
patients require several procedures and late recurrences are not
infrequent.
248,639,772780
Key outcomes include QoL, HF, stroke, and mortal-
ity.
539541,608,781,782
Compared with AADs, AF catheter ablation was
associated with significant and sustained improvement in QoL scores
in several RCTs and meta-analyses.
1,235,239242,246,247,539541,783,784
To date, there is no RCT sufficiently large to properly evaluate a
reduction in stroke by catheter ablation.
Several factors, including AF type and
duration,
235237,239,607,609,612,613,654,680,682,785
and the presence of
comorbidities such as hypertension,
621,639641
obesity,
638,639,643,646,772,786791
metabolic syndrome,
792794
and
sleep apnoea
643645,647652
may influence the outcome of catheter
..................................................................................
Table 16 Procedure-related complications in catheter ablation and thoracoscopic ablation of AF
771
Complication severity Complication type Complication rate
Catheter ablation Thoracoscopic ablation
Life-threatening complications Periprocedural death <0.1% <0.1%
Oesophageal perforation/fistula <0.5% N/A
Periprocedural thromboembolic event <1.0% <1.5%
Cardiac tamponade 1% <1.0%
Severe complications Pulmonary vein stenosis <1.0% N/A
Persistent phrenic nerve palsy <1.0% N/A
Vascular complications 2-4% N/A
Conversion to sternotomy N/A <1.7%
Pneumothorax N/A <6.5%
Moderate or minor complications Various 1 - 2% 1 - 3%
Complications of unknown significance Asymptomatic cerebral embolism 5 - 15% N/A
NA = not available.
ESC Guidelines 47

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
ablation (Figure 18 and Supplementary Box 2). Prospective cohort
studies suggest that aggressive control of modifiable risk factors may
improve arrhythmia-free survival after catheter ablation.
636
10.2.2.3.5 Follow-up after atrial fibrillation ablation. AF catheter abla-
tion is a complex procedure that may be associated with a range of
specific post-procedural complications (section
10.2.2.3.3)
603,604,766770
. Although mostly rare, potentially cata-
strophic complications may initially present with non-specific symp-
toms and signs to which managing physicians should be attuned. Key
issues in follow-up are shown in Tab le 17.
10.2.2.3.6 Risk assessment for recurrence of atrial fibrillation post cath-
eter ablation. Recurrence of AF after catheter ablation is driven by
the complex interaction of various factors. These include increasing
AF duration, age, and LA size,
619624
and structural factors such as
the abundance of epicardial fat tissue
807810
and the presence of
atrial substrate as evident from electrical or morphological
markers.
811
A number of risk-prediction scores have been evaluated
(for detailed description see Supplementary Table 11 and
Supplem entary Bo x 2). Whereas these scores only moderately predict
AF recurrence, one of the strongest predictors is early recurrent AF,
indicating the need for further refinement of these scoring
systems.
629
©ESC 2020
Figure 18 Risk factors for AF contributing to the development of an
abnormal substrate translating into poorer outcomes with rhythm con-
trol strategies. AF = atrial fibrillation; BMI = body mass index; CPAP =
continuous positive airway pressure; HbA
1C
= haemoglobin A1c; OSA =
obstructive sleep apnoea. Several AF risk factors may contribute to the
development of LA substrates and thus affect the outcome of AF catheter
ablation, predisposing to a higher recurrence rate. Aggressive control of
modifiable risk factors may reduce recurrence rate.
Table 17 Key issues in follow-up after AF catheter ablation
Key issues
Recognition and management of complications
•
Patients must be fully informed about the clinical signs and symptoms of rare but potentially dangerous ablation-related complications that may occur after
hospital discharge (e.g. atrio-oesophageal fistula, pulmonary vein stenosis).
Follow-up monitoring:
Useful to assess procedural success and correlate symptom status with rhythm.
795,796
Recurrences beyond the first month post-ablation are generally pre-
dictive of late recurrences,
797,798
but recurrent symptoms may be due to ectopic beats or other non-sustained arrhythmia
640,799,800
; conversely the presence
of asymptomatic AF after ablation is well described.
801803
Monitoring may be performed with intermittent ECG, Holter, Patch recordings, external or implanted loop recorder, or smart phone monitor (although
the latter has not been validated for such use). Patients should be first reviewed at a minimum of 3 months and annually thereafter.
1
Management of antiarrhythmic medication and treatment of AF recurrences
a. Continuing AAD treatment for 6 weeks to 3 months may reduce early AF recurrences, rehospitalizations and cardioversions during this period.
797,804
Clinical practice regarding routine AAD treatment after ablation varies and there is no convincing evidence that such treatment is routinely needed.
b. Subsequently, AADs may be weaned, ceased, or continued according to symptoms and rhythm status. Recent findings suggest that in AAD-treated
patients remaining free of AF at the end of the blanking period, AAD continuation beyond the blanking period reduces arrhythmia recurrences.
805
Management of anticoagulation therapy
a. In general, OAC therapy is continued for 2 months following ablation in all patients.
1,806
Beyond this time, a decision to continue OAC is determined pri-
marily by the presence of CHA
2
DS
2
-VASc stroke risk factors rather than the rhythm status (section 10.2.2.6).
AAD = antiarrhythmic drug; AF = atrial fibrillation; CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age
65 - 74 years, Sex category (female); ECG=electrocardiogram; OAC = oral anticoagulant.
48 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
10.2.2.4 Surgery for atrial fibrillation
With development of the maze procedure for surgical cure from AF,
Cox et al. opened up a new window of therapeutic opportunities for
AF patients.
822
The classical cut-and-sew maze procedure underwent
several modifications and various device-based surgical ablation pro-
cedures have been developed.
823,824
More than 200 publications
documented the application of these techniques and technologies in
various clinical scenarios.
825
Most studies are retrospective and/or
observational, but some RCTs and meta-analyses have also been
published.
771,826828
While the effects of surgical ablation on rhythm
outcome (i.e. restoration of sinus rhythm/freedom from AF) have
been clearly demonstrated, the effects on endpoints such as QoL,
hospitalization, stroke, and mortality are not well estab-
lished.
461,827,829,830
The only RCT with longer follow-up has shown a
significant reduction in stroke risk at 5 years and a greater likelihood
of maintaining sinus rhythm although the trial was underpowered for
Recommendations for rhythm control/catheter ablation of AF
Recommendations Class
a
Level
b
General recommendations
For the decision on AF catheter ablation, it is recommended to take into consideration the procedural risks and the major risk factors
for AF recurrence following the procedure and discuss them with the patient.
235237,239,607,609,612,613,636,638,652,654,680,682,785,789
IB
Repeated PVI procedures should be considered in patients with AF recurrence provided the patient’s symptoms were improved after
the initial PVI.
812814
IIa B
AF catheter ablation after failure of drug therapy
AF catheter ablation for PVI is recommended for rhythm control after one failed or intolerant class I or III AAD, to improve symp-
toms of AF recurrences in patients with
235238,247,605609,612,613,615617,654,677,678,680,682,685,758,779,780,815
:
I
•
Paroxysmal AF, or
A
•
Persistent AF without major risk factors for AF recurrence, or
A
•
Persistent AF with major risk factors for AF recurrence.
B
AF catheter ablation for PVI should be considered for rhythm control after one failed or intolerant to beta-blocker treatment to
improve symptoms of AF recurrences in patients with paroxysmal and persistent AF.
246
IIa B
First-line therapy
AF catheter ablation for PVI should/may be considered as first-line rhythm control therapy to improve symptoms in selected patients
with symptomatic:
•
Paroxysmal AF episodes,
240242,614,615
or
IIa B
•
Persistent AF without major risk factors for AF recurrence.
253255,264,598601,609,610,633,636,641,724,745,746,832
IIb C
as an alternative to AAD class I or III, considering patient choice, benefit, and risk.
AF catheter ablation:
•
Is recommended to reverse LV dysfunction in AF patients when tachycardia-induced cardiomyopathy is highly probable, inde-
pendent of their symptom status.
666,675,676
IB
•
Should be considered in selected AF patients with HF with reduced LVEF to improve survival and reduce HF
hospitalization.
612,659,662666,668671,817826
IIa B
AF catheter ablation for PVI should be considered as a strategy to avoid pacemaker implantation in patients with AF-related bradycar-
dia or symptomatic pre-automaticity pause after AF conversion considering the clinical situation.
816818
IIa C
Techniques and technologies
Complete electrical isolation of the pulmonary veins is recommended during all AF catheter-ablation
procedures.
235237,239,606,608610,613,614,678,679,681,683,684,686,713,731,759,780
IA
If patient has history of CTI-dependent AFL or if typical AFL is induced at the time of AF ablation, delivery of a CTI lesion may be
considered.
731733,819821
IIb B
Use of additional ablation lesions beyond PVI (low voltage areas, lines, fragmented activity, ectopic foci, rotors, and others) may be
considered but is not well established.
677,680,708,711730
IIb B
Lifestyle modification and other strategies to improve outcomes of ablation
Weight loss is recommended in obese patients with AF, particularly those who are being evaluated to undergo AF
ablation.
636,638,639,643,646,772,786791
IB
Strict control of risk factors and avoidance of triggers are recommended as part of a rhythm control strategy.
636,637
IB
AAD = antiarrhythmic drug; AF = atrial fibrillation; AFL = atrial flutter; CTI = cavotricuspid isthmus; HF = heart failure; LV = left ventricular; LVEF = left ventricular ejection
fraction; PVI = pulmonary vein isolation.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 49

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
stroke risk assessment.
828
The largest registry published, from the
Polish National Health Service, describes better survival when abla-
tion is performed concomitant to mitral or coronary surgery.
831,832
Close cooperation between cardiac surgeons and electrophysiolo-
gists (heart team) for proper patient selection and postoperative
management, especially for handling of arrhythmia recurrences,
seems advisable for high-standard quality care.
10.2.2.4.1 Concomitant surgery for atrial fibrillation: indications, out-
come, complications. Most trials of concomitant AF ablation have been
based mainly on patients undergoing mitral valve repair or replacement.
While surgical PVI has been shown to be effective for maintaining sinus
rhythm,
833
the most effective ablation treatment for AF isolates the pul-
monary veins and the LA posterior wall, creates ablation lines that
impede electrical impulses around the most important structures
(mitral and tricuspid annuli, venae cavae and appendages), and excludes
the LAA. Most evidence supports bipolar radiofrequency clamps and
cryothermy to perform a maze.
834
For non-paroxysmal AF, a biatrial
lesion pattern is more effective than left-sided only, performed by ster-
notomy or minimally invasive techniques.
826
In general, the same preoperative risk factors for AF recurrence
after concomitant AF surgery as for AF catheter ablation have been
identified. These include LA size, patient age, AF duration, HF/
reduced LVEF, and renal dysfunction.
379,636,835841
The significant
positive effects of concomitant surgical ablation on freedom from
atrial arrhythmias is clearly documented. Most RCTs with 1-year
follow-up show no effect on QoL, stroke, and mortality,
842845
but
some reported reduced event rates.
828,830,846
Surgical AF ablation concomitant to other cardiac surgery signifi-
cantly increases the need for pacemaker implantation with biatrial
(but not left-sided) lesions,
827
being reported from 6.8% to 21.5%,
while other complications are not increased.
827830,846,847
10.2.2.4.2 Stand-alone surgery for atrial fibrillation: indications, out-
come, complications. Thoracoscopic radiofrequency ablation targets
the pulmonary veins, LA posterior wall, and LAA closure in AF patients
with no structural heart disease. Freedom from AF after the procedure
is well documented, but only a few studies have reported improved
QoL.
844,845,848850
A recent meta-analysis of three RCTs showed a sig-
nificantly higher freedom from atrial tachyarrhythmia and less need for
repeat ablations after thoracoscopic ablation compared with AF cathe-
ter ablation for paroxysmal or persistent AF.
851
The FAST trial
randomized patients who were prone to AF catheter-ablation failure
(i.e. failed previous ablation or LA dilatation and hypertension) and
reported common but substantially lower recurrence after thoraco-
scopic compared with AF catheter ablation (56% vs. 87%) at long-term
follow-up (mean 7 years).
849
Hospitalization was longer and complica-
tion rates of surgical ablation were higher compared with catheter
ablation
771
(Table 16). A systematic safety analysis of thoracoscopic
ablation showed a 30-day complication rate of 11.3%, mainly self-
limiting, whereas it was significantly lower (3.6%) in a multicentre regis-
try.
456
In RCTs, thoracoscopic ablation proved more effective in
rhythm control than catheter ablation; however, surgical ablation is
more invasive, with higher complication rates and longer hospitaliza-
tion.
461,852
Because of this risk-benefit ratio of surgical vs. catheter
ablation, it seems reasonable to consider thoracoscopic surgery prefer-
entially in patients with previous failed catheter ablation or with a high
risk of catheter-ablation failure. There are no convincing data on the
effects on stroke of surgical ablation as a stand-alone procedure or in
combination with LAA occlusion or exclusion. Hence, OAC therapy
should be continued after the procedure regardless of rhythm out-
come in AF patients with stroke risk factors.
10.2.2.5 Hybrid surgical/catheter ablation procedures
Hybrid AF procedures combine a minimally invasive epicardial non-
sternotomy ablation not using cardiopulmonary bypass with a percutane-
ous endocardial approach. They can be performed as a single intervention
or sequentially, when the endocardial catheter mapping and, if needed,
additional ablations are done within 6 months after the epicardial proce-
dure.
853
There are no studies comparing these two hybrid strategies.
A systematic review on rhythm outcome and complications with a
hybrid procedure or AF catheter ablation in patients with persistent
or long-standing persistent AF showed that at 12 months or longer, a
hybrid procedure achieved a significantly higher rate of freedom from
atrial arrhythmias with and without the use of AAD compared with
AF catheter ablation. Although the overall complication rate was low
for both strategies, hybrid ablations had more complications (13.8%
vs. 5.9%).
854
The difference in outcome could be explained by a long-
lasting isolation of the pulmonary veins after bipolar radiofrequency
clamping of the pulmonary veins, epicardial clipping of the LAA, and
the add-on possibility of an endocardial touch-up.
855,856
Recommendations for surgical ablation of AF
Recommendations Class
a
Level
b
Concomitant AF ablation should be considered
in patients undergoing cardiac surgery, balancing
the benefits of freedom from atrial arrhythmias
and the risk factors for recurrence (left atrial
dilatation, years in AF, age, renal dysfunction, and
other cardiovascular risk factors).
461,843,857859
IIa A
Thoracoscopic—including hybrid surgical abla-
tion—procedures should be considered in
patients who have symptomatic paroxysmal or
persistent AF refractory to AAD therapy and
have failed percutaneous AF ablation, or with
evident risk factors for catheter failure, to main-
tain long-term sinus rhythm. The decision must
be supported by an experienced team of elec-
trophysiologists and surgeons.
860,861
IIa B
Thoracoscopic—including hybrid surgical abla-
tion—procedures may be considered in patients
with persistent AF with risk factors for recur-
rence, who remain symptomatic during AF
despite at least one failed AAD and who prefer
further rhythm control therapy.
IIb C
AAD = antiarrhythmic drug; AF = atrial fibrillation.
a
Class of recommendation.
b
Level of evidence.
50 ESC Guidelines

10.2.2.6 Peri-procedural stroke risk management in patients undergoing
rhythm control interventions
10.2.2.6.1 Management of stroke risk and oral anticoagulant therapy in
atrial fibrillation patients undergoing cardioversion. Patients undergoing
cardioversion of AF are at increased risk of stroke and thrombo-
embolism, especially in the absence of OAC and if AF has been
present for >_12 h.
860862
The exact duration of an AF episode
before cardioversion may be difficult to ascertain, as many patients
develop AF asymptomatically, seeking help only when symptoms or
complications occur. If there is uncertainty over the exact onset of
AF (i.e. unknown duration of AF), peri-cardioversion anticoagulation
is managed as for AF of >12 h to 24 h. Mechanisms of the increased
propensity to peri-cardioversion thrombo-embolism include the
presence of pre-existing thrombus (especially if not anticoagulated),
change in the atrial mechanical function with restoration of sinus
rhythm, atrial stunning post-cardioversion, and a transient prothrom-
botic state.
863
No RCT has evaluated anticoagulation vs. no anticoagulation in AF
patients undergoing cardioversion with a definite duration of
AF<48 h. Observational data suggest that the risk of stroke/
thrombo-embolism is very low (0 - 0.2%) in patients with a definite
AF duration of <12 h and a very low stroke risk (CHA
2
DS
2
-VASc 0
in men, 1 in women),
860,864,865
in whom the benefit of 4-week antico-
agulation after cardioversion is undefined and the prescription of anti-
coagulants can be optional, based on an individualized approach.
Peri-cardioversion anticoagulation with a VKA results in a signifi-
cant decrease of stroke and thrombo-embolism,
863
but achieving the
necessary therapeutic anticoagulation (INR 2.0 - 3.0) for a minimum
of 3 weeks before cardioversion may be difficult. This 3-week period
is arbitrary, based on the time presumably needed for endothelializa-
tion or resolution of pre-existing AF thrombus. To shorten this time,
TOE-guided cardioversion was introduced. If there is no atrial throm-
bus on TOE, cardioversion is performed after administration of hepa-
rin, and OAC is continued post-cardioversion.
866,867
As NOACs act rapidly, cardioversion can be scheduled 3 weeks
after NOAC initiation, provided that patients are counselled about
the need for compliance to NOAC therapy
868870
; NOACs have at
least comparable efficacy and safety to warfarin in AF patients under-
going cardioversion.
871874
A review of the three largest prospective
trials (n =5203 patients) showed that the composite primary out-
come (stroke/systemic embolism, myocardial infarction,
or cardiovascular death) was significantly reduced with NOACs com-
pared with VKA.
873
Long-term OAC therapy after cardioversion should not be based
on successful restoration of sinus rhythm, but on the stroke risk pro-
file (using the CHA
2
DS
2
-VASc score), balanced against bleeding risk
(e.g. HAS-BLED score).
For patients in whom a thrombus is identified on TOE, effective
anticoagulation for at least 3 weeks before reassessment for cardio-
version is recommended. A repeat TOE to ensure thrombus resolu-
tion should be considered before cardioversion.
875
Antithrombotic
management for these patients is challenging and decided on an indi-
vidual basis based on the efficacy (or inefficacy) of previous
treatments.
Recommendations for stroke risk management peri-
cardioversion
Recommendations Class
a
Level
b
In patients with AF undergoing cardioversion,
NOACs are recommended with at least similar
efficacy and safety to warfarin.
868873
IA
For cardioversion of AF/AFL, effective anticoagu-
lation is recommended for a minimum of 3
weeks before cardioversion.
866870
IB
TOE is recommended to exclude cardiac throm-
bus as an alternative to 3-week pre-procedural
anticoagulation when early cardioversion is
planned.
866,868870,875
IB
In patients at risk of stroke, it is recommended
that OAC therapy is continued long term after
cardioversion according to the long-term antico-
agulation recommendations, irrespective of the
method of cardioversion, the apparent mainte-
nance of sinus rhythm, or characterization of AF
as a ‘first-diagnosed episode’.
412,872,876
IB
When thrombus is identified on TOE, effective
anticoagulation is recommended for at least 3
weeks before cardioversion of AF.
875
IB
It is recommended that the importance of adher-
ence and persistence to NOAC treatment both
before and after cardioversion is strongly
emphasized to patients.
IC
Effective anticoagulation should be initiated as
soon as possible before every cardioversion of
AF or AFL.
866870
IIa B
Early cardioversion can be performed without
TOE in patients with an AF duration of <48 h.
866
IIa B
In patients with AF duration of >24 h undergoing
cardioversion, therapeutic anticoagulation
should be continued for at least 4 weeks, even
after successful cardioversion to sinus rhythm
(beyond 4 weeks, the decision about long-term
OAC treatment is determined by the presence
of stroke risk factors).
860,861
IIa B
When thrombus is identified on TOE, a repeat
TOE to ensure thrombus resolution should be
considered before cardioversion.
875
IIa C
In patients with a definite duration of AF <_24 h
and a very low stroke risk (CHA
2
DS
2
-VASc of 0
in men or 1 in women) post-cardioversion anti-
coagulation for 4 weeks may be omitted.
871,876
IIb C
AF = atrial fibrillation; AFL = atrial flutter; CHA
2
DS
2
-VASc = Congestive heart
failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease,
Age 65 - 74 years, Sex category (female); NOAC = non-vitamin K antagonist oral
anticoagulant; OAC = oral anticoagulant; TOE = transoesophageal
echocardiography.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 51

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
10.2.2.6.2 Management of stroke risk and oral anticoagulant ther-
apy in atrial fibrillation patients undergoing atrial fibrillation cathe-
ter ablation. Although there is some variability in the peri-
procedural OAC management in patients undergoing AF ablation,
more recently operators have moved towards a strategy of per-
forming the ablation under uninterrupted VKA or NOAC treat-
ment, provided the INR is within therapeutic range. In non-
anticoagulated patients, initiating therapeutic anticoagulation 3 - 4
weeks before ablation may be considered.
1
In a meta-analysis of 12 studies,
877
uninterrupted anticoagulation
using NOACs vs. VKAs for AF catheter ablation was associated with
low rates of stroke/TIA (NOACs, 0.08%; VKA, 0.16%) and similar
rates of silent cerebral embolic events (8.0% vs 9.6%). However,
major bleeding was significantly reduced with uninterrupted NOACs
(0.9%) compared with VKAs (2%).
In the largest RCT comparing peri-procedural NOAC vs. warfarin
[the RE-CIRCUIT trial (Randomized Evaluation of dabigatran etexi-
late Compared to warfarIn in pulmonaRy vein ablation: assessment of
different peri-proCedUral antIcoagulation sTrategies)],
878
the inci-
dence of major bleeding events during and up to 8 weeks after abla-
tion was significantly lower with dabigatran vs. warfarin (1.6% vs.
6.9%). Other RCTs (VENTURE-AF with rivaroxaban,
879
AXAFA-AF
NET 5 with apixaban,
880
and ELIMINATE-AF with edoxaban
881
)also
showed similar event rates under uninterrupted NOACs vs. VKAs.
Overall, uninterrupted peri-procedural NOACs were associated
with a low incidence of stroke/TIA and a significant reduction in
major bleeding compared with uninterrupted VKAs in patients
undergoing AF catheter ablation. In contrast, heparin bridging
increases the bleeding risk and should be avoided.
Frequently, the term ‘uninterrupted’ is used in clinical practice for
the description of regimens where one or two NOAC doses are
omitted before ablation, whereas in the RCTs comparing uninter-
rupted NOACs vs. warfarin, NOAC administration before ablation
was truly uninterrupted.
869,878
Hence, there is no reason to recom-
mend omitting one or two NOAC doses before ablation. After the
procedure, administration of the first dose the evening after ablation
or the next morning (if this corresponds to the timing of the next
dose according to the patient’s previous OAC regimen) appears to
be safe.
878,881
10.2.2.6.3 Postoperative anticoagulation after surgery for atrial
fibrillation. Owing to endothelial damage during ablation, OAC is
advisable in all patients after AF surgery, starting as soon as possible
(balancing the risk of postoperative bleeding). There are no RCT
data regarding interruption of OAC over the long term. Non-
randomized studies with longer follow-up have shown better long-
term freedom from stroke in patients with persistent sinus rhythm,
but not in those with AF despite LAA exclusion.
824
Therefore, long-
term OAC is recommended in all patients at risk of stroke despite a
successful maze surgery and appendage closure.
10.2.2.7 Long-term antiarrhythmic drug therapy for rhythm control
10.2.2.7.1 Antiarrhythmic drugs. The aim of AAD therapy is to
improve AF-related symptoms.
484,882,883
Hence, the decision to ini-
tiate long-term AAD therapy needs to balance symptom burden,
possible adverse drug reactions, and patient preferences. The princi-
ples of AAD therapy are shown in Tables 18 and 19.
Compared with no therapy, AAD therapy approximately doubles
sinus rhythm maintenance,
883
but it is difficult to draw firm
Recommendations for stroke risk management peri-catheter ablation
Recommendations Class
a
Level
b
In AF patients with stroke risk factors not taking OAC before ablation, it is recommended that pre-procedural management of stroke
risk includes initiation of anticoagulation and:
•
Preferably, therapeutic OAC for at least 3 weeks before ablation, or
•
Alternatively, the use of TOE to exclude LA thrombus before ablation.
I
C
IIa C
For patients undergoing AF catheter ablation who have been therapeutically anticoagulated with warfarin, dabigatran, rivaroxaban,
apixaban, or edoxaban, performance of the ablation procedure without OAC interruption is recommended.
878,879,881
IA
After AF catheter ablation, it is recommended that:
•
Systemic anticoagulation with warfarin or a NOAC is continued for at least 2 months post ablation, and
•
Long-term continuation of systemic anticoagulation beyond 2 months post ablation is based on the patient’s stroke risk profile and
not on the apparent success or failure of the ablation procedure.
IC
AF = atrial fibrillation; LA = left atrial; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagulant therapy; TOE=transoesophageal echocardiography.
a
Class of recommendation
b
Level of evidence
Recommendations for postoperative anticoagulation
after AF surgery
Recommendations Class
a
Level
b
Long-term OAC therapy is recommended in
patients after AF surgery and appendage closure,
based on the patient’s thrombo-embolic risk
assessed with the CHA
2
DS
2
-VASc score.
IC
AF = atrial fibrillation; CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension,
Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 65 - 74 years, Sex
category (female); OAC = oral anticoagulant.
a
Class of recommendation.
b
Level of evidence.
52 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
conclusions from existing trials on their comparative efficacy.
884
In
general, AAD therapy is less effective than AF catheter abla-
tion,
114,611,615
but previously ineffective AADs can be continued after
PVI, to reduce rec urrent AF.
805
A shorter duration of AAD therapy
would likely reduce the risk of side-effects
883,885
but late recurrences
may oc cur.
595
Short-term AAD therapy is also used to prevent early
AF recurrences after catheter ablation,
886
although the benefit is still
debated
797,887
; this strategy may be reasonable in patients deemed at
increased risk of AAD side-effects or in those with a low perceived
risk of recurrent AF. Concomitant management of underlying
cardiovascular conditions is pivotal to reduce AF symptom burden
and facilitate the maintenance of sinus rhythm.
245,636,888,889
10.2.2.7.1 Available antiarrhythmic drugs. Several AADs have been
shown to reduce AF recurrences (Table 20).
890
Class Ia (quinidine
and disopyramide) and sotalol have been associated with increased
overa ll mo rtality.
884
Again, safety should dictate both the initiation
and continuation of AADs.
A flow chart for use of AADs for long-term rhythm control,
depending on the underlying disease, is given in Figure 19.
10.2.2.7.2 Non-antiarrhythmic drugs with antiarrhythmic properties
(upstream therapy). Either resulting from, or being a marker of, struc-
tural atrial remodelling, AF is closely related to atrial cardiomyopathy.
Drugs that affect the atrial-remodelling process could prevent new-
onset AF acting as non-conventional AADs (i.e. upstream therapy)
(Table 21).
Recently, the RACE 3 study
245
confirmed the importance of
assessing underlying conditions and targeted upstream therapy for
intense risk-factor control in AF patients with mild or moderate HF
in optimizing rhythm control. The results showed that targeted ther-
apy of underlying conditions improves maintenance of sinus rhythm
in patients with persistent AF.
A list of new investigational antiarrhythmic drugs is provided in
Supplem entary Box 3.
Table 19 Rules to initiate antiarrhythmic drugs for long-term rhythm control in AF
Consideration Criteria
Indication for AAD
•
Is the patient symptomatic?
•
Are AF symptoms severe enough (EHRA class) to justify AAD use?
•
Are there associated conditions predicting poor tolerance of AF episodes?
When to start AAD
•
Usually not for the first episode, but it may enhance efficacy of cardioversion
How to choose among AADs
•
Minimize proarrhythmic risk and organ toxicity
Evaluate for:
•
basal ECG abnormalities (QRS duration, PR, QTc) and possible interference with AAD
•
impact on LV function
•
important pharmacokinetic and pharmacodynamic interactions (i.e. antithrombotic drugs)
•
Risk factors for proarrhythmia may be dynamic and change over time
How to minimize proarrhythmic risk
•
Evaluate ECG after the treatment, as indicated in these Guidelines
•
Evaluate periodically for organ toxicity (amiodarone)
•
Long-term Holter monitoring and exercise test in selected cases
•
Avoid AAD combinations
How to verify efficacy
•
Estimate AF burden under therapy (ask patient for noting episodes)
•
If the patient is already on AAD and it was effective but was stopped because of intolerance,
choose preferably from the same class
Adjuvant interventions and hybrid therapy
•
In patients with atrioventricular conduction abnormalities and/or sinus node dysfunction,
pacemaker implantation should be considered if AAD therapy is deemed necessary
•
Short-term AAD therapy could prevent early recurrences after AF ablation
AAD = antiarrhythmic drug; AF = atrial fibrillation; ECG = electrocardiogram; EHRA = European Heart Rhythm Association; LV = left ventricular; PR = PR interval; QRS =
QRS interval; QTc = corrected QT interval.
Table 18 Principles of antiarrhythmic drug therapy
143
Principles
AAD therapy aims to reduce AF-related symptoms
Efficacy of AADs to maintain sinus rhythm is modest
Clinically successful AAD therapy may reduce rather than eliminate AF
recurrences
If one AAD ‘fails’, a clinically acceptable response may be achieved by
another drug
Drug-induced proarrhythmia or extracardiac side-effects are frequent
Safety rather than efficacy considerations should primarily guide the
choice of AAD
AAD = antiarrhythmic drug; AF = atrial fibrillation.
ESC Guidelines 53

Table 20 Antiarrhythmic drugs used for long-term maintenance of sinus rhythm in AF patients
890
Drug Administration
route
Dose Contraindications/precautions/comments
Amiodarone
233,506,891896
Oral 3 200 mg daily over
4 weeks, then 200 mg
daily
506
•
The most effective AAD
890,897
•
RCTs showed lower AF recurrence compared with sotalol and
dronedarone
884
•
Also reduces ventricular rate (for 10 - 12 bpm), safe in patients with
HF
898900
•
Concomitant use with other QT-prolonging drugs with caution
•
Concomitant use with VKAs or digitalis (their dose should be reduced)
•
Increased risk of myopathy when used with statins
•
Requires regular surveillance for liver, lung, and thyroid toxicity
•
Has atrioventricular nodal-slowing properties, but should not be
used as first intention for rate control
•
QT prolongation is common but rarely associated with torsades de
pointes (<0.5%)
901
•
Torsades de pointes occurs infrequently during treatment with amio-
darone (the proarrhythmia caution requires QT-interval and TU-
wave monitoring)
902
•
Should be discontinued in case of excessive QT prolongation
(>500 ms)
•
ECG at baseline, after 4 weeks
•
Contraindicated in manifest hyperthyroidism
•
Numerous and frequent extracardiac side-effects may warrant dis-
continuation of amiodarone, thus making it a second-line treatment
when other choices are possible
903907
Flecainide
Flecainide slow release
896,908,909
Oral 100 - 200 mg b.i.d., or
200 mg once daily (fle-
cainide slow release)
•
Effective in preventing recurrence of AF
891,908,910
•
Should not be used in patients with CrCl <35 mL/min/1.73 m
2
and
significant liver disease
•
Both are contraindicated in patients with ischaemic heart disease or
reduced LVEF
911913
•
Should be discontinued in case of QRS widening >25% above base-
line and patients with left bundle-branch block or any other conduc-
tion block >120 ms
•
Caution when sinoatrial/atrioventricular conduction disturbances
present
a
•
CYP2D6 inhibitors increase concentration
•
May increase AFL cycle length, thus promoting 1:1 atrioventricular
conduction and increasing ventricular rate.
914
This risk can be
reduced by concomitant administration of an atrioventricular nodal-
blocking drug such as a beta-blocker or NDCC
•
In patients properly screened for propensity to proarrhythmias, both
flecainide and propafenone are associated with a low proarrhythmic
risk
915
•
ECG at baseline, after 1 - 2 weeks
Propafenone
Propafenone slow
release
895,896,916922
Oral 150 - 300 mg three
times daily, or
225 - 425 mg b.i.d.
(propafenone slow
release)
•
Should not be used in patients with significant renal or liver disease,
ischaemic heart disease, reduced LV systolic function, or asthma
•
Should be discontinued in case of QRS widening >25% above base-
line and in patients left bundle-branch block and any other conduc-
tion block >120 ms
•
Caution when sinoatrial/atrioventricular conduction disturbances
present
a
•
Increases concentration of warfarin/acenocoumarin and digoxin
when used in combination
•
May increase AFL cycle length, thus promoting 1:1 atrioventricular
conduction and increasing ventricular rate
•
ECG at baseline and after 1 - 2 weeks
Continued
54 ESC Guidelines

Table 20 Continued
Drug Administration
route
Dose Contraindications/precautions/comments
Dronedarone
923927
Oral 400 mg b.i.d.
•
Less effective than amiodarone in rhythm control but has very few
extracardiac side-effects
925,928930
•
Reduces cardiovascular hospitalizations and death in patients with
paroxysmal or persistent AF or AFL and cardiovascular
comorbidity
923,931
•
Associated with increased mortality in patients with recent decom-
pensated HF
927
or permanent AF
932
•
Dronedarone has the most solid safety data and may thus be a pref-
erable first choice,
933,934
however not indicated in patients with HF
and permanent AF
935,936
•
Should not be used in NYHA class III or IV or unstable HF, in combi-
nation with QT-prolonging drugs or with strong CYP3A4 inhibitors
(e.g. verapamil, diltiazem) and in patients with CrCl <30 mL/min
•
Concomitant use with dabigatran is contraindicated
•
Combination with digoxin may significantly increase digoxin serum
concentration
•
When used with digitalis or beta-blockers their doses should be
reduced
•
Should be discontinued in case of excessive QT prolongation
(>500 ms or >60 ms increase)
•
A modest increase in serum creatinine is common and reflects drug-
induced reduction in CrCl rather than a decline in renal function
937
•
Has atrioventricular nodal-slowing properties
•
ECG at baseline and after 4 weeks
Sotalol (d,l racemic
mixture)
233,891,894,895,920,938940
Oral 80 - 160 mg b.i.d.
•
Only class III effects if dosing >160 mg daily
•
Considering its safety and efficacy and potential drug alternatives,
sotalol should be used with a caution
•
Should not be used in patients with HFrEF, significant LVH, pro-
longed QT, asthma, hypokalaemia, or CrCl <30 mL/min
•
Dose-related torsades de pointes may occur in >2% of patients
941
•
Should be discontinued in case of excessive QT prolongation
(>500 ms or >60 ms increase)
•
Should not be used if CrCl <50 mL/min
•
The potassium channel-blocking effect increases with increasing dose
and, consequently, the risk of ventricular proarrhythmia (torsades de
pointes) increases
•
Observational data and a recent meta-analysis revealed a correlation
with an increased all-cause mortality
890,897,934
, whereas a nationwide
registry analysis and two RCTs found no evidence for increased
safety concerns with sotalol
233,933,942,943
•
ECG at baseline, after 1 day and after 1 - 2 weeks
Disopyramide
944946
Oral 100 - 400 mg two or
t.i.d. (maximum 800 mg/
24 h)
•
Associated with significantly increased mortality
890,947
, and rarely
used for rhythm control in AF.
948,949
Should not be used in patients
with a structural heart disease. Rarely used for rhythm control in AF
patients, due to increased mortality and frequent intolerance to side-
effects
•
May be useful in ‘vagal’ AF occurring in athletes or during sleep
901
•
Reduces LV outflow obstruction and symptoms in patients with
HCM
950
AAD = antiarrhythmic drug; AF = atrial fibrillation; AFL = atrial flutter; b.i.d. = bis in die (twice a day); bpm = beats per minute; CrCl = creatinine clearance; CYP2D6 = cyto-
chrome P450 2D6; CYP34A = cytochrome 34A; ECG=electrocardiogram; HCM = hypertrophic cardiomyopathy; HF = heart failure; HFrEF = HF with reduced ejection frac-
tion; LV = left ventricular; LVEF = LV ejection fraction; LVH = LV hypertrophy; NDCC = non-dihydropyridinecalcium-channel blocker; NYHA = New York Heart Association;
QRS = QRS interval; QT = QT interval; RCT=randomized controlled trial; SBP = systolic blood pressure; t.i.d. = ter in die (three times a day); VKA = vitamin K antagonist.
a
Caution is needed when using any AAD in patients with conduction-system disease (e.g. sinoatrial or atrioventricular node disease).
ESC Guidelines 55

©ESC 2020
Figure 19 Long-term rhythm control therapy. ACEi = angiotensin converting enzyme inhibitor; AF = atrial fibrillation; ARB = angiotensin receptor
blocker; CAD=coronary artery disease; HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction;LV=
left ventricular; LVH = left ventricular hypertrophy; MRA=mineralocorticoid receptor antagonist.
Table 21 Non-antiarrhythmic drugs with antiarrhythmic properties (upstream therapy)
Drugs Comment
ACEi, ARBs Activated renin-angiotensin-aldosterone system is up-regulated in AF.
951,952
ACEi and ARBs showed encouraging results in preventing
AF in preclinical studies.
953
As suggested by retrospective analyses and studies where AF was a prespecified secondary endpoint, ACEi/ARBs could prevent new-
onset AF in patients with LV dysfunction, LVH, or hypertension.
954961
As initial treatment, ACEi and ARBs seem to be superior to other antihypertensive regimens,
962
but ARBs did not reduce AF burden
in patients without structural heart disease.
963
Despite several positive small-scale prospective studies and retrospective analyses,
larger RCTs have shown controversial results and failed to confirm the role of ACEi or ARBs in secondary (post-cardioversion) pre-
vention of AF.
964
The multifactorial pathways for AF promotion and study design could explain these negative results and should not
discourage the use of ACEi or ARB to AAD in patients with structural heart disease.
MRAs Aldosterone is implicated in inducibility and perpetuation of AF.
965967
Evidence from RCTs showed that MRAs reduced new-onset
atrial arrhythmias in patients with HFrEF in parallel with improvement of other cardiovascular outcomes.
968,969
Recently, the positive impact of MRAs was also shown in patients with HFpEF
970
irrespective of baseline AF status. Regarding other
renin-angiotensin-aldosterone system inhibitors, the role of MRAs as upstream therapy in rhythm control strategy for patients with
HF and AF has not been clarified. As AF is a marker of HF severity, the beneficial antiarrhythmic effect could be driven indirectly,
through improvement of HF. A recent meta-analysis showed that MRAs significantly reduced new-onset AF and recurrent AF, but not
postoperative AF.
971
Beta-blockers Several small studies suggested a lower AF recurrence rate with beta-blockers, with a comparable efficacy with sotalol.
939,972,973
However, most evidence pleads against a significant role of beta-blockers in preventing AF.
890
The observed beneficial effect could
also result from transformation of clinically manifested AF to silent AF, because of the rate control with beta-blockers.
Statins Statins are attractive candidates for upstream therapy, as the role of inflammation in AF is well established. However, in an adequately
designed RCT,
974
statins failed to show a beneficial effect, and their preventive effect was not confirmed in other settings.
975,976
Specific patient groups in whom statins could induce reverse remodelling are not identified yet, but findings from the CARAF registry
suggested that AF patients already on beta-blockers could benefit from statin therapy.
977
Polyunsaturated fatty acids also failed to
show convincing benefit in preventing AF.
978982
AAD = antiarrhythmic drug; ACEi = angiotensin converting enzyme inhibitor; AF = atrial fibrillation; ARB=angiotensin receptor blocker; CARAF = Canadian Registry of Atrial
Fibrillation; HF = heart failure; HFrEF = HF with reduced ejection fraction; HFpEF = HF with preserved ejection fraction; LV = left ventricular; LVH = LV hypertrophy; MRA =
mineralocorticoid receptor antagonist; RCT = randomized controlled trial.
56 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
10.2.2.7.3 Assessment and long-term monitoring of the risk of proar-
rhythmia with antiarrhythmic drugs. A variety of clinical, echocardio-
graphic, and ECG criteria have been associated with a higher risk of
proarrhythmia.
986989
Increasing age, female sex, impaired renal and/
or liver function, and known CAD have been variously identified as
associated with higher risk.
890,990992
Concomitant AAD use, hypo-
kalaemia, or family history of sudden death have also been impli-
cated.
990
Proarrhythmic events tend to cluster shortly after drug
initiation, especially if a loading dose or a change in usual dosage is
prescribed.
568
For quinidine, the risk is idiosyncratic independent of
dosage. Impaired LV function and LVH are echocardiographic
markers of increased proarrhythmic risk. Sotalol has a proarrhythmic
risk even in the absence of structural heart disease. On the 12-lead
ECG, prolonged corrected QT interval (QTc), widened QRS, and
prolonged PR interval have all been associated with
proarrhythmia.
993995
Significant ion-channel mutations have been
detected in only a minority of cases of drug-induced torsade.
996
Periodic ECG analysis for proarrhythmia signs has been used success-
fully in recent AAD trials
594,
.
997
Specifically, ECG monitoring was
used systematically on days 13 in patients receiving flecainide, prop-
afenone, or sotalol to identify those at risk of proarrhythmia
233,594,
.
998
The role of routine use of exercise stress testing in patients com-
mencing 1C drugs who had no evidence of structural heart disease is
still debatable
915,
.
999
10.3 ‘C’ Cardiovascular risk factors
and concomitant diseases: detection and
management
Cardiovascular risk-factor burden and comorbidities, including life-
style factors and borderline conditions, significantly affect the lifetime
risk for AF development (Supplementary Figure 5). The continuum of
unhealthy lifestyle, risk factor(s), and cardiovascular disease can con-
tribute to atrial remodelling/cardiomyopathy and development of AF
that commonly results from a combined effect of multiple interacting
factors (often without specific threshold values).
The ‘C’ component of the ABC pathway includes identification
and management of concomitant diseases, cardiometabolic risk fac-
tors, and unhealthy lifestyle factors. Management of risk factors and
cardiovascular disease complements stroke prevention and reduces
AF burden and symptom severity. In a recent RCT, for example, tar-
geted therapy of underlying conditions significantly improved mainte-
nance of sinus rhythm in patients with persistent AF and HF.
245
Whereas strategies on comprehensive risk-factor modification
and interventions targeting underlying conditions have shown reduc-
tion of AF burden and recurrence, studies addressing isolated man-
agement of specific conditions alone (e.g. hypertension) yielded
inconsistent findings,
1000
likely because the condition was not a sole
contributor to AF.
10.3.1 Lifestyle interventions
10.3.1.1 Obesity and weight loss
Obesity increases the risk for AF progressively according to body
mass in dex.
366,10011005
It may also increase the risk for ischaemic
stroke, thrombo-embolism, and death in AF patients,
366
notwith-
standing an obesity paradox in AF patients, especially regarding all-
cause and cardiovascular death, with an inverse relationship between
overweight/obesity and better cardiovascular prognosis in long-term
follow-up.
1006
Intense weight reduction with comprehensive management of
concomitant cardiovascular risk factors resulted in fewer AF recur-
rences and symptoms than general advice in obese patients with
AF
636,888,
.
889
Achieving a healthy weight may reduce blood pressure
(BP), dyslipidaemia, and risk of developing type 2 diabetes mellitus,
Recommendations for long-term antiarrhythmic drugs
Recommendations Class
a
Level
b
Amiodarone is recommended for long-term rhythm control in all AF patients, including those with HFrEF. However, owing to its
extracardiac toxicity, other AADs should be considered first whenever possible.
233,570,884,942,983,985
IA
Dronedarone is recommended for long-term rhythm control in AF patients with:
•
Normal or mildly impaired (but stable) LV function, or
•
HFpEF, ischaemic, or VHD.
884,923,925,985
IA
Flecainide or propafenone is recommended for long-term rhythm control in AF patients with normal LV function and without struc-
tural heart disease, including significant LVH and myocardial ischaemia.
594,884,910,942,983,984
IA
In AF patients treated with sotalol, close monitoring of QT interval, serum potassium levels, CrCl, and other proarrhythmia risk fac-
tors is recommended.
884,942
IB
In AF patients treated with flecainide for long-term rhythm control, concomitant use of an atrioventricular nodal-blocking drug (if tol-
erated) should be considered.
IIa C
Sotalol may be considered for long-term rhythm control in patients with normal LV function or with ischaemic heart disease if close
monitoring of QT interval, serum potassium levels, CrCl, and other proarrhythmia risk factors is provided.
233,983
IIb A
AAD therapy is not recommended in patients with permanent AF under rate control and in patients with advanced conduction dis-
turbances unless antibradycardia pacing is provided.
III C
AAD = antiarrhythmic drug; AF = atrial fibrillation; CrCl = Creatinine clearance; HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced
ejection fraction; LV = left ventricular; LVH = LV hypertrophy; VHD = Valvular heart disease.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 57

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
thus improving the cardiovascular risk profile.
1007
Obesity may
increase AF recurrence rates after AF catheter ablation (with OSA as
a potential confounder).
638,643,789,1008
It has also been linked to a
higher radiation dose and complication rate during AF abla-
tion,
1009,1010
whereas symptom improvement after AF catheter abla-
tion seems comparable in obese and normal-weight patients.
1008
Given the potential to reduce AF episodes by weight reduction, AF
catheter ablation should be offered to obese patients in conjunction
with lifestyle modifications for weight reduction (Figure 18).
10.3.1.2 Alcohol and caffeine use
Alcohol excess is a risk factor for incident AF
10111014
and bleed-
ing
395
in anticoagulated patients (mediated by poor adherence, liver
disease, variceal bleeding, and risk of major trauma), and high alcohol
intake may be associated with thrombo-embolism or death.
1015
In a
recent RCT, alcohol abstinence reduced arrhythmia recurrence in
regular drinkers with AF.
1016
By contrast, it is unlikely that caffeine consumption causes or con-
tributes to AF.
47
Habitual caffeine consumption might be associated
with lower risk of AF, but caffeine intake may increase symptoms of
palpitations unrelated to AF.
10.3.1.3 Physical activity
Many studie s have demonstrated beneficial effects of moderate exer-
cise/physical activity on cardiovascular health.
10171019
Nevertheless,
the incidence of AF appears to be increased among elite athletes, and
multiple small studies reported a relationship between AF and vigorous
physical ac tivity, ma inly related to long-term or endurance sport partic-
ipation.
10201023
A non-linear relationship between physical activity
and AF seems likely. Based on these data, patients should be encour-
aged to undertake moder ate-in tensity exerc ise and remain phy sically
active to prevent AF incidence or recurrence, but maybe avoid chronic
excessive endurance exercise (such as marathons and lon g-distance tri-
athlons, etc.), especially if aged >50 years. Owing to few randomized
patients and outcomes, the effect of exercise-based cardiac rehabilita-
tion on mortality or serious adverse events is uncertain.
1024
10.3.2 Specific cardiovascular risk factors/comorbidities
10.3.2.1 Hypertension
Hypertension is the most common aetiological factor associated with
the developmen t of AF, and patients with hypertension have a 1.7-fold
higher risk of developing AF compared with normotensives.
26,1025
Hypertension also adds to the complications of AF, particularly
stroke, HF, and bleeding risk. AF patients with a longer hypertension
duration or uncontrolled systolic BP (SBP) levels should be catego-
rized as ‘high-risk’, and strict BP control in addition to OAC is impor-
tant to reduce the risk of ischaemic stroke and ICH.
Given the importance of hypertension as a precipitating factor for
AF, which should be regarded as a manifestation of hypertension
target-organ damage, treatment of hypertension consistent with cur-
rent BP guidelines
1026
is mandatory in AF patients, aiming to achieve
BP<_130/80 mmHg to reduce adverse outcomes.
338,1027,1028
A recent
randomized trial in patients with paroxysmal AF and hypertension
reported fewer recurrences in patients undergoing renal denervation
in addition to PVI compared with patients undergoing PVI only.
1029
Sotalol should not be used in the presence of hypertensive LVH or
renal impairment, owing to the risk of proarrhythmia. There is some
evidence of angiotensin converting enzyme or angiotensin receptor
blocker use to improve outcomes in AF or reduce progression of the
arrhythmia
26,
.
1025
Other lifestyle changes, including obesity manage-
ment, alcohol reduction, and attention to OSA, may also help in
patients with AF and hypertension.
10.3.2.2 Heart failure
The interactions between AF and HF and the optimal management of
patients with both AF and HF are discussed in section 11.6.
10.3.2.3 Coronary artery disease
The interactions between AF and CAD and the optimal management
of patients with both AF and CAD are discussed in section 11.3.
10.3.2.4 Diabetes mellitus
In addition to shared risk factors (e.g. hypertension and obe-
sity),
1004,1030
diabetes is an independent risk factor for AF, especially in
young patients.
1031
Silent AF episodes are favoured by concurrent
autonomic dysfunction,
1032
thus suggesting an opportunity for routine
screening for AF in diabetes mellitus patients. The prevalence of AF is
at least two-fold higher in patients with diabetes compared with people
without diabetes,
1033
and AF incidence rises with increasing severity of
microvascular complications (retinopathy, renal disease).
1034
Both type
1 and type 2 diabetes mellitus are the risk factors for stroke.
342,1035
Intensive glycaemic control does not affect the rate of new-onset
AF,
1036
but metformin and pioglitazone could be associated with
lower long-term risk of AF in patients with diabetes,
1037
while this
was not confirmed for rosiglitazone.
1038
Currently there is no evi-
dence that glucagon-like peptide-1 agonists, sodium glucose co-
transporter-2 inhibitors, and dipeptidyl peptidase-4 inhibitors affect
the development of AF.
1039
Previous meta-analyses showed no significant interaction between
diabetes mellitus and NOAC effects in AF patients,
423,1040
but vascu-
lar mortality was lower in patients with diabetes treated with
NOACs than in those on warfarin.
1040
Bleeding risk reduction with
NOACs was similar in diabetic and non-diabetic patients except for
apixaban, where a lower reduction in haemorrhagic complications
was reported in the AF patients with diabetes compared with AF
patients without diabetes.
1041
Regarding potential side-effects of
OAC, there is no evidence that bleeding risk is increased in patients
with diabetes and retinopathy.
341
Optimal glycaemic control in 12 months before AF catheter abla-
tion was associated with significant reduction in recurrent AF after
ablation.
1042
10.3.2.5 Sleep apnoea
The most common form of sleep-disordered breathing, OSA, is
highly prevalent in patients with AF, HF, and hypertension, and is
associated with increased risk of mortality or major cardiovascular
events.
1043
In a prospective analysis, approximately 50% of AF
patients had OSA compared with 32% of controls.
1044
The mecha-
nisms facilitating AF include intermittent nocturnal hypoxemia/hyper-
capnia, intrathoracic pressure shifts, sympathovagal imbalance,
oxidative stress, inflammation, and neurohumoral activation.
1045
OSA has been shown to reduce success rates of AADs, electrical car-
dioversion, and catheter ablation in AF.
1045
58 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Continuous positive airway pressure (CPAP) is the therapy of
choice for OSA, and may ameliorate OSA effects on AF recur-
rences.
1046,1047
Observational studies and meta-analyses showed
that appropriate CPAP treatment of OSA may improve rhythm con-
trol in AF patients.
648,649,10471051
It seems reasonable to test for OSA before the initiation of rhythm
control therapy in symptomatic AF patients, with the aim to reduce
symptomatic AF recurrences (Figure 18). In the ARREST-AF
(Aggressive Risk Factor Reduction Study Implication for AF) and
LEGACY (Long-term Effect of Goal-directed weight management on
an Atrial fibrillation Cohort: a 5-Year follow-up study) studies, an
aggressive risk-factor reduction programme focusing on weight man-
agement, hyperlipidaemia, OSA, hypertension, diabetes, smoking ces-
sation, and alcohol-intake reduction significantly reduced AF burden
after PVI.
636,1052
However, it remains unclear how and when to test
for OSA and implement OSA management in the standard work-up
of AF patients.
11 The ABC pathway in specific
clinical settings/conditions/patient
populations
In this section, the management of AF in patient populations with spe-
cific conditions is described. The principles of the ABC pathway apply
in these settings as well. Additionally, specific considerations are given
for each of these special conditions and populations.
11.1 Atrial fibrillation with
haemodynamic instability
Acute haemodynamic instability (i.e. syncope, acute pulmonary
oedema, ongoing myocardial ischaemia, symptomatic hypotension,
or cardiogenic shock) in AF patients presenting with a rapid ventricu-
lar rate requires prompt intervention. In severely compromised
patients, emergency electrical cardioversion should be attempted
without delay, and anticoagulation should be started as soon as
possible.
In critically ill patients and those with severely impaired LV systolic
function, AF is often precipitated/exacerbated by increased sympa-
thetic tone, inotropes, and vasopressors, and rhythm control is often
unsuccessful. It is important to identify and correct precipitating fac-
tors and secondary causes and optimize background treatment.
Owing to their rate-controlling effect during exertion and increased
sympathetic tone, rather than only at rest, beta-blockers are pre-
ferred over digitalis glycosides for ventricular rate control in AF.
490
Beta-blockers and NDCC antagonists may exert a negative inotropic
effect (the latter are contraindicated in HFrEF). Digoxin is often
unsuccessful due to the increased sympathetic tone in these patients.
As conventional therapy is often ineffective or not well-toler-
ated,
490
electrical cardioversion should always be considered, even as
initial therapy, whereas intravenous amiodarone may be instituted
for rate control (or potential cardioversion to sinus rhythm), with or
without electrical cardioversion.
504,514,515
Intravenous administration
of amiodarone may lead to a further decrease in BP.
11.2 First-diagnosed (new-onset) atrial
fibrillation
First-diagnosed or new-onset AF is a working diagnosis in a patient
without a history of AF, until the pattern of AF can be defined more
Recommendations for lifestyle interventions and man-
agement of risk factors and concomitant diseases in
patients with AF
Recommendations Class
a
Level
b
Identification and management of risk factors
and concomitant diseases is recommended as an
integral part of treatment in AF patients.
888
IB
Modification of unhealthy lifestyle and targeted
therapy of intercurrent conditions is recom-
mended to reduce AF burden and symptom
severity.
245,636,887,889,1016,1052
IB
Opportunistic screening for AF is recommended
in hypertensive patients.
26,172,222
IB
Attention to good BP control is recommended in
AF patients with hypertension to reduce AF recur-
rences and risk of stroke and bleeding.
26,1035
IB
In obese patients with AF, weight loss together
with management of other risk factors should be
considered to reduce AF incidence, AF progres-
sion, AF recurrences, and symptoms.
898,899,1011
IIa B
Advice and management to avoid alcohol excess
should be considered for AF prevention and in
AF patients considered for OAC
therapy.
324,1012,1014,1016
IIa B
Physical activity should be considered to help
prevent AF incidence or recurrence, with the
exception of excessive endurance exercise,
which may promote AF.
10271033,1063
IIa C
Opportunistic screening for AF should be con-
sidered in patients with OSA.
172
IIa C
Optimal management of OSA may be consid-
ered, to reduce AF incidence, AF progression,
AF recurrences, and
symptoms.
650,651,10571061,1064,1065
IIb C
AF = atrial fibrillation; BP = blood pressure; OAC = oral anticoagulant; OSA =
obstructive sleep apnoea.
a
Class of recommendation.
b
Level of evidence.
Recommendations for management of AF with haemo-
dynamic instability
Recommendations Class
a
Level
b
Emergency electrical cardioversion is recom-
mended in AF patients with acute or worsening
haemodynamic instability.
1053,1054
IB
In AF patients with haemodynamic instability,
amiodarone may be considered for acute con-
trol of heart rate.
503,511,512
IIb B
AF = atrial fibrillation.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 59

precisely. Although the clinical profile and outcome of patients with
first-diagnosed AF in AF registries were less favourable than those
with paroxysmal AF, rather resembling permanent AF,
1055,1056
OAC
prescription rates were the lowest in patients with first-diagnosed
AF.
1057
In patients with first-diagnosed AF, the ABC pathway should
resemble all steps outlined in the Central Illustration.
11.3 Acute coronary syndromes,
percutaneous coronary intervention, and
chronic coronary syndromes in patients
with atrial fibrillation
The incidence of AF in acute coronary syndromes (ACS) ranges from
2-23%,
1058
the risk of new-onset AF is increased by 60 - 77%
1059
in
myocardial infarction patients, and AF per se may be associated with
an increased risk of ST-segment elevation myocardial infarction
(STEMI) or non-STEMI ACS.
381,10601063
Overall, 10 - 15% of AF
patients undergo PCI for CAD.
1064
In observational studies, patients
with AF and ACS were less likely to receive appropriate antithrom-
botic therapy
1065
and more likely to experience adverse out-
comes
1066
than ACS patients without AF.
Peri-procedural management of patients with an ACS or under-
going PCI is detailed in the respective ESC Guidelines on myocardial
revascularization
1067
and chronic coronary syndromes (CCS).
1068
Post-procedural management of atrial fibrillation
patients with acute coronary syndrome and/or
percutaneous coronary intervention
In AF patients having an ACS or undergoing PCI, concomitant risks of
ischaemic stroke/systemic embolism, coronary ischaemic events, and
antithrombotic treatment-related bleeding need to be carefully bal-
anced when considering the use and duration of combined antith-
rombotic therapy.
1069
Overall, dual antithrombotic therapy including
OAC (preferably NOAC) and a P2Y
12
inhibitor (preferably clopidog-
rel) is associated with significantly less major bleeding (and ICH) than
triple therapy. However, available evidence suggests that at least a
short course of triple therapy (e.g. <_1 week) would be desirable in
some AF patients after a recent ACS or undergoing PCI, especially in
those at increased risk of ischaemic events
1070,1071
(Figure 20).
Box 1 About post-procedural manage-
ment of patients with AF and ACS and/
or PCI
Shorter courses of triple therapy (OAC þ DAPT) may be safe in
post-ACS/PCI patients requiring OAC.
1076
Observational data
1077
and the WOEST trial with warfarin (a safety RCT, underpowered for
ischaemic outcomes)
1078
suggested better safety and similar efficacy
with dual (OAC þ clopidogrel) vs. triple therapy.
RCTs of NOACs in AF patients after a recent ACS/PCI
Four RCTs compared dual therapy with a P2Y
12
inhibitor (mostly clo-
pidogrel) plus a NOAC—dabigatran 110 mg or 150 mg b.i.d. (RE-
DUAL PCI),
1079
rivaroxaban 15 mg o.d. (PIONEER AF-PCI),
1080
apix-
aban 5 mg b.i.d. (AUGUSTUS),
1081
or edoxaban 60 mg o.d.
(ENTRUST-AF PCI)
1082
—vs. triple therapy with a VKA in AF
patients with a recent ACS or undergoing PCI. The two-by-two
factorial AUGUSTUS trial design enabled the comparison of
aspirin vs. placebo (see Supplementary Table 12 for detailed
information about these studies). All four trials had a primary safety
endpoint (i.e. bleeding) and were underpowered to assess ischaemic
outcomes.
Despite some heterogeneity among these trials, all have consistently:
•
Included a proportion of patients with an ACS/PCI (37 - 52%);
nevertheless, the highest risk patients (e.g. previous stent throm-
bosis or a complex PCI with stent-in-stent placement) were
largely under-represented;
•
Used triple therapy during PCI and until randomization (1 - 14
days post PCI);
•
Most commonly used the P2Y
12
inhibitor clopidogrel (overall,
>90%); and
•
Reported a significant reduction of major/clinically significant
bleeding, comparable rates of ischaemic stroke, similar or non-sig-
nificantly higher rates of myocardial infarction and stent thrombo-
sis, and a neutral effect on trial-defined major adverse
cardiovascular events and all-cause mortality with dual (NOAC
þ P2Y
12
)vs.triple(VKAþ P2Y
12
þ aspirin) therapy.
In AUGUSTUS,
1081
both placebo (vs. aspirin) and apixaban (vs. VKA)
regimens were associated with significant reduction in bleeding, and
apixaban (vs. VKA) was associated with significantly lower rates of
stroke, death, or hospitalization.
Meta-analyses of RCTs
•
Bleeding outcomes: Meta-analyses
1070,1071,1083,1084
consistently
showed a significant reduction in major bleeding with dual vs. tri-
ple and NOAC- vs. VKA-based therapies (NOAC-based treat-
ments were also associated with a significant reduction in ICH).
•
Ischaemic events: Stroke rates were similar across all treat-
ment arms, but the rates of myocardial infarction and stent
thrombosis were numerically higher with dual vs. triple therapy.
In two meta-analyses
1070,
,
1071
stent thrombosis was statistically
significantly increased on dual (i.e. no aspirin) vs. triple therapy.
Also, the risk of myocardial infarction or stent thrombosis was
slightly higher with dabigatran 110 mg but not dabigatran 150 mg.
•
The trial-defined major adverse cardiovascular events and mortal-
ity rates were similar in all treatment arms, suggesting that the
benefit from major bleeding and ICH reduction is counterbal-
anced by a higher risk for coronary (mainly stent-related) ischae-
mic events with dual therapy.
ACS = acute coronary syndromes; AF = atrial fibrillation; b.i.d. = bis in die
(twice a day); DAPT = dual antiplatelet therapy; ENTRUST-AF PCI =
Edoxaban Treatment Versus Vitamin K Antagonist in Patients With Atrial
Fibrillation Undergoing Percutaneous Coronary Intervention; ICH = intracranial
haemorrhage; NOAC = non-vitamin K antagonist oral anticoagulant; OAC =
oral anticoagulant; o.d. = omni die (once daily); PCI = percutaneous coronary
intervention; PIONEER AF-PCI = (OPen-Label, Randomized, Controlled,
Multicenter Study ExplorIng TwO TreatmeNt StratEgiEs of Rivaroxaban and a
Dose-Adjusted Oral Vitamin K Antagonist Treatment Strategy in Subjects with
Atrial Fibrillation who Undergo Percutaneous Coronary Intervention; RCT =
randomized controlled trial; RE-DUAL PCI = Randomized Evaluation of Dual
Antithrombotic Therapy with Dabigatran vs. Triple Therapy with Warfarin in
Patients with Nonvalvular Atrial Fibrillation Undergoing Percutaneous
Coronary Intervention; VKA = vitamin K antagonist; WOEST = What is the
Optimal antiplatElet and anticoagulant therapy in patients with oral anticoagula-
tion and coronary StenTing.
60 ESC Guidelines

©ESC 2020
Figure 20 Post-procedural management of patients with AF and ACS/PCI (full-outlined arrows represent a default strategy; graded/dashed arrows
show treatment modifications depending on individual patient’s ischaemic and bleeding risks).
Pretreatment with a P2Y
12
inhibitor is recommended in STEMI patients or when coronary anatomy is known; it should be withheld in non-STEMI ACS
until the time of coronary angiography in case of an early invasive strategy within 24 hours. Observational studies indicate that PCI on uninterruptedVKAs
is generally safe compared with OAC interruption and heparin-bridging therapy,
1073
particularly with radial artery access; in contrast, studies on NOACs
are conflicting, predominantly discouraging a PCI on fully uninterrupted NOAC therapy.
1074,1075
If urgent PCI is needed, administration of a parenteral anti-
coagulant (UFH, LMWH, or bivalirudin) is suggested, with temporary withdrawal of NOAC at least for the initial post-procedural period (e.g. 24 h)
depending on the patient’s thrombotic and bleeding risk profile. Where thrombolysis is being considered in a patient with STEMI, the initial step should be
to assess the anticoagulation status (e.g. INR in a patient taking VKA; with a NOAC, assessing, for example, activated partial thromboplastin time on dabiga-
tran or anti-factor Xa activity on factor Xa inhibitors). Thrombolytic therapy may be associated with an increased risk of bleeding in systemically anticoagu-
lated patients, especially if parenteral heparin and antiplatelet drugs are coadministered. A balance between the potential benefit (e.g. large anterior
myocardial infarction) and harm (e.g. ICH) is needed, as well as the reassessment of urgent transfer to a PCI centre. If the supposedly anticoagulated patient
does not have evidence of a therapeutic anticoagulation effect (e.g. INR <2.0 on warfarin; or no NOAC anticoagulant effect detected), systemic thrombol-
ysis may be considered if no access to primary PCI is possible.
ACS = acute coronary syndromes; ASA = acetylsalicylic acid; CAD = coronary artery disease; CCS = chronic coronary syndromes; CKD = chronic kidney
disease; DAPT = dual antithrombotic therapy; eGFR = estimated glomerular filtration rate; ICH = intracranial haemorrhage; INR = international normal-
ized ratio; LMWH = low-molecular-weight heparin; MI = myocardial infarction; NOAC = non-vitamin K antagonist oral anticoagulant; NSAID = non-ster-
oidal anti-inflammatory drug; OAC = oral anticoagulant; PAD = peripheral artery disease; PCI = percutaneous coronary intervention; PPI = proton-pump
inhibitor; STEMI = ST-segment elevation myocardial infarction; UFH = unfractionated heparin; VKA = vitamin K antagonist.
ESC Guidelines 61

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Whichever initial treatment plan was chosen, dual therapy with OAC
and an antiplatelet drug (preferably clopidogrel) is recommended for
the first 12 months after PCI for ACS, or 6 months after PCI in patients
with CCS.
1067
Thereafter, OAC monotherapy is to be continued (irre-
spective of the stent type) provided that there were no recurrent
ischaemic events in the interim. In 1-year event-free (i.e. ‘stable’) AF
patients with CAD and no PCI, OAC monotherapy is also
recommended.
1072
Use of prasugrel or ticagrelor has been associated with a greater risk
of major bleeding compared with clopidogrel
10851089
and should be
avoided in ACS patients with AF. In the RE-DUAL PCI (Randomized
Evaluation of Dual Antithrombotic Therapy with Dabigatran vs. Triple
TherapywithWarfarininPatientswithNonvalvularAtrialFibrillation
Undergoing Percutaneous Coronary Intervention) trial, 12% of patients
received ticagrelor with dabigatran, but experience with ticagrelor or
prasugrel was minimal in PIONEER-AF (OPen-Label, Randomized,
Controlled, Multicenter Study ExplorIng TwO TreatmeNt StratEgiEs of
Rivaroxaban and a Dose-Adjusted Oral Vitamin K Antagonist
Treatment Strategy in Subjects with Atrial Fibrillation who Undergo
Percutaneous Coronary Intervention), AUGUSTUS, and ENTRUST-
AF PCI (Edoxaban Treatment Versus Vitamin K Antagonist in Patients
With Atrial Fibrillation Undergoing Percutaneous Coronary
Intervention). In patients at potential risk of gastrointestinal bleeding,
concomitant use of proton-pump inhibitors is reasonable.
1084
In AF patients treated with surgical coronary revascularization,
OAC should be resumed as soon as bleeding is controlled, possibly in
combinationwithclopidogrel,andtripletherapyshouldbeavoided.
Poor ventricular rate control during AF may exacerbate symptoms
of myocardial ischaemia and precipitate or worsen HF. Appropriate
treatment may include a beta-blocker or rate-limiting calcium
antagonist. In haemodynamic instability, acute cardioversion may be
indicated. Vernakalant, flecainide, and propafenone should not be used
for rhythm control in patients with known CAD (section 10.2.2.2).
In all AF patients with an ACS/CCS, optimized management of risk
factors is needed, and cardiovascular prevention strategies such as
good BP control,
338
lipid management, and other cardiovascular pre-
vention interventions
1007
should be implemented as needed, once
the acute presentation is stabilized.
Recommendations for patients with AF and an ACS, PCI, or CCS
1068
General recommendations for patients with AF and an indication for concomitant antiplatelet therapy Class
a
Level
b
In AF patients eligible for NOACs, it is recommended to use a NOAC
c
in preference to a VKA in combination with antiplatelet
therapy.
1079,1081
IA
In patients at high bleeding risk (HAS-BLED >_3), rivaroxaban 15 mg o.d. should be considered in preference to rivaroxaban 20 mg
o.d. for the duration of concomitant single or DAPT, to mitigate bleeding risk.
1080
IIa B
In patients at high bleeding risk (HAS-BLED >_3), dabigatran 110 mg b.i.d. should be considered in preference to dabigatran 150 mg
b.i.d. for the duration of concomitant single or DAPT, to mitigate bleeding risk.
1079
IIa B
In AF patients with an indication for a VKA in combination with antiplatelet therapy, the VKA dosing should be carefully regulated
with a target INR of 2.0 - 2.5 and TTR>70%.
1094,1095,1104,1105
IIa B
Recommendations for AF patients with ACS
In AF patients with ACS undergoing an uncomplicated PCI, early cessation (<_1 week) of aspirin and continuation of dual therapy with an
OAC and a P2Y
12
inhibitor (preferably clopidogrel) for up to 12 months is recommended if the risk of stent thrombosis
d
is low or if con-
cerns about bleeding risk
e
prevail over concerns about risk of stent thrombosis,
d
irrespective of the type of stent used.
1090,10921095
IB
Triple therapy with aspirin, clopidogrel, and an OAC
f
for longer than 1 week after an ACS should be considered when risk of stent
thrombosis
d
outweighs the bleeding risk,
e
with the total duration (<_1 month) decided according to assessment of these risks, and the
treatment plan should be clearly specified at hospital discharge.
IIa C
Recommendations in AF patients with a CCS undergoing PCI
After uncomplicated PCI, early cessation (<_1 week) of aspirin and continuation of dual therapy with OAC for up to 6 months and
clopidogrel is recommended if the risk of stent thrombosis
d
is low or if concerns about bleeding risk
e
prevail over concerns about
risk of stent thrombosis,
d
irrespective of the type of stent used.
1076,10781081
IB
Triple therapy with aspirin, clopidogrel, and an OAC
f
for longer than 1 week should be considered when risk of stent thrombosis
d
outweighs the bleeding risk,
e
with the total duration (<_1 month) decided according to assessment of these risks, and the treatment
plan should be clearly specified at hospital discharge.
IIa C
ACS = acute coronary syndrome; AF = atrial fibrillation; b.i.d. = bis in die (twice a day); CCS = chronic coronary syndrome; CKD = chronic kidney disease; DAPT = Dual anti-
platelet therapy; HAS-BLED = Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile INR, Elderly (>65 years), Drugs/alcohol concomi-
tantly; INR = international normalized ratio; NOAC = non-vitamin K antagonist oral anticoagulant; o.d. = omni die (once daily); OAC = oral anticoagulant; PCI=percutaneous
coronary intervention; TTR = time in therapeutic range; VKA = vitamin K antagonist.
a
Class of recommendation.
b
Level of evidence.
c
See summary of product characteristics for reduced doses or contraindications for each NOAC in patients with CKD, body weight <60 kg, age >75 - 80 years, and/or drug
interactions.
d
Risk of stent thrombosis encompasses: (i) risk of thrombosis occurring, and (ii) risk of death should stent thrombosis occur, both of which relate to anatomical, procedural,
and clinical characteristics. Risk factors for CCS patients include: stenting of left main stem or last remaining patent artery; suboptimal stent deployment; stent length >60 mm;
diabetes mellitus; CKD; bifurcation with two stents implanted; treatment of chronic total occlusion; and previous stent thrombosis on adequate antithrombotic therapy.
e
Bleeding risk in AF patients may be assessed using the HAS-BLED score (section 10.1.2), which draws attention to modifiable bleeding risk factors; those at high risk (score >_3)
can have more frequent or early review and follow-up. Bleeding risk is highly dynamic and does not remain static, and relying on modifiable bleeding risk factors alone is an infe-
rior strategy to evaluate bleeding risk.
389
f
When dabigatran is used in triple therapy, dabigatran 110 mg b.i.d may be used instead of 150 mg b.i.d, but the evidence is insufficient.
62 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
11.4 Acute stroke or intracranial
haemorrhage in patients with atrial
fibrillation
11.4.1 Patients with atrial fibrillation and acute
ischaemic stroke or transient ischaemic attack
Management of acute stroke in AF patients is beyond the scope of
this document. In AF patients presenting with acute ischaemic
stroke while taking OAC, acute therapy depends on the treatment
regimen and intensity of anticoagulation. Patients on VKA with an
INR<1.7 are eligible for thrombolysis according to the neurologi-
cal indication (if presenting with a clinically relevant neurological
deficit within the appropriate time window and ICH is excluded
with cerebral imaging). In patients taking NOACs, measurement
of activated partial thromboplastin time or thrombin time (for
dabigatran), or antifactor Xa levels (for factor Xa inhibitors) will
provide information on whether the patient is systemically antico-
agulated. Whenever possible, the time when the last NOAC dose
was taken should be elucidated (generally, thrombolysis is consid-
ered to be safe in patients with last NOAC intake being >_48 h,
assuming normal renal function).
1090
If the patient is systemically anticoagulated, thrombolysis should
not be performed due to the risk of haemorrhage, and endovascular
treatment should be considered. In patients taking dabigatran, sys-
temic thrombolysis may be performed after reversal of the dabiga-
tran action by idarucizumab.
1091
Secondary prevention of stroke/systemic embolism in patients
after acute AF-related ischaemic stroke or TIA includes early
prevention of recurrent ischaemic stroke in the 2 weeks after the
index event and long-term prevention thereafter
Whereas infarct size/stroke severity is used clinically to guide tim-
ing of OAC initiation,
1090
the usefulness of such an approach in esti-
mating the net benefit of early treatment may be limited. Robust data
to inform optimal timing for (re)initiation of OAC after acute stroke
are lacking. From the cardiological perspective, OAC should be
(re)initiated as soon as considered possible from the neurological
perspective (in most cases within the first 2 weeks). A multidiscipli-
nary approach with involvement of stroke specialists, cardiologists,
and patients is considered appropriate.
In AF patients who presented with acute ischaemic stroke despite
taking OAC, optimization of OAC therapy is of key importance—if
on VKA, optimize TTR (ideally >70%) or switch to a NOAC; if on
NOAC, ensure appropriate dosing and good adherence to treat-
ment. Inappropriate NOAC under-dosing using lower or reduced
doses of specific NOACs has been associated with increased risk of
stroke/systemic embolism, hospitalization, and deaths without appre-
ciable reduction in major bleeding.
1107
11.4.2 Cryptogenic stroke/embolic stroke with
undetermined source
Currently available evidence including two recently completed
RCTs
1108,1109
does not support routine OAC use in patients with
acute ischaemic stroke of uncertain aetiology (cryptogenic stroke)
or acute embolic stroke of undetermined source in patients wi th-
out documented AF (Supplementary Box 4). Of note, subgroup
Box 2 About acute ischaemic stroke in patients with AF
AF-related ischaemic strokes are often fatal or disabling
106
, with increased risk of early recurrence within 48 h
1092
to 2 weeks,
10921095
or haemorrhagic trans-
formation,
1096
especially in the first days after large cardio-embolic lesions and acute recanalization therapy.
1097,1098
Notably, ICH is generally associated with
higher mortality and morbidity than recurrent ischaemic stroke.
Timing of OAC (re)initiation after acute ischaemic stroke
•
Early anticoagulation after acute ischaemic stroke might cause parenchymal haemorrhage, with potentially serious clinical consequences
1097,
.
1099
Using UFH,
LMWH, heparinoids, or VKAs <48 h after acute ischaemic stroke was associated with an increased risk of symptomatic ICH, without significant reductionin
recurrent ischaemic stroke.
1095
•
Reportedly, the 90-day risk of recurrent ischaemic stroke outweighs the risk of symptomatic ICH in AF patients receiving a NOAC 4 - 14 days after the acute
event
11001102
(ischaemic stroke recurrence rates after mild/moderate ischaemic stroke significantly increased with a later NOAC administration,
1101
e.g. >14
days).
1100
In a small RCT, rivaroxaban use within 5 days after mild ischaemic stroke in AF patients was associated with similar event rates compared with VKA.
1103
As high-quality RCT-derived evidence to inform optimal timing of anticoagulation after acute ischaemic stroke is lacking, OAC use in the early post-stroke period
is currently based on expert consensus.
505
Several ongoing RCTs [ELAN (NCT03148457), OPTIMAS (EudraCT, 2018-003859-3), TIMING (NCT02961348), and
START (NCT03021928)] are investigating early (<1 week) vs. late NOAC initiation in patients with AF-related ischaemic stroke (first results are not expected
before 2021).
Long-term secondary stroke prevention
•
There is no evidence that the addition of aspirin to OAC or supratherapeutic INRs would improve outcomes in secondary stroke prevention.
•
Compared with VKAs, NOACs were associated with better efficacy in secondary stroke prevention and better safety regarding ICH in a meta-analysis of
landmark NOAC AF trial.
1104
•
Good adherence to OAC treatment is essential for effective secondary stroke prevention.
There is some evidence to support that strokes can induce AF through neurogenic mechanisms
1105,
.
1106
The first study showed that damage to the insula
increases the odds of AF detection after ischaemic stroke and is more prevalent in patients with AF diagnosed after stroke than among those without AF.
1105
The second study explained the reason why AFDAS detected soon after ischaemic stroke is associated with a low risk of ischaemic stroke recurrence.
1106
AF = atrial fibrillation; ELAN = Early versus Late Initiation of Direct Oral Anticoagulants in Post-ischaemic Stroke Patients With AF; ICH = intracranial haemor-
rhage; INR = international normalized ratio; LMWH = low-molecular-weight heparin; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral antico-
agulant; OPTIMAS = OPtimal TIMing of Anticoagulation after Stroke; RCT = randomized controlled trial; START = Optimal Delay Time to Initiate
Anticoagulation After Ischemic Stroke in AF; TIMING = TIMING of Oral Anticoagulant Therapy in Acute Ischemic Stroke With AF; UFH = unfractionated hepa-
rin; VKA = vitamin K antagonist.
ESC Guidelines 63

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
analyses of those two RCTs suggested that certain subgroups (i.e.
age >_75 years, impaired renal function,
1109
or enlarged LA
1110
)
could benefit from OAC, but more data are needed to inform
optimal use of NOACs among patients with a cryptogenic stroke.
Two ongoing trials will study the use of apixaban in this setting
[ATTICUS (Apixaban for treatment of embolic stroke of undeter-
mined source)]
1111
and ARCADIA [(AtRial Cardiopathy and
Antithrombotic Drugs In Prevention After Cryptogenic Stroke)
(NCT03192215)].
Efforts to improve detection of AF are needed in such patients
(see also section 8). Clinical risk scores f e.g. C
2
HEST [CAD/COPD
(1 point each), Hypertension (1 point), Elderly ( >_75 years, 2 points),
Systolic heart failure (2 points), and Thyroid disease (hyperthyroid-
ism, 1 point) (score)]g have been proposed for identification of ‘high-
risk’ patients for AF diagnosis
1112
and facilitation of prolonged
monitoring.
11.4.3 Post-stroke patients without known atrial
fibrillation
Detection of previously unknown AF after stroke has important
implications for secondary prevention. Several RCTs have established
the effectiveness of ECG monitoring for post-stroke AF detection,
with numbers needed to screen of 8 14.
1117,1118
Looking harder and longer and using more sophisticated moni-
toring may generally improve AF detection. In a meta-analysis
1118
of 50 post-stroke studies, the proportion of patients with post-
stroke AF was 7.7% in the emergency room using admission ECG;
5.1% in the wards using serial ECG, continuous inpatient ECG
monitoring/cardiac telemetry, and in-hospital Holter monitoring;
10.7% in the first ambulatory period using ambulatory Holter; and,
after discharge, 16.9% using mobile cardiac outpatient telemetry
and external or implantable loop recording. The overall post-
stroke AF detection after all phases of cardiac monitoring reached
23.7%.
1118
In patients with ischaemic stroke/TIA, monitoring for AF is recom-
mended by short-term ECG recording followed by continuous ECG
monitoring for at least 72 h, also considering a tiered longer ECG
monitoring approach
1113
and insertion of an intracardiac monitor in
case of cryptogenic stroke.
1114,1119
Post-stroke ECG monitoring is
likely cost-effective
1120,1121
; however, RCTs have not been powered
to assess the effect of prolonged ECG monitoring and subsequent
prescription of OAC on stroke or mortality in patients with detected
AF.
11.4.4 Management of patients with atrial fibrillation
post-intracranial haemorrhage
As ICH is the most feared, often lethal, complication of anticoagulant
and antiplatelet therapy, there is a considerable reluctance to (re)ini-
tiate OAC in AF patients who survived an ICH, despite their high esti-
mated risk of AF-related ischaemic stroke.
Patients with a history of recent ICH were excluded from RCTs of
stroke prevention in AF, but available observational data suggest than
many AF patients would benefit from (re)institution of OAC,
depending on the cause(s) of ICH and findings on brain CT and MRI
(Supplementary Box 5).
Treatment decision to (re)start OAC in AF patients after an ICH
requires multidisciplinary-team input from cardiologists, stroke spe-
cialists, neurosurgeons, patients, and their family/carers. After acute
spontaneous ICH (which includes epidural, subdural, subarachnoid,
or intracerebral haemorrhage), OAC may be considered after careful
assessment of risks and benefits, and cerebral imaging may help. The
risk of recurrent ICH may be increased in the presence of specific
risk factors, shown in Figure 21. Of note, the risk of OAC-related ICH
is increased especially in Asian patients.
1122
Compared with VKAs, the use of NOACs in patients without pre-
vious ICH is associated with an approximately 50% lower risk of
ICH,
423
whereas the size and outcome of OAC-related ICH is similar
with NOACs and VKAs.
1124
Hence, NOACs should be preferred in
NOAC-eligible ICH survivors with AF although there is no RCT to
prove this.
The optimal timing of anticoagulation after ICH is unknown, but
should be delayed beyond the acute phase, probably for at least 4
weeks; in AF patients at very high risk of recurrent ICH, LAA occlu-
sion may be considered. Ongoing RCTs of NOACs and LAA occlu-
sion may inform decision making in the future.
Recommendations for the search for AF in patients
with cryptogenic stroke
Recommendations Class
a
Level
b
In patients with acute ischaemic stroke or TIA
and without previously known AF, monitoring
for AF is recommended using a short-term ECG
recording for at least the first 24 h, followed by
continuous ECG monitoring for at least 72 h
whenever possible.
11131116
IB
In selected
c
stroke patients without previously
known AF, additional ECG monitoring using
long-term non-invasive ECG monitors or insert-
able cardiac monitors should be considered, to
detect AF.
1112
IIa B
AF = atrial fibrillation; C
2
HEST = CAD/COPD (1 point each), Hypertension (1
point), Elderly ( >_75 years, 2 points), Systolic heart failure (2 points), and Thyroid
disease (hyperthyroidism, 1 point) (score); ECG=electrocardiogram; LA = left
atrial; TIA=transient ischaemic attack.
a
Class of recommendation.
b
Level of evidence.
c
Not all stroke patients would benefit from prolonged ECG monitoring; those
deemed at risk of developing AF (e.g. elderly, with cardiovascular risk factors or
comorbidities, indices of LA remodelling, high C
2
HEST score, etc.) or those with
cryptogenic stroke and stroke characteristics suggestive of an embolic stroke
should be scheduled for prolonged ECG monitoring.
64 ESC Guidelines

©ESC 2020
Figure 21 (Re-) initiation of anticoagulation post-intracranial bleeding.
A pooled analysis of individual patient data from cohort studies (n=20 322 patients; 38 cohorts; >35 225 patient-years) showed that although cerebral
microbleeds can inform regarding the risk for ICH in patients with recent ischaemic stroke/TIA treated with antithrombotic therapy, the absolute risk of
ischaemic stroke is substantially higher than that of ICH, regardless of the presence, burden, or location of cerebral microbleeds.
505,1123
IS = ischaemic stroke;ACS = acute coronary syndrome; CMB = cerebral microbleeds; ICH = intracranial haemorrhage; LAA = left atrial appendage; LDL
= low-density lipoprotein; LoE = level of evidence; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagulant; PCI = percutaneous
coronary intervention; RCT = randomized controlled trial; TIA = transient ischaemic attack.
Recommendations for secondary stroke prevention in AF patients after acute ischaemic stroke Class
a
Level
b
In AF patients with an ischaemic stroke or TIA, long-term secondary prevention of stroke using OAC is recommended if there is no
strict contraindication to OAC use, with a preference for NOACs over VKAs in NOAC-eligible patients.
11251130
IA
In AF patients presenting with acute ischaemic stroke, very early anticoagulation (<48 h) using UFH, LMWH, or VKAs is not
recommended.
1095
III B
Recommendations for stroke prevention in AF patients after intracranial haemorrhage
In AF patients at high risk of ischaemic stroke, (re-)initiation of OAC, with preference for NOACs over VKAs in NOAC-eligible
patients, should be considered in consultation with a neurologist/stroke specialist after:
•
A trauma-related ICH
•
Acute spontaneous ICH (which includes subdural, subarachnoid, or intracerebral haemorrhage), after careful consideration of risks
and benefits.
c
IIa C
AF = atrial fibrillation; ICH = intracranial haemorrhage; LMWH = low-molecular-weight heparin; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagu-
lant; TIA = transient ischaemic attack; UFH = unfractionated heparin; VKA = vitamin K antagonist.
a
Class of recommendation.
b
Level of evidence.
c
A more favourable net benefit is likely with deep ICH or without neuroimaging evidence of cerebral amyloid angiopathy or microbleeds.
ESC Guidelines 65

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
11.5 Active bleeding on anticoagulant
therapy: management and reversal
drugs
Management of patients with active bleeding while on OAC is shown
in Figur e 22. General assessment should include detection of the
bleeding site, assessment of bleeding severity, and evaluation of the
time-point of last OAC intake. Concomitant antithrombotic drugs
and other factors influencing bleeding risk (alcohol abuse, renal func-
tion) should be explored. Laboratory tests, such as INR, are useful in
case of VKA therapy. More specific coagulation tests for NOACs
include diluted thrombin time, ecarin clotting time, or ecarin chromo-
genic assay for dabigatran, and chromogenic anti-factor Xa assay for
rivaroxaban, apixaban, and edoxaban.
1131
However, these tests or
measurement of NOAC plasma levels are not always readily available
in practice and are often unnecessary for bleeding management.
1132
An overview of reversal drugs for NOACs is given in Supplementary
Table 13 and Sup plementary Figure 6.
Notably, the time of last drug ingestion combined with assessment
of renal function, haemoglobin, haematocrit, and platelet count ena-
ble appropriate clinical decision making in most of the cases.
Minor bleeding events should be treated with supportive measures
such as mechanical compression or minor surgery to achieve haemo-
stasis. Withdrawal of VKAs is not associated with a prompt reduction
of anticoagulant effect, while NOACs have a short plasma half-life
and haemostasis can be expected within 12 - 24 h after an omitted
dose.
Treatment of moderate bleeding events may require blood trans-
fusions and fluid replacement. If the last intake of NOACs was less
than 2 - 4 h before bleeding assessment, charcoal administration and/
or gastric lavage will reduce further exposure. Specific diagnostic and
treatment interventions to identify and manage the cause of bleeding
(e.g. gastroscopy) should be performed promptly. Dialysis is effective
in reducing dabigatran concentration and has been associated with
reduction in the duration and/or severity of associated bleeding.
1133
Severe or life-threatening bleeding requires immediate reversal of
the antithrombotic effect of OACs. For VKAs, administration of fresh
frozen plasma restores coagulation more rapidly than vitamin K, but
prothrombin complex concentrates achieve even faster blood coagu-
lation
1134
and are first-line therapy for VKA reversal.
1135
Specific
reversal drugs are available for NOACs: idarucizumab (for dabiga-
tran) and andexanet alfa (for factor Xa inhibitors) effectively reverse
the anticoagulation action of NOACs and restore physiological hae-
mostasis.
1136,1137
However, their use is often associated with subse-
quent non-reinitiation of OAC and increased rates of thrombotic
events. These drugs can be effectively applied in case of severe life-
threatening bleeding or urgent surgery, but their use is only very
rarely necessary in daily clinical practice. Ciraparantag is an investiga-
tional synthetic drug that binds and inhibits direct factor Xa inhibitors,
dabigatran, and heparin. The use of four-factor prothrombin complex
concentrates may be considered as an alternative treatment for
reversing the anticoagulant effect of rivaroxaban, apixaban, and edox-
aban, although scientific evidence is very limited in this context and is
frequently from healthy volunteers.
11381140
©ESC 2020
Figure 22 Management of active bleeding in patients receiving anticoagulation (institutions should have an agreed procedure in place).
143
FFP = fresh
frozen plasma; INR = international normalized ratio; i.v. = intravenous; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagulation
therapy; PCC = prothrombin complex concentrates; VKA = vitamin K antagonist.
66 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
11.6 Atrial fibrillation and heart failure
Both AF and HF facilitate the occurrence and aggravate the prognosis
of each other, and often coexist (see also sections 4.2 and 5.3); HF is
also a thrombo-embolic risk factor in AF. The efficacy and safety of
NOACs do not seem to differ in AF patients with and without
HF.
1141,1142
The management of patients with AF and HF is often challenging
(section 10.2). The optimal heart-rate target in AF patients with HF
remains unclear, but a rate of <100 - 110 bpm is usually recommen-
ded.
11431145
Pharmacological rate control strategies are different
for patients with heart failure with preserved ejection fraction
(HFpEF) and HFrEF. Beta-blockers, diltiazem, verapamil, and digoxin
are all viable options in HFpEF, while beta-blockers and digoxin can
be used in those with HFrEF. Amiodarone may be considered for
rate control in both forms of HF, but only in the acute setting.
Atrioventricular-node ablation and pacing can control ventricular
rate when medication fails (section 10.2.1.). However, in an observa-
tion study, rhythm control strategies showed a lower 1-year all-cause
death over rate control in older patients (>_65 years) with HFpEF.
1146
Haemodynamic instability or worsening of HF may require emer-
gency or immediate electrical cardioversion of AF, whereas pharma-
cological cardioversion using i.v. amiodarone may be attempted if a
delayed cardioversion is consistent with the clinical situation (section
10.2.2.2.2). AF catheter ablation has been shown to improve symp-
toms, exercise capacity, QoL, and LVEF in AF patients with HF,
661
whereas the recent CASTLE-AF RCT showed a reduction in all-
cause mortality and hospitalization for worsening HF after AF cathe-
ter ablation in patients with HFrEF
657
(section 10.2.2.3).
All patients with HF and AF should receive guideline-adherent HF
therapy.
1145
The benefit of beta-blocker therapy in reducing
mortality in AF patients with HFrEF has been questioned by some
meta-analyses,
491
although this is not a universal finding, especially
with some real-world studies supporting an improved
prognosis.
1147,1148
11.7 Atrial fibrillation and valvular heart
disease
VHD is independently associated with AF
1149
and more than one-
third of patients with AF have some form of VHD.
512
Among patients with severe VHD, including those undergoing sur-
gical and transcatheter aortic or mitral valve intervention, AF is asso-
ciated with less favourable clinical outcomes.
11501155
Compared to
AF patients without VHD, the risk of thrombo-embolism and stroke
is increased among AF patients with VHD other than mitral stenosis
and mechanical heart prostheses, mostly owing to older age and
more frequent comorbidities.
1156,1157
While patients with moderate-
to-severe mitral stenosis and mechanical prosthetic heart valves
require anticoagulation with VKAs,
1158
there is no evidence that the
presence of other VHDs including aortic stenosis/regurgitation,
mitral regurgitation, bioprostheses, or valve repair should modify the
choice of OAC.
1156,1159
In a meta-analysis of the four pivotal RCTs
comparing NOACs with VKAs, the effects of NOACs vs. VKAs in
terms of stroke/systemic embolism and bleeding risk in patients with
VHD other than mitral stenosis and mechanical prosthetic heart
valves were consistent with those in the main RCTs.
1160
In an obser-
vational study, NOACs were associated with better outcomes, with
reduced rates of ischaemic stroke and major bleeding compared to
warfarin in AF patients with mitral stenosis.
1161
Recently, a functional categorization of VHD in relation to OAC
use was introduced, categorizing patients with moderate-severe or
rheumatic mitral stenosis as type 1 and all other VHD as type
2.
148,1157,1162
There are gaps in evidence on NOAC use in AF
patients with rheumatic mitral valve disease, and during the first
3 months after surgical or transcatheter implantation of a bioprosthe-
sis, and observational data regarding NOACs use after transcatheter
aortic valve implantation are conflicting.
1163
An RCT in non-AF
patients comparing rivaroxaban 10 mg daily with aspirin after trans-
catheter aortic valve implantation was stopped early due to higher
risks of death or thrombo-embolic complications and bleeding in the
rivaroxaban arm.
1164
Recommendations for the management of active bleed-
ing on OAC
Class
a
Level
b
In an AF patient with severe active bleeding, it is
recommended to:
•
Interrupt OAC until the cause of bleeding is
identified and active bleeding is resolved; and
•
Promptly perform specific diagnostic and
treatment interventions to identify and man-
age the cause(s) and source(s) of bleeding.
IC
Four-factor prothrombin complex concentrates
should be considered in AF patients on VKA
who develop a severe bleeding complication.
IIa C
AF = atrial fibrillation; OAC = oral anticoagulant; VKA=vitamin K antagonist.
a
Class of recommendation.
b
Level of evidence.
Recommendations for patients with valvular heart dis-
ease and AF
Recommendations Class
a
Level
b
NOACs are contraindicated in patients with a
prosthetic mechanical valve.
1165
III B
Use of NOACs is not recommended in patients
with AF and moderate-to-severe mitral stenosis.
III C
AF = atrial fibrillation; NOAC = non-vitamin K antagonist oral anticoagulant.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 67

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
11.8 Atrial fibrillation and chronic kidney
disease
Independently of AF, CKD is a prothrombotic and prohaemorrhagic
condition (Supplementary Figure 7),
1166,1167,1168
and AF may acceler-
ate CKD progression. Coexisting in 1520% of CKD patients,
1169
AF is associated with increased mortality,
1170
whereas CKD may be
present in 40 - 50% of AF patients.
1171
In AF patients, renal function
can deteriorate over time,
1172
and worsening CrCl is a better inde-
pendent predictor of ischaemic stroke/systemic embolism and bleed-
ing than renal impairment per se.
1172
In RCTs of OAC for stroke
prevention in AF, renal function was usually estimated using the
CockcroftGault formula for CrCl, and a CrCl cut-off of <50 mL/
min was used to adapt NOAC dosage.
In patients with mild-to-moderate CKD (CrCl 30 - 49 mL/min),
the safety and efficacy of NOACs vs. warfarin was consistent with
patients without CKD in landmark NOAC trials
11731176
, hence the
same considerations for stroke risk assessment and choice of OAC
may apply.
In patients with CrCl 15 - 29 mL/min, RCT-derived data on the
effect of VKA or NOACs are lacking. These patients were essentially
excluded from the major RCTs. The evidence for the benefits of
OAC in patients with end-stage kidney disease with CrCl<_15 mL/
min or on dialysis is even more limited, and to some extent contro-
versial. There are no RCTs, whereas observational data question the
benefit of OAC in this patient population. Data from observational
studies suggest possible bleeding risk reduction in patients with end-
stage kidney disease taking a NOAC compared with VKA,
435,1177
but
there is no solid evidence for a reduction in embolic events with
either NOACs or VKAs, as recently shown in a systematic
review.
1178
Notably, NOACs have not been approved in Europe for
patients with CrCl <_15 mL/min or on dialysis.
Several RCTs are currently assessing OAC use and comparing
NOACs with VKAs in patients with end-stage renal disease
(NCT02933697, NCT03987711). The RENAL-AF trial, investigating
apixaban vs. warfarin in AF patients on haemodialysis, was terminated
early with inconclusive data on relative stroke and bleeding rates.
1179
There are no RCT data on OAC use in patients with AF after kid-
ney transplantation. The prescription and dosing of NOACs should
be guided by the estimated glomerular filtration rate of the trans-
planted kidney and taking into account potential interactions with
concomitant medication.
Particular attention must be given to the dosing of NOACs in
patients with CKD (Supplementary Table 9).
11.9 Atrial fibrillation and peripheral
artery disease
Patients with AF often have atherosclerotic vascular disease. With
the inclusion of asymptomatic ankle-brachial index<_0.90 in the defini-
tion PAD, the prevalence of vascular disease increased signifi-
cantly.
1180
In a systematic review and meta-analysis, the presence of
PAD was significantly associated with a 1.3- to 2.5-fold increased risk
of stroke.
347
Complex aortic plaque in the descending aorta, as iden-
tified on TOE, is also a significant vascular stroke risk factor (section
10.1.1).
In patients with asymptomatic PAD, the risk of cardiovascular
events progressively increases with increasing vascular disease
burden.
470
Therefore, PAD patients should be opportunistically
screened for AF. Patients with AF and PAD should be prescribed
OAC, unless contraindicated. Those with stable vascular disease
(arbitrarily defined as no new vascular event in the past 12 months)
should be managed with OAC alone (section 11.3), as concomitant
use of antiplatelet therapy has not been shown to reduce stroke or
other cardiovascular events, but may increase serious bleeds, includ-
ing ICH.
The principles of rate and rhythm control outlined in section 10.2
also apply for AF patients with PAD. Special considerations include
possibly limited exercise capacity in these patients, owing to intermit-
tent claudication. Beta-blockers may exacerbate PAD symptoms in
some patients, in whom NDCC blockers may be more appropriate
for rate control.
11.10 Atrial fibrillation and endocrine
disorders
Electrolyte disturbances and altered glucose and/or hormone levels
in endocrine disorders such as thyroid disorders, acromegaly, pheo-
chromocytoma, diseases of adrenal cortex, parathyroid disease, or
pancreas dysfunction including diabetes mellitus may contribute to
development of AF. Data on management of AF in these settings are
limited.
3
Diabetes is discussed in section 10.3.2.4. Stroke prevention
should follow the same principles as in other AF patients, with risk
stratification using the CHA
2
DS
2
-VASc score.
3,1181
In AF patients
with hyperthyroidism, spontaneous conversion of AF often occurs
once a euthyroid state is achieved.
1182
Withdrawal of amiodarone is
mandatory in hyperthyroidism. AF catheter ablation should be per-
formed under stable electrolytic and metabolic conditions and should
not be carried out during active hyperthyroidism.
11.11 Atrial fibrillation and
gastrointestinal disorders
While gastrointestinal lesions can lead to bleeding events in anticoa-
gulated AF patients, some gastrointestinal conditions such as active
inflammatory bowel disease increase the risk of AF and stroke.
1183
Gastrointestinal bleeding is a well-known complication of OAC.
Overall, NOAC use is associated with an increased risk of gastroin-
testinal bleeding,
1184,1185
but in patients treated with apixaban or
dabigatran 110 mg the risk is similar to warfarin.
419,421
Bleeding
lesions can be identified in more than 50% of cases of major gastroin-
testinal bleeding.
1186
After correction of the bleeding source, OAC
should be restarted, as this strategy has been associated with
decreased risks of thrombo-embolism and death.
1187
Patients treated with dabigatran may experience dyspepsia (about
11% in the RE-LY trial, and 2% discontinued the drug because of gas-
trointestinal symptoms
419
). After-meal ingestion of dabigatran and/or
the addition of proton-pump inhibitors improves symptoms.
1188
Management of AF patients with liver disease is challenging, owing
to increased bleeding risk (associated with decreased hepatic syn-
thetic function in advanced liver disease, thrombocytopenia, and gas-
trointestinal variceal lesions), as well as increased ischaemic
risk
1189,1190
). Patients with hepatic dysfunction were generally
excluded from the RCTs,
1191
especially those with abnormal clotting
tests, as such patients may be at higher risk of bleeding on VKA, possi-
bly less so on NOACs. Despite the paucity of data, observational
68 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
studies did not raise concerns regarding the use of NOACs in
advanced hepatic disease.
1192
In a recent study, AF patients with liver
fibrosis had no increase in bleeding on NOACs compared with
VKAs.
470
Other reassuring data for NOACs come from a large
nationwide cohort.
472
A number of patients may be started on a
NOAC while having unrecognized significant liver damage and, in cir-
rhotic patients, ischaemic stroke reduction may outweigh bleeding
risk.
471
NOACs are contraindicated in patients within Child-
Turcotte-Pugh C hepatic dysfunction, and rivaroxaban is not recom-
mended for patients in the Child-Turcotte-Pugh B or C category.
1193
11.12 Atrial fibrillation and
haematological disorders
Anaemia is an independent predictor of OAC-related major bleed-
ing.
393,402
In a population-based AF cohort, anaemia was associated
with major bleeding and lower TTR, whereas OAC use in AF patients
with moderate or severe anaemia was associated with more major
bleeding but no reduction in thrombo-embolic risk.
1194
Thrombocytopenia is also associated with increased bleeding risk.
Before and during anticoagulation treatment, both anaemia and
thrombocytopenia should be investigated and corrected, if possible.
Decision making on OAC use in patients with platelet counts <100/
mL requires a multidisciplinary approach including haematologists,
balancing thrombotic and bleeding risks and addressing modifiable
bleeding risk factors. Some chemotherapeutic drugs may increase the
risk of incident AF (e.g. ibrutinib, melphalan, anthracyclines)
11951197
or impair platelet function, thus increasing the risk of bleeding (e.g.
ibrutinib).
1198,1199
11.13 The elderly and frail with atrial
fibrillation
The prevalence of AF increases progressively with age
67,12001206
,
and age is an independent risk factor for adverse outcomes in
AF.
372,1200,1207,1208
Older people are less likely to receive
OAC
12091216
despite sufficient evidence supporting the use of
OAC in this population. Frailty, comorbidities, and increased risk of
falls
12171219
do not outweigh the benefits of OAC given the small
absolute risk of bleeding in anticoagulated elderly
patients.
339,390,391,12201223
Evidence from RCTs,
441,1224
meta-analy-
ses
423,1225
and large registries
339,433,1209,1226
support the use of OAC
in this age group. Antiplatelets are neither more effective nor safer
than warfarin and may even be harmful,
433
whereas NOACs appear
to have a better overall riskbenefit profile compared with
warfarin.
423,433,441,1035,1225,12271236
Prescribing a reduced dose of
OAC is less effective in preventing AF adverse
outcomes.
1107,1211,1237,1238
Rate control is traditionally the preferred strategy, but evidence
informing the choice between rate and rhythm control in the elderly
is insufficient.
12391242
Limited evidence on other AF treatments sup-
ports the use of all rate and rhythm control options, including cardio-
version, pacemaker implantation, and AF catheter ablation without
any age discrimination. AF catheter ablation may be an effective and
safe option in selected older individuals with success rates compara-
ble to younger patients
12431255
and acceptable complication rate-
s.
1243,12451247,12491260
Nevertheless, age was a predictor of
complications in AF catheter ablation in some studies
12611263
and
longer follow-up studies suggested an age-related increase in
multivariable-adjusted risk for AF/AFL recurrence, death, and major
adverse cardiac events.
1257
11.14 Patients with cognitive
impairment/dementia
Evidence regarding effective prevention of cognitive impairment in
AF is derived mainly from observational studies, suggesting that OAC
could play a protective role in AF patients with stroke risk factors,
not only for stroke prevention but also for prevention of cognitive
decline.
1264
The quality of anticoagulation with VKAs (i.e. TTR) seems
to play an additional role: low TTR and supratherapeutic INR values
were associated with higher risk of dementia.
1265,1266
Limited evi-
dence suggests that NOACs may be superior to VKA for preventing
cognitive impairment in some,
1267,1268
but not all, studies.
1269
Recent
observational data indicate a protective effect of OAC even in low-
risk AF patients who do not need OAC for stroke prevention.
1270
A
number of RCTs with cognitive function as an endpoint are ongoing
and will provide more insights into the role of anticoagulation
(NOACs and VKAs) for prevention of cognitive impairment in AF.
86
Conversely, cognitive impairment can influence treatment adher-
ence,
1271,1272
thus affecting outcomes in AF patients. After AF cathe-
ter ablation, silent brain lesions are detected by MRI, but this has not
led to cognitive impairment in the AXAFAAFNET 5 trial, although
underpowered.
880
11.15 Atrial fibrillation and congenital
heart disease
Survival of patients with congenital heart disease has increased over
time, but robust data on the management of AF are missing and avail-
able evidence is derived mainly from observational studies and/or
extrapolation from large clinical trials.
In patients with AF (or AFL or intra-atrial re-entrant tachycardia)
and congenital heart disease, OAC treatment is recommended for all
patients with intracardiac repair, cyanotic congenital heart disease,
Fontan palliation, or systemic right ventricle.
1273
Patients with AF and
other congenital heart diseases should follow the general risk stratifi-
cation for OAC use in AF. Notably, NOACs are contraindicated in
patients with mechanical heart valves,
1165
whereas they seem safe in
those with a valvular bioprosthesis.
1274,1275
Rate control drugs such as beta-blockers, verapamil, diltiazem, and
digitalis can be used with caution due to the risk of bradycardia and
hypotension. Rhythm control strategies (i.e. amiodarone) may be
effective. In Fontan patients, sodium-channel blockers suppress half
of the atrial arrhythmias, but caution is needed for proarrhythmia.
When cardioversion is planned, both 3 weeks of anticoagulation and
TOE may be considered as thrombi are common in patients with
congenital heart disease and atrial tachyarrhythmias.
1276,1277
In patients with atrial septal defect, closure may be considered
before the fourth decade of life to decrease the risk of AF or AFL.
1278
Patients with stroke who underwent closure of the patent foramen
ovale may have an increased risk of AF,
1279
but in patients with patent
foramen ovale and AF, closure is not recommended for stroke pre-
vention; and OAC use should be decided using the conventional
stroke risk assessment tool. In patients with a history of AF, AF sur-
gery or AF catheter ablation should be considered at the time of
ESC Guidelines 69

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
closure of the septal defect.
12801282
AF catheter ablation of late
atrial arrhythmias is likely to be effective after surgical atrial septal
defect closure.
1283
11.16 Atrial fibrillation in inherited
cardiomyopathies and primary
arrhythmia syndromes
A higher incidence and prevalence of AF have been described in
patients with inherited cardiomyopathies and primary arrhythmia
syndromes.
12841318
Sometimes AF is the presenting or only clini-
cally overt feature,
13191323
is often associated with adverse clinical
outcomes,
1292,1299,1301,1307,1308,1310,13241329
and has important
implications:
•
The use of AADs may be challenging. In congenital long QT syn-
drome, many drugs are contraindicated owing to increased risk
of QT prolongation and torsade de pointes (http://www.credible
meds.org/); in Brugada syndrome, class I drugs are contraindi-
cated (http://www.brugadadrugs.org/). Owing to its long-term
adverse effects, chronic use of amiodarone is problematic in
these typically young individuals.
•
In patients with an implantable cardioverter defibrillator, AF is a
common cause of inappropriate shocks.
1307,1311,13301333
Programming a single high-rate ventricular fibrillation zone
>_210 - 220 bpm with long detection time is safe,
1295,1296,1334
and
is recommended in patients without documented slow mono-
morphic ventricular tachycardia. Implantation of an atrial lead
may be considered in case of significant bradycardia under beta-
blocker treatment.
Supplementary Table 14 summarizes the main clinical features of AF
in patients with inherited cardiac diseases.
Patients with Wolff-Parkinson-White syndrome and AF are at risk
of fast ventricular rates resulting from rapid conduction of atrial elec-
trical activity to the ventricles via the accessory pathway, and at
increased risk of ventricular fibrillation and sudden death.
1335,1336
Electrical cardioversion should be readily available for haemodynami-
cally compromised patients with pre-excited AF, and atrioventricular
node-modulating drugs (e.g. verapamil, beta-blockers, digoxin)
should be avoided.
1337,1338
Pharmacological cardioversion can be
attempted using ibutilide,
1339
whereas class Ic AADs (procainamide,
propafenone, flecainide) should be used with caution owing to their
effect on the atrioventricular node.
13401343
Amiodarone may not
be safe in pre-excited AF as it may enhance pathway conduction.
1343
11.17 Atrial fibrillation during pregnancy
AF is one of the most frequent arrhythmias during pregnancy,
1344
especially in women with congenital heart disease
1345,1346
and in
older gravidae,
1344,1347,1348
and is associated with increased risk of
death.
1344
Rapid atrioventricular conduction may have serious hae-
modynamic consequences for mother and foetus.
Pregnancy is associated with a hypercoagulable state and increased
thrombo-embolic risk. Given the lack of specific data, the same rules
for stroke risk assessment should be used as in non-pregnant
women.
1349
Detailed practical recommendations on oral and paren-
teral anticoagulation regimens depending on the pregnancy trimester,
such as low- and high-dose VKA use during the second and third tri-
mesters, timing of low-molecular-weight heparin (LMWH) to unfrac-
tionated heparin (UFH) relative delivery, and control of therapeutic
effects are given in the recent ESC Pregnancy Guidelines.
1349
Immediate anticoagulation is required in clinically significant mitral
stenosis, using LMWH at therapeutic doses in the first and last tri-
mesters, and VKA with the usual INR targets or LMWH for the sec-
ond trimester. Use of NOACs is prohibited during pregnancy.
Vaginal delivery should be advised for most women but is contraindi-
cated while the mother is on VKAs because of the risk of foetal intra-
cranial bleeding.
1349
Intravenous beta-blockers are recommended for acute rate control.
Beta-1 selective blockers (e.g. metoprolol and bisoprolol) are generally
safe and are recommended as the first choice.
1349
If beta-blockers fail,
digoxin and verapamil should be considered for rate control.
Rhythm control should be considered the preferred strategy dur-
ing pregnancy. Electrical cardioversion is recommended if there is
haemodynamic instability or considerable risk for mother or foetus.
It can be performed safely without compromising foetal blood
flow
1350
and the consequent risk for foetal arrhythmias or preterm
Recommendations for the management of AF in
patients with congenital heart disease
Recommendations Class
a
Level
b
•
Oral anticoagulation should be considered in
all adult patients with intracardiac repair, cya-
nosis, Fontan palliation, or systemic right ven-
tricle and a history of AF, AFL, or intra-atrial
re-entrant tachycardia.
1273
•
In patients with AF and other congenital heart
diseases, anticoagulation should be considered
in the presence of one or more non-sex
stroke risk factor(s).
1273
IIa C
Surgery for AF should be considered in patients:
•
Who need surgical closure of an atrial septal
defect and who have a history of symptomatic
atrial arrhythmia (atrial ablation should be
considered at the time of surgical
closure).
12801282
•
Cox maze surgery should be considered in
patients with symptomatic AF and an indica-
tion for corrective repair of congenital heart
defects. The surgery should be done in experi-
enced centres.
12801282
IIa C
AF catheter ablation of atrial arrhythmias associ-
ated with congenital heart defects may be con-
sidered when performed in experienced
centres.
1283
IIb C
In patients with congenital heart disease, TOE
may be considered together with 3-week antico-
agulation therapy before cardioversion.
1292,1293
IIb C
AF = atrial fibrillation; AFL = atrial flutter; TOE = transoesophageal
echocardiography.
a
Class of recommendation.
b
Level of evidence.
70 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
labour is low.
1351,1352
The fetal heart rate should routinely be con-
trolled after cardioversion.
1353
Cardioversion should generally be
preceded by anticoagulation (section 10.2.2.6).
1349
In haemodynami-
cally stable patients without structural heart disease, i.v. ibutilide or
flecainide may be considered for termination of AF but experience is
limited.
1354,1355
Flecainide, propafenone, or sotalol should be consid-
ered to prevent AF if atrioventricular nodal-blocking drugs fail. AF
catheter ablation has no role during pregnancy.
11.18 Atrial fibrillation in professional
athletes
Moderate physical activity improves cardiovascular health and pre-
vents AF, whereas intense sports activity increases the risk of
AF.
35,1357
Athletes have an approximate five-fold increased lifetime
risk of AF compared with sedentary individuals despite a lower
prevalence of conventional AF risk factors.
35,1020
Risk factors for AF
in athletes include male sex, middle age, endurance sports, tall stat-
ure, and total lifetime exercise dose exceeding
1500 - 2000 hours.
1020,13581361
Endurance sports such as running,
cycling, and cross-country skiing
35,1362
carry the highest risk.
In the absence of RCTs, recommendations for AF management in
athletes are based largely on evidence in non-athletes, observational
data, and expert consensus.
143
The need for anticoagulation is deter-
mined by clinical risk factors. Sports with direct bodily contact or
prone to trauma should be avoided in patients on OAC. As athletes
have a high prevalence of sinus bradycardia and sinus pauses, medical
therapy is frequently contraindicated or poorly tolerated.
1021,1363
Digoxin and verapamil are often ineffective for rate control during
exertional AF, whereas beta-blockers may not be well tolerated or
are sometimes prohibited. Pill-in-the-pocket therapy has been used,
but sports activity should be avoided after ingestion of flecainide or
propafenone until AF ceases and two half-lives of the drug have
elapsed.
586
AF catheter ablation is often preferred by athletes and
was similarly efficacious in both the athletic and non-athletic popula-
tions in small studies.
1364,1365
11.19 Postoperative atrial fibrillation
Perioperative AF describes the onset of the arrhythmia during an
ongoing intervention. This is most relevant in patients undergoing
cardiac surgery. While multiple strategies to reduce the incidence of
perioperative AF with pretreatment or acute drug treatment have
been described, there is lack of evidence from large RCTs.
Amiodarone is the most frequently used drug for prevention of peri-
operative AF.
1369
Postoperative AF, defined as new-onset AF in the immediate post-
operative period, is a clinically relevant problem,
1370,1371
occurring in
20 - 50% of patients after cardiac surgery,
1372,1373
10 - 30% after non-
cardiac thoracic surgery,
1374
and in 5 - 10% after vascular or large col-
orectal surgery,
1375
with peak incidence between postoperative day
2and4.
1376
Intra- and postoperative changes affecting AF triggers
and pre-existing atrial substrate may increase atrial vulnerability to
AF. Many episodes of postoperative AF are self-terminating and
some are asymptomatic, but postoperative AF has been associated
with a four- to five-fold risk of recurrent AF in the next 5
years.
1377,1378
It has also been shown to be a risk factor for stroke,
Recommendations for the management of AF during
pregnancy
Recommendations Class
a
Level
b
Acute management
Immediate electrical cardioversion
c
is recom-
mended in case of haemodynamic instability or
pre-excited AF.
1350,1351,1354
IC
In pregnant women with HCM, cardioversion
c
should be considered for persistent AF.
882
IIa C
Ibutilide or flecainide i.v. may be considered for
termination of AF in stable patients with struc-
turally normal hearts.
1355
IIb C
Long-term management (oral administration of drugs)
Therapeutic anticoagulation with heparin or
VKA according to the stage of pregnancy is rec-
ommended for patients with AF.
1349
IC
Beta-selective blockers are recommended for
rate control in AF.
d
IC
Flecainide,
e
propafenone,
e
or sotalol
f
should be
considered to prevent AF if atrioventricular
nodal-blocking drugs
f
fail.
IIa C
Digoxin
g
or verapamil
g
should be considered for
rate control if beta-blockers fail.
IIa C
AF = atrial fibrillation; ECG = electrocardiogram; US FDA = United States Food
and Drug Administration; i.v. = intravenous; LV = left ventricular; HCM = hyper-
trophic cardiomyopathy; QTc = corrected QT interval; VKA = vitamin K
antagonist.
a
Class of recommendation.
b
Level of evidence.
c
Cardioversion of AF should generally be preceded by anticoagulation.
d
Atenolol has been associated with higher rates of foetal growth retardation and
is not recommended.
1356
e
Flecainide and propafenone should be combined with atrioventricular nodal-
blocking drugs, but structural heart disease, reduced LV function, and bundle
branch block should be excluded.
f
Class III drugs should not be used in prolonged QTc.
g
Atrioventricular nodal-blocking drugs should not be used in patients with pre-
excitation on resting ECG or pre-excited AF.
Note that the former A to X categories of drugs—the classification system for
counselling of pregnant women requiring drug therapy—was replaced by the
Pregnancy and Lactation Labelling Rule, which provides a descriptive risk sum-
mary and detailed information on animal and clinical data, by the US FDA in June
2015.
Recommendations for sports activity in patients with
AF
Recommendation Class
a
Level
b
It is recommended to counsel professional ath-
letes that long-lasting intense sports participation
may promote AF, while moderate physical activ-
ity is recommended to prevent
AF.
35,38,1020,1360,13661368
IB
AF = atrial fibrillation.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 71

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
myocardial infarction, and death compared with non-postoperative
AF patients.
1379,1380
Other adverse consequences of postoperative AF include haemo-
dynamic instability, prolonged hospital stay, infections, renal compli-
cations, bleeding, increased in-hospital death, and greater healthcare
costs.
1371,1381,1382
Management of postoperative AF is shown in
Figure 23.
11.19.1 Prevention of postoperative AF
Preoperative beta-blocker (propranolol, carvedilol plus N-acetyl cys-
teine) use in cardiac and non-cardiac surgery is associated with a
reduced incidence of postoperative AF,
13831386
but not major
adverse events such as death, stroke, or acute kidney injury.
1387
Notably, in non-cardiac surgery, perioperative metoprolol was asso-
ciated with increased risk of death in a large RCT.
1388
In a meta-
analysis, amiodarone (oral or i.v.), and beta-blockers were equally
effective in reducing postoperative AF,
1389
but their combination was
better than beta-blockers alone.
1390
Lower cumulative doses of
amiodarone (<3000 mg) could be effective, with fewer adverse even-
ts.
13911393
Data for other interventions such as statins
974,
,
1394
mag-
nesium,
1395
sotalol,
1385
colchicine,
1396
posterior
pericardiotomy,
1397,1398
(bi)atrial pacing,
1385
and corticosteroids
1399
are not robust. Two large RCTs showed no significant effect of i.v.
steroids on the incidence of postoperative AF after cardiac sur-
gery,
1400,1401
and colchicine is currently being investigated in the
prevention of postoperative AF [COP-AF (Colchicine For The
Prevention Of Perioperative Atrial Fibrillation In Patients Undergoing
Thoracic Surgery): NCT03310125].
11.19.2 Prevention of thrombo-embolic events
In a large meta-analysis, patients with postoperative AF had a 62%
higher odds of early and 37% higher risk of long-term stroke com-
pared with those without postoperative AF (>_1-year stroke rates
were 2.4% vs. 0.4%, respectively), as well as 44% higher odds of early
and 37% higher risk of long-term mortality; long-term stroke risk was
substantially higher with non-cardiac than cardiac postoperative AF
(HR 2.00; 95% CI 1.702.35 for non-cardiac vs. HR 1.20; 95% CI
1.071.34 for cardiac postoperative AF; P for subgroup difference
<0.0001).
1379
Nevertheless, the evidence on OAC effects in patients with post-
operative AF is not very robust.
1382,14021407
Observational data
1408
suggest that although coronary artery bypass graft-related postopera-
tive AF might not be equivalent to non-surgery AF regarding the
long-term risk of adverse outcomes, OAC use during follow-up was
associated with a significantly lower risk of thrombo-embolic events
in both postoperative AF and non-surgery AF compared with no
OAC.
1408
Reportedly, postoperative AF occurring after non-cardiac
surgery was associated with a similar long-term thrombo-embolic
risk to non-surgery AF, and OAC therapy was associated with com-
parably lower risk of thrombo-embolic events and all-cause death in
©ESC 2020
Figure 23 Management of postoperative AF. AAD = antiarrhythmic drug; bpm = beats per minute; CCB = calcium channel blocker; ECV = electrical
cardioversion; LVEF = left ventricular ejection fraction; Mg
2þ
magnesium; OAC = oral anticoagulation; PCV = pharmacological cardioversion;
PUFA=polyunsaturated fatty acid.
72 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
both groups.
1409
Ongoing RCTs in cardiac [PACES (Anticoagulation
for New-Onset Post-Operative Atrial Fibrillation After CABG);
NCT04045665] and non-cardiac (ASPIRE-AF; NCT03968393) sur-
gery will inform optimal long-term OAC use among patients devel-
oping postoperative AF.
In haemodynamically unstable patients with postoperative AF,
emergency electrical cardioversion (or i.v. administration of amiodar-
one
1385
or vernakalant,
583
if consistent with the clinical situation) is
indicated. In a recent RCT of postoperative AF patients after cardiac
surgery, neither rate nor rhythm control showed net clinical advant-
age over each other.
1373
Hence, rate or rhythm control treatment
decisions should be based on symptoms, and non-emergency cardio-
version should follow the principles of peri-cardioversion anticoagu-
lation outlined in section 10.2.
12 Prevention of atrial fibrillation
12.1 Primary prevention of atrial
fibrillation
Primary prevention of AF refers to the implementation of preventive
measures in patients at risk but without previous documentation of
AF. This strategy relies on the identification and management of risk
factors and comorbidities predisposing to AF, before the develop-
ment of atrial remodelling and fibrosis
964,
.
1411
Upstream therapy
refers to the use of non-AADs that modify the atrial substrate or
target-specific mechanisms of AF to prevent the occurrence or
recurrence of the arrhythmia. The key targets of upstream therapy
are structural changes in the atria (e.g. fibrosis, hypertrophy, inflam-
mation, oxidative stress), but effects on atrial ion channels, gap junc-
tions, and calcium handling are also evident.
964
Adequate management of hypertension and HF may prevent AF
by reducing atrial stretch, but inhibition of the renin-angiotensin-
aldosterone system may exert an additional protective role by sup-
pressing electrical and structural cardiac remodelling.
964,1411,1412
Large RCTs and meta-analyses have yielded equivocal results, either
in favour
14131416
or against
14171421
statin use for primary preven-
tion of AF. Controversial results have also been reported for the
effects of fish oils on primary prevention of AF.
1422
For primary prevention of postoperative AF after cardiac and non-
cardiac surgery, see section 11.19.
12.2 Secondary prevention of atrial
fibrillation
For secondary AF prevention see section 11.3 and Supplementary sec-
tion 12.
13 Sex-related differences in atrial
fibrillation
Female patients are generally under-represented in RCTs, including
AF trials. Sex-related differences in the epidemiology, pathophysiol-
ogy, clinical presentation, and prognosis of AF that are consistently
reported
19,107,124,1423,1424
may influence the effectiveness of AF treat-
ment, and hence should be considered in a personalized, individual
patient-centred approach to AF management in clinical practice.
1425
Understanding the underlying pathophysiological mechanisms and
biology may help to improve personalized treatments. Adequate rep-
resentation of women in future AF trials is recommended, as well as
the identification and resolution of sex-specific barriers to implemen-
tation of guideline-recommended treatments for AF.
Women presenting with AF are older, have a higher prevalence of
hypertension, VHD, and HFpEF, and a lower prevalence of CAD
compared with men. Women with AF are more often symptomatic
than men with AF, with greater symptom severity.
1423,1426
Female sex is a stroke risk modifier that increases the risk of AF-
associated stroke in the presence of other stroke risk factors.
353
Women with AF have a greater stroke severity and permanent dis-
ability than men with AF.
1427
Anticoagulation with warfarin may be
less well controlled in women, and they have a greater residual stroke
risk even with well-controlled VKAs.
1428
The efficacy and safety of
NOACs in landmark RCTs were consistent in both sexes, but
women were largely under-represented.
423
In women with AF, the use of AADs for rhythm control is associ-
ated with significantly higher rates of life-threatening adverse events
(e.g. acquired long QT syndrome with class Ia or III AADs)
1429,1430
or
sinus-node disease/bradyarrhythmia requiring pacemaker implanta-
tion
19
compared with male patients. Women with AF are less likely
to undergo electrical cardioversion,
1426
and are referred for AF cath-
eter ablation later than men, possibly reflecting AF occurrence later
in life among women.
107,1431,1432
The result of PVI may be less favour-
able in women,
1431,1432
with higher rates of procedure-related com-
plications.
1431
Women are more likely to undergo atrioventricular
nodal ablation for AF than men.
124
Sex-specific data on cardiovascu-
lar risk management in women with AF are lacking. Principles out-
lined in section 11.3 apply to women with AF.
Recommendations for postoperative AF
Recommendations Class
a
Level
b
Perioperative amiodarone or beta blocker ther-
apy is recommended for the prevention of post-
operative AF after cardiac surgery.
1390,1492
IA
Long-term OAC therapy to prevent thrombo-
embolic events should be considered in patients
at risk for stroke with postoperative AF after
non-cardiac surgery, considering the anticipated
net clinical benefit of OAC therapy and informed
patient preferences.
1404,1405,1408,1409
IIa B
Long-term OAC therapy to prevent thrombo-
embolic events may be considered in patients at
risk for stroke with postoperative AF after car-
diac surgery, considering the anticipated net clin-
ical benefit of OAC therapy and informed
patient preferences.
1404,1405,1408,1409
IIb B
Beta-blockers should not be used routinely for
the prevention of postoperative AF in patients
undergoing non-cardiac surgery.
1410
III B
AF = atrial fibrillation; OAC = oral anticoagulant.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 73

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
14 Implementation of the atrial
fibrillation guidelines
Guideline-adherent care (i.e. the implementation of guideline-
recommended management to individual AF patients) aims to
improve patient outcomes and reduce healthcare costs,
1238,1434,1435
but adherence to guidelines is modest
worldwide.
124,14361439,1440,1441
Reportedly, the adoption of
NOACs as first-line therapy has been associated with increasing
guideline-adherent stroke prevention.
1442,1443
Guideline non-adherence is multifactorial,
1215,1444,1445
including
physician/healthcare professional- and healthcare system-related fac-
tors.
1446
Integrated AF management may facilitate adherence to
guidelines. Various educational interventions
280,284,290,1447,1448
based
on guideline-provided recommendations
284
and tailored to close
specific knowledge gaps among healthcare professionals and/or AF
patients
1446
may facilitate the implementation of guideline-based AF
management to improve patient outcomes.
277,14491452
Further
research is needed to identify the cost-effective intervention type(s)
that would more effectively improve patient clinical outcomes, medi-
cation adherence, and QoL.
15 Quality measures and clinical
performance indicators in the
management of atrial fibrillation
Measurable service quality has been identified as a cornerstone for
optimal AF management and is a mandatory step towards value-
based healthcare. Quality and performance indicator sets should pro-
vide practitioners and institutions with the tools to measure the qual-
ity of care (e.g. adherence to guideline class I recommendations upon
discharge/end of visit, complications after procedures, access/waiting
list times) and identify opportunities for improvement. They should
capture important aspects of care quality, including structure, proc-
ess, outcome measures, and patient-centrednes, while the reporting
burden for hospitals, practices, and practitioners should be kept to a
minimum.
658,14531455
A collaborative effort involving the ESC, EHRA, Asia Pacific Heart
Rhythm Society, Heart Rhythm Society, and Latin American Heart
Rhythm Society was put in place to develop quality indicators for the
diagnosis and management of AF; a summary form of these quality
indicators is provided in Table 22, with the full set published sepa-
rately.
317
The ESC quality indicators are intended for quality
improvement and performance measurement through meaningful
surveillance, as well as for integration within registries that specifically
aim to identify areas for improvement in clinical practice and are not
intended for ranking healthcare professionals/providers or payment
incentives.
16 Epidemiology, clinical
implications, and management of
atrial high-rate episodes/
subclinical atrial fibrillation
The incidence of AHRE/subclinical AF in patients with a pacemaker/
implanted device is 3070%, but it may be lower in the general pop-
ulation.
1458
Very short episodes (<_10 - 20 s/day) are considered clini-
cally irrelevant, as they are not significantly associated with longer
episodes or an increased risk of stroke or systemic embolism.
1459
However, longer episodes of AHRE/subclinical AF (minimum of 5 - 6
min) are associated with an increased risk of clinical AF,
467,469
ischae-
mic stroke,
168,467
major adverse cardiovascular events,
1460
and cardi-
ovascular death.
1461
Overall, the absolute risk of stroke associated with AHRE/subclini-
cal AF may be lower than with clinical AF.
160,168,226,467
The temporal
dissociation from acute stroke suggests that AHRE/subclinical AF
may represent a marker rather than a risk factor for stroke
4,7,1462
(Supplementary Box 6).
Whereas current data were obtained mostly from pacemakers/
implantable cardioverter defibrillators or post-stroke patients,
AHRE/subclinical AF is increasingly reported in a variety of patients
undergoing cardiac monitoring. Clinical AF will reportedly develop in
1 in 5 - 6 of patients within 2.5 years after diagnosing AHRE/subclini-
cal AF.
168
Notwithstanding that more high-quality evidence is needed
to inform optimal management of these patients, more intense
Recommendations pertaining to sex-related differences
in AF
Recommendation Class
a
Level
b
It is recommended that women and men with
AF are equally offered diagnostic assessment and
therapies to prevent stroke and other AF-
related complications.
423,1433
IA
Women with symptomatic paroxysmal or per-
sistent AF should be offered timely access to
rhythm control therapies, including AF catheter
ablation, when appropriate for medical
reasons.
1448,1451
IIa B
AF = atrial fibrillation.
a
Class of recommendation.
b
Level of evidence.
Recommendations for quality measures in patients with
AF
Recommendations Class
a
Level
b
The introduction of tools to measure quality of
care and identify opportunities for improved
treatment quality and AF patient outcome
should be considered by practitioners and
institutions.
317
IIa B
AF = atrial fibrillation.
a
Class of recommendation.
b
Level of evidence.
74 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
follow-up and monitoring to detect clinical AF early is prudent (pref-
erably with the support of remote monitoring). Notably, the AHRE/
subclinical AF burden is not static but may change on daily basis,
469
hence should be regularly reassessed—the greater the AHRE/sub-
clinical AF burden at diagnosis, the higher the risk of subsequent pro-
gression to longer episodes
469
(Figure 24).
Whereas available evidence is insufficient to justify routine OAC
use in patients with AHRE/subclinical AF, modifiable stroke risk fac-
tors should be identified and managed in each patient.
The use of OAC may be considered in selected patients with lon-
ger durations of AHRE/subclinical AF (>_24 h) and an estimated high
individual risk of stroke,
4,1462
accounting for the anticipated net
Table 22 Summary of quality indicators for the diagnosis and management of AF
Domain: Patient assessment (at baseline and follow-up)
Main quality indicator: CHA
2
DS
2
-VASc cardioembolic risk assessment.
Main quality indicator: bleeding risk assessment using a validated method such as the HAS-BLED score.
Numerator: Number of AF patients who have their respective score documented at the time of diagnosis and at every follow-up appointment.
Denominator: Number of AF patients.
Domain: Anticoagulation
Main quality indicator: inappropriate prescription of anticoagulation to patients with a CHA
2
DS
2
-VASc score of 0 for men and 1 for women.
Numerator: number of AF patients with CHA
2
DS
2
-VASc score of 0 for men and 1 for women, who are inappropriately prescribed anticoagulation.
Denominator: number of AF patients with CHA
2
DS
2
-VASc score of 0 for men and 1 for women who do not have other indication for anticoagulation.
Main quality indicator: proportion of patients with a CHA
2
DS
2
-VASc score of >_1 for men and >_2 for women who are prescribed anticoagulation.
Numerator: Number of AF patients with CHA
2
DS
2
-VASc score of >_1 for men and >_2 for women who are prescribed anticoagulation.
Denominator: Number of AF patients with CHA
2
DS
2
-VASc score of >_1 for men and >_2 for women who are eligible for anticoagulation with no contraindica-
tion or refusal.
Domain: rate control
Main quality indicator: inappropriate prescription of AADs
a
to patients with permanent AF (i.e. where no attempt to restore sinus rhythm is planned).
Numerator: Number of patients with permanent AF who are prescribed one or more AADs
a
for rhythm control.
Denominator: Number of patients with permanent AF.
Domain: rhythm control
Main quality indicator: inappropriate prescription of class IC AADs to patients with structural heart disease.
Numerator: number of AF patients with structural heart disease who are inappropriately prescribed class IC AADs.
Denominator: number of AF patients with structural heart disease.
Main quality indicator: proportion of patients with symptomatic paroxysmal or persistent AF who are offered AF catheter ablation after failure of/intolerance
to one class I or class III AAD.
Numerator: Number of patients with paroxysmal or persistent AF who are offered catheter ablation after the failure of, or intolerance to, at least one class I
or class III AAD.
Denominator: Number of patients with paroxysmal or persistent AF with no contraindications (or refusal) to catheter ablation who remain symptomatic on,
or intolerant to at least one class I or class III AAD.
Domain: risk factor management
Main quality indicator: Proportion of patients who have their modifiable risk factors identified.
Numerator: number of AF patients who have their modifiable risk factors (e.g. BP, obesity, OSA, alcohol excess, lack of exercise, poor glycaemic control and
smoking) identified
Denominator: number of AF patients.
Domain: outcomes
Main quality indicator: ischaemic stroke or TIA.
Main quality indicator: life-threatening or major bleeding events.
b
Numerator: number of AF patients who have a documented ischaemic or bleeding event
Denominator: number of AF patients or number of patients prescribed an OAC, respectively.
AAD = antiarrhythmic drug; AF = atrial fibrillation; BP = blood pressure; CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke,
Vascular disease, Age 65-74 years, Sex category (female); HAS-BLED = Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile INR,
Elderly (>65 years), Drugs/alcohol concomitantly; OAC = oral anticoagulant; OSA = obstructive sleep apnoea; TIA = transient ischaemic attack.
a
Flecainide, propafenone, amiodarone, dronedarone, sotalol and disopyramide.
b
Using the definitions of the International Society of Thrombosis and Haemostasis.
1456,1457
ESC Guidelines 75

.
.
.
.
.
.
.
.
.
.
.
.
clinical benefit and informed patient’s preferences (Figures 24 and 25).
In the recent trials, OAC was initiated in 76.4% and 56.3% of patients
with >_2 clinical stroke risk factors and insertable cardiac monitor-
detected physician-confirmed AF>_6 min, but follow-up bleeding
rates were not reported.
1463,1464
In a large retrospective cohort
study using remote monitoring data about daily AF burden, there was
large practice variation in OAC initiation. Across increasing AF bur-
den strata (from >6 min to >24 h) the risk of stroke in untreated
©ESC 2020
Figure 25 Proposed management of AHRE/subclinical AF. AF = atrial fibrillation; AHRE = atrial high-rate episode; CKD = chronic kidney disease;
CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 65 - 74 years, Sex category
(female); f = female; LA = left atrium; LoE = level of evidence; m = male; OAC = oral anticoagulant; SCAF = subclinical atrial fibrillation.
a
Highly selected
patients (e.g. with previous stroke and/or age >_75 years, or >_3 CHA
2
DS
2
-VASc risk factors, and additional non-CHA
2
DS
2
-VASc stroke factors such as
CKD, elevated blood biomarkers, spontaneous echo contrast in dilated LA, etc); selected patients (e.g. with previous stroke and/or age >_75 years, or >_3
CHA
2
DS
2
-VASc risk factors , etc).
©ESC 2020
Figure 24 Progression of atrial high-rate episode burden (left panel) and stroke rates according to AHRE daily burden and CHA
2
DS
2
-VASc score (right
panel). AHRE = atrial high-rate episodes; CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular dis-
ease, Age 65 - 74 years, Sex category (female); OAC = oral anticoagulant.
a
The higher the burden at diagnosis, the greater the incidence of progression in
the next 6 months and thereafter.
b
Stroke rates above the threshold for OAC are shown in red.
76 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
patients increased numerically, and the strongest association of OAC
with reduction in stroke was observed among patients with device-
detected AF episodes of >24 h.
5
17 Atrial fibrillation and other
atrial tachyarrhythmias (atrial
flutter and atrial tachycardias)
Although AFL may exist as a solitary atrial arrhythmia, a significant
proportion of patients will subsequently develop AF.
14661470
Typical AFL may occur in those taking class IC AADs or amiodar-
one.
1467,1468,1471
The ABC pathway for integrated AF management
largely applies to patients with AFL. It is recommended that stroke-
prevention strategies in patients with solitary AFL, including peripro-
cedural management of stroke risk, follow the same principles as in
patients with AF.
1472
Rate control should be the first step in symptom management.
However, cardioversion to sinus rhythm may be more effective,
especially electrical cardioversion or (where feasible) high-rate stimu-
lation.
1473,1474
Of note, the class III AADs dofetilide and ibutilide i.v.
are very effective in interrupting AFL, whereas the class Ic drugs fle-
cainide and propafenone
14751478
should not be used in the absence
of atrioventricular-blocking drugs as they may slow the atrial rate,
thus facilitating 1 : 1 atrioventricular conduction with a rapid ventricu-
lar rate.
1479,1480
AF catheter ablation of the CTI is the most effective
rhythm control treatment for CTI-dependent AFL.
732,1481,1482
When
typical AFL develops in AF patients during treatment with class Ic
drugs or amiodarone, CTI ablation should be considered to ensure
that AADs can be continued for AF rhythm control.
732,1481
Atypical AFL (i.e. macro re-entrant atrial tachycardia) most com-
monly occurs in diseased or scarred atrial myocardium. Clinical
management of atypical AFL/macro re-entrant atrial tachycardia
broadly follows the principles of typical AFL management, but the
use of AADs is often limited by significant structural heart disease,
and ablation is more complex.
1336
Notably, the intervention to treat atrial tachycardias (AFL/macro
re-entrant atrial tachycardia) occurring early after AF catheter abla-
tion (or surgery) should be delayed, and initial rate control or the use
of AADs should be considered instead, as some of these tachyar-
rhythmias are transient and cease after maturation of the lesions
deployed by the index procedure.
14831485
For additional details
about AFL, see Supplementary Box 7 and the 2019 ESC Guidelines on
supraventricular tachycardias.
1336
18 Key messages
(1) The diagnosis of AF needs to be confirmed by a conventional 12-
lead ECG tracing or rhythm strip showing AF for >_30 s.
(2) Structured characterization of AF, including stroke risk, symptom
severity, severity of AF burden, and AF substrate, helps improve
personalized treatment of AF patients.
(3) Novel tools and technologies for screening and detection of AF
such as (micro-)implants and wearables substantially add to the
diagnostic opportunities in patients at risk for AF. However,
appropriate management pathways based on such tools are still
incompletely defined.
(4) Integrated holistic management of AF patients is essential to
improving their outcomes.
(5) Patient values need to be considered in treatment decision making
and incorporated into the AF management pathways; the struc-
tured assessment of PRO measures is an important element to
document and measure treatment success.
(6) The ABC pathway streamlines integrated care of AF patients
across healthcare levels and among different specialties.
(7) Structured, clinical, risk-score-based assessment of individual
thrombo-embolic risk, using the CHA
2
DS
2
-VASc score, should be
performed as the first step in optimal thrombo-embolic risk man-
agement in AF patients.
(8) Patients with AF and risk factors for stroke need to be treated
with OAC for stroke prevention. In NOAC-eligible patients,
NOACs are preferred over VKAs.
(9) A formal structured risk-score-based bleeding risk assessment using,
for example, the HAS-BLED score, helps to identify non-modifiable
and address modifiable bleeding risk factors in AF patients.
(10) An elevated bleeding risk should not automatically lead to withhold-
ing OAC in patients with AF and stroke risk. Instead, modifiable
bleeding risk factors should be addressed, and high-risk patients
scheduled for a more frequent clinical review and follow-up.
(11) Rate control is an integral part of AF management and is often suf-
ficient to improve AF-related symptoms.
(12) The primary indication for rhythm control using cardioversion,
AADs, and/or catheter ablation is reduction in AF-related symp-
toms and improvement of QoL.
(13) The decision to initiate long-term AAD therapy needs to balance
symptom burden, possible adverse drug reactions, particularly
drug-induced proarrhythmia or extracardiac side-effects, and
patient preferences.
Recommendations for management of patients with
AHRE
Recommendations Class
a
Level
b
In patients with AHRE/subclinical AF detected by
CIED or insertable cardiac monitor, it is recom-
mended to conduct:
•
Complete cardiovascular evaluation with ECG
recording, clinical risk factors/comorbidity
evaluation, and thrombo-embolic risk assess-
ment using the CHA
2
DS
2
-VASc score.
469
•
Continued patient follow-up and monitoring
(preferably with the support of remote moni-
toring) to detect progression to clinical AF,
monitor the AHRE/subclinical AF burden
(especially transition to >_24 h), and detect
changes in underlying clinical conditions.
469
IB
AF = atrial fibrillation; AHRE = atrial high-rate episode; CIED = cardiac implant-
able electronic device; ECG = electrocardiogram.
a
Class of recommendation.
b
Level of evidence.
ESC Guidelines 77

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
(14) Catheter ablation is a well-established treatment for prevention of
AF recurrences. When performed by appropriately trained opera-
tors, catheter ablation is a safe and superior alternative to AADs
for maintenance of sinus rhythm and symptom improvement.
(15) Major risk factors for AF recurrence should be assessed and con-
sidered in the decision making for interventional therapy.
(16) In patients with AF and normal LVEF, catheter ablation has not
been shown to reduce total mortality or stroke. In patients with
AF and tachycardia-induced cardiomyopathy, catheter ablation
reverses LV dysfunction in most cases.
(17) Weight loss, strict control of risk factors, and avoidance of triggers for
AF are important strategies to improve outcome of rhythm control.
(18) Identification and management of risk factors and concomitant dis-
eases is an integral part of the treatment of AF patients.
(19) In AF patients with ACS undergoing uncomplicated PCI, an early
discontinuation of aspirin and switch to dual antithrombotic ther-
apy with OAC and a P2Y
12
inhibitor should be considered.
(20) Patients with AHRE should be regularly monitored for progression
to clinical AF and changes in the individual thrombo-embolic risk
(i.e. change in CHA
2
DS
2
-VASc score). In patients with longer
AHRE (especially >24 h) and a high CHA
2
DS
2
-VASc score, it is
reasonable to consider the use of OAC when a positive net clinical
benefit from OAC is anticipated in a shared, informed, treatment
decision-making process.
19 Gaps in evidence
Whereas some progress has been made since publication of the 2016
ESC AF Guidelines, major gaps identified in those guidelines persist in
2020, calling for more intense research. In 2019, the EHRA published a
white paper that covers major gaps in the field of AF in detail.
1486
The
following bullet-list gives the most important knowledge gaps:
h Major health modifiers causing atrial fibrillation
Mechanisms of AF are not yet fully understood. Improvement in
understanding of these mechanisms in individual patients, e.g. patients
with cardiac structural remodelling or HF, would allow better selec-
tion of treatments including the best rate and rhythm control strat-
egies and OAC.
It is uncertain how educational interventions translate into actual
behavioural change (patients and physicians) that leads to improve-
ments in clinical management and outcomes, especially in the multi-
morbid AF patient.
h Implementation of digital technologies for screening,
diagnosis, and risk stratification in the atrial fibrillation
patient
New techniques for digital ECG analysis (e.g. machine learning and
artificial intelligence) and new technologies (e.g. wearables and inject-
ables) have opened up potentially significant opportunities for the
detection and diagnosis of AF. These innovations may help to person-
alize therapy and risk stratification. Studies are needed to evaluate
such opportunities and to define for which groups of patients this is
worthwhile.
h Type of atrial fibrillation
There is a gap in knowledge regarding classification of AF. Recent
data suggest that paroxysmal AF is not one entity. According to the
pattern, type of therapy and outcome may differ.
1487
More studies
are needed.
h How much atrial fibrillation constitutes a mandate for
therapy?
The threshold of AF burden at which to initiate OAC therapy needs
to be defined more clearly. This knowledge gap has resulted in sub-
stantial variation in physician attitudes and practice patterns.
5
We are still waiting for the results of two ongoing RCTs in subclinical
AF patients who are detected with cardiac implantable electronic device
(CIED) [(Apixaban for the Reduction of Thrombo-Embolism in Patients
With Device-Detected Sub-Clinical Atrial Fibrillation) (NCT
01938248) and NOAH (Non-vitamin K Antagonist Oral Anticoagulants
in Patients With Atrial High Rate Episodes) (NCT 02618577)].
h Role of biomarkers in atrial fibrillation management
Although some studies have demonstrated an effective role of bio-
markers (including natriuretic peptides and troponin) in AF risk
assessment, there is uncertainty over the exact time point of bio-
marker assessment, optimal cut-offs, and the effect on management
decision making based on changes in biomarker levels over time,
especially with increasing age and incident comorbidities.
h Stroke risk in specific populations
Some studies have tested the effect of biomarkers in predicting risk
of AF-related complications, including stroke, in specific populations.
However, it is unknown if biomarkers and biomarker-based scores
practically help physicians in refining stroke risk, especially in prospec-
tive non-anticoagulated cohorts, particularly given the dynamic
nature of stroke risk and how many current biomarkers are non-
specific for AF or AF-related outcomes.
There is uncertainty of actual stroke risk in AHRE, compared with
actual stroke risk in overt AF, in properly matched cohorts in similar
settings, and the effect of appropriate management pathways.
The effect of sex in AF patients has been more investigated. Men
with AF are less likely to have hypertension or VHD vs. women.
1488
Women often present with atypical symptoms related to AF. Further
comparative studies are needed in different settings and ethnic
groups on the effect of different stroke risk factors and female sex on
stroke and bleeding risks.
h Anticoagulant therapy in specific patients
There is a gap in knowledge regarding optimal NOAC dosing in spe-
cific groups, including those with mild-to-moderate CKD, with very
low/high body mass index, and patients receiving medications with a
high risk of metabolic interaction.
1489
In patients with CrCl <_25 mL/min, RCT-derived data on the effect of
VKA or NOACs is still lacking, due to the exclusion of these patients
from the major RCTs. However, two RCTs (NCT02933697,
NCT03987711) are currently assessing OAC use and comparing
NOACs with VKAs in patients with end-stage renal disease.
h Anticoagulation in patients with heart valve diseases
There are gaps in evidence on NOAC use in AF patients with rheu-
matic mitral valve disease and during the first 3 months after surgical
or transcatheter implantation of a bioprosthesis; observational data
regarding the use of NOACs after transcatheter aortic valve implan-
tation are conflicting.
1163
h Anticoagulation in atrial fibrillation patients after a
bleeding or stroke event
As high-quality RCT-derived evidence to inform optimal timing of
anticoagulation after acute ischaemic stroke is lacking, OAC use in
the early post-stroke period is currently based on expert consensus.
Several ongoing RCTs [ELAN (NCT03148457), OPTIMAS
78 ESC Guidelines

©ESC 2020
1.
I
dent
i
f
y l
f
f
o
w
-risk
p
atient
s
CH
A
2
D
S
2
-
V
-
A
V
V
S
c
0
(
m
)
,
1
(
f
)
C
H
A
2
D
S
2
V
A
V
V
Sc ≥
1
(
m
)
, 2
(
f
)
A
s
sess bleedin
g
ri
s
k
,
ad
d
r
ess
3.
C
h
oose
OA
C
(N
O
A
C
o
r VK
A
w
i
t
h
w
e
ll-mana
g
ed
T
T
R
)
RR
Assess s
y
m
p
to
m
s
,
Q
oL
a
n
d
p
atie
n
t
’
s
p
r
e
f
e
f
f
r
ences
Op
tim
i
z
e ra
t
e
con
t
r
ol
Co
n
s
id
e
r
a
r
h
y
t
hm
con
t
r
ol
s
t
rate
g
y
Comorbidities
a
nd
ca
r
d
i
o
v
a
s
cu
l
a
r
ris
k
f
a
ff
c
to
r
s
Li
f
e
f
f
s
t
y
l
e
c
h
a
nges
(
ob
es
i
(
(
t
y
r
e
d
u
c
t
i
o
n
,
r
egu
l
a
r
e
x
e
r
c
is
e
,
r
edu
c
t
i
o
n
of
a
lcohol
us
e
,
et
c
.
)
Treat AF: The ABC pathway
A
Anticoagulation/
Avoid stroke
B
Better
symptom
control
C
Comorbidities/
Cardiovascular
risk factor
management
Symptom severity (Sy)
(e.g., EHRA symptom score)
Severity of AF burden (Sb)
(duration, spontaneous termination)
Stroke risk (St)
(e.g., CHA
2
DS
2
-VASc score)
Substrate severity (Su)
(age, comorbidities,
C
CC To ABC
Characterise AF (the 4S-AF scheme)
A 12-lead ECG or a rhythm strip showing AF pattern for ≥30 s
(CV, AADs, ablation)
Central Illustration Management of AF. AAD = antiarrhythmic drug; AF = atrial fibrillation; ECG = electrocardiogram; EHRA = European Heart
Rhythm Association; CHA
2
DS
2
-VASc = Congestive HF, Hypertension, Age >_75 years, diabetes mellitus, Stroke, Vascular disease, Age 65 - 74 years, Sex
category (female); CV = cardioversion; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagulant; TTR = time in therapeutic range;
VKA = vitamin K antagonist.
ESC Guidelines 79

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
(EudraCT, 2018-003859-3), TIMING (NCT02961348), and START
(NCT03021928)] will try to assess the differences between the two
approaches, including early (<1 week) vs. late NOAC initiation in
patients with AF-related ischaemic stroke.
h Left atrial appendage occlusion for stroke prevention
More studies have been conducted in this field. There is clearer evidence
of the safety and possible complications of the LAA closure
procedure.
450454
However, there are still knowledge gaps to be
addressed: (i) antithrombotic management after LAA occlusion has not
been evaluated in a randomized manner; and (ii) the efficacy and safety of
LAA closure vs. OAC therapy needs to be assessed in randomized trials.
LAA occluders have not been compared with NOAC therapy in
patients at risk for bleeding, or with surgical LAA occlusion/
exclusion.
h Surgical exclusion of Left atrial appendage
Only limited RCT data are available
457459
on surgical exclusion of
theLAA.AlthoughalargeRCTinpatientswithanassociatedcardiac
surgical procedure is ongoing,
462
adequately powered RCTs are
needed.
There is the need for adequately powered trials to define the best
indications for LAA occlusion/exclusion compared with NOAC ther-
apy in patients with relative or absolute contraindications for anticoa-
gulation, in those with an ischaemic stroke on anticoagulant therapy,
and for assessment of the appropriate antithrombotic therapy after
LAA occlusion.
h Atrial fibrillation catheter ablation technique
The best approach to safely and expeditiously achieve permanent
PVI in a single procedure is still one of the knowledge gaps in relation
to emerging technologies for catheter ablation of AF. Moreover, it
remains unknown if ablating additional targets will improve the out-
comes of AF catheter ablation.
1490
h Outcome of atrial fibrillation catheter ablation
The following issues need to be addressed in further studies:
•
The value of early AF ablation to prevent AF progression.
•
The optimal outcome measure (AF 30 s, AF burden, etc.) for AF-
related outcome.
•
How much reduction in AF burden is needed to achieve an effect
on hard endpoints, including survival, stroke, and comorbidity.
•
The main mechanism of PVI translating into freedom of AF.
•
The potential effect of cardiac structure and function on the like-
lihood of success of AF ablation.
Despite the publication of CABANA and CASTLE-AF, more data
are needed on the effect of AF catheter ablation on clinical outcomes,
including death, stroke, serious bleeding, AF recurrence, QoL, and
cardiac arrest.
The relationship between the degree of atrial dilation/fibrosis and
successful ablation of AF needs to be addressed. Additionally, the
impact of specific components of structural heart disease, including
LA structure/function, LV structure, etc., on the success of AF cathe-
ter ablation and the likelihood of recurrence requires further
investigation.
h Who may benefit less from atrial fibrillation catheter
ablation
There are gaps in knowledge about subgroups of patients who may
benefit less from AF catheter ablation, including (i) persistent and
long-standing persistent AF; (ii) patients with enlarged atrial size and/
or atrial fibrosis; (iii) patients with atypical AFL; and (iv) patients with
risk factors for AF recurrence, including obesity or sleep apnoea.
h Thoracoscopic ‘stand-alone’ atrial fibrillation surgery
There are no convincing data on the effects on stroke of surgical abla-
tion as a stand-alone procedure or in combination with LAA occlu-
sion or exclusion on various outcomes including QoL, stroke, and
death.
h Personalized therapy
The arrhythmia phenotype may differ among patients. Improved
assessment of the pathophysiological process involved in the individ-
ual patient by using clinical characteristics, blood biomarkers, and
non-invasive substrate determination (echo/MRI/CT) may improve
personalized therapy (e.g. selection of rhythm control, yes or no;
treatment of risk factors and comorbidities; type of antiarrhythmic
drug; atrial ablation; and which type/techniques used for AF).
Recommendations Class
a
Level
b
Recommendations for diagnosis of AF
ECG documentation is required to establish the diagnosis of AF.
•
A standard 12-lead ECG recording or a single-lead ECG tracing of >_30 s showing heart rhythm with no discernible repeating P
waves and irregular RR intervals (when atrioventricular conduction is not impaired) is diagnostic of clinical AF.
IB
Recommendations for screening of AF
Opportunistic screening for AF by pulse taking or ECG rhythm strip is recommended in patients >_65 years of age.
IB
It is recommended to interrogate pacemakers and implantable cardioverter defibrillators on a regular basis for AHRE.
IB
When screening for AF it is recommended that:
•
The individuals undergoing screening are informed about the significance and treatment implications of detecting AF.
•
A structured referral platform is organized for screen-positive cases for further physician-led clinical evaluation to confirm the
diagnosis of AF and provide optimal management of patients with confirmed AF.
•
Definite diagnosis of AF in screen-positive cases is established only after the physician reviews the single-lead ECG recording of
>_30 s or 12-lead ECG and confirms that it shows AF.
IB
Continued
20 ‘What to do’ and ‘what not to do’ messages from the Guidelines
80 ESC Guidelines

Recommendations for diagnostic evaluation of patients with AF
In patients with AF, it is recommended to:
•
Evaluate AF-related symptoms (including fatigue, tiredness, exertional shortness of breath, palpitations, and chest pain) and
quantify the patient symptom status using the modified EHRA symptom scale before and after initiation of treatment.
•
Evaluate AF-related symptoms before and after cardioversion of persistent AF to aid rhythm control treatment decisions.
IC
In patients with AHRE/subclinical AF detected by CIED or insertable cardiac monitor, it is recommended to conduct:
•
Complete cardiovascular evaluation with ECG recording, clinical risk factors/comorbidity evaluation, and thrombo-embolic risk
assessment using the CHA
2
DS
2
-VASc score.
•
Continued patient follow-up and monitoring (preferably with the support of remote monitoring) to detect progression to clini-
cal AF, monitor the AHRE/subclinical AF burden (especially transition to >_24 h), and detect changes in underlying clinical
conditions.
IB
Recommendations about integrated AF management
To optimize shared decision making about specific AF treatment option(s) in consideration, it is recommended that physicians:
•
Inform the patient about the advantages/limitations and benefit/risks associated with the treatment option(s) being considered;
and
•
Discuss the potential burden of the treatment with the patient and include the patient’s perception of treatment burden in the
treatment decision.
IC
It is recommended to routinely collect PROs to measure treatment success and improve patient care.
IC
Recommendations for the prevention of thrombo-embolic events in AF
For stroke prevention in AF patients who are eligible for OAC, NOACs are recommended in preference to VKAs (excluding
patients with mechanical heart valves or moderate-to-severe mitral stenosis).
IA
For stroke risk assessment, a risk-factor-based approach is recommended, using the CHA
2
DS
2
-VASc clinical stroke risk score to
initially identify patients at ‘low stroke risk’ (CHA
2
DS
2
-VASc score = 0 in men, or 1 in women) who should not be offered antith-
rombotic therapy.
IA
OAC is recommended for stroke prevention in AF patients with CHA
2
DS
2
-VASc score >_2 in men or >_3 in women.
IA
For bleeding risk assessment, a formal structured risk-score-based bleeding risk assessment is recommended to help identify non-
modifiable and address modifiable bleeding risk factors in all AF patients, and to identify patients potentially at high risk of bleeding
who should be scheduled for early and more frequent clinical review and follow-up.
IB
Stroke and bleeding risk reassessment at periodic intervals is recommended to inform treatment decisions (e.g. initiation of OAC
in patients no longer at low risk of stroke) and address potentially modifiable bleeding risk factors.
IB
If a VKA is used, a target INR of 2.0 - 3.0 is recommended, with individual TTR>_70%.
IB
In patients on VKAs with low time in INR therapeutic range (e.g. TTR<70%), switching to a NOAC but ensuring good adherence
and persistence with therapy is recommended.
IB
Antiplatelet therapy alone (monotherapy or aspirin in combination with clopidogrel) is not recommended for stroke prevention
in AF.
III A
Estimated bleeding risk, in the absence of absolute contraindications to OAC, should not in itself guide treatment decisions to use
OAC for stroke prevention.
III A
Clinical pattern of AF (i.e. first detected, paroxysmal, persistent, long-standing persistent, permanent) should not condition the
indication to thromboprophylaxis.
III B
Recommendations for stroke risk management peri-cardioversion
In patients with AF undergoing cardioversion, NOACs are recommended with at least similar efficacy and safety as warfarin.
IA
For cardioversion of AF/AFL, effective anticoagulation is recommended for a minimum of 3 weeks before cardioversion.
IB
TOE is recommended to exclude cardiac thrombus as an alternative to 3-week pre-procedural anticoagulation when early cardi-
oversion is planned.
IB
In patients at risk of stroke, it is recommended that OAC therapy is continued long term after cardioversion according to the
long-term anticoagulation recommendations, irrespective of the method of cardioversion, the apparent maintenance of sinus
rhythm, or characterization of AF as a ‘first-diagnosed episode’.
IB
When thrombus is identified on TOE, effective anticoagulation is recommended for at least 3 weeks before cardioversion of AF.
IB
It is recommended that the importance of adherence and persistence to NOAC treatment both before and after cardioversion is
strongly emphasized to patients.
IC
Recommendations for stroke risk management peri-catheter ablation
In AF patients with stroke risk factors not taking OAC before ablation, it is recommended that pre-procedural management of
stroke risk includes initiation of anticoagulation and, preferably, therapeutic OAC for at least 3 weeks before ablation.
IC
Continued
ESC Guidelines 81

For patients undergoing AF catheter ablation who have been therapeutically anticoagulated with warfarin, dabigatran, rivaroxaban,
apixaban, or edoxaban, performance of the ablation procedure without OAC interruption is recommended.
IA
After AF catheter ablation, it is recommended that:
•
Systemic anticoagulation with warfarin or a NOAC is continued for at least 2 months post ablation, and
•
Long-term continuation of systemic anticoagulation beyond 2 months post ablation is based on the patient’s stroke risk profile
and not on the apparent success or failure of the ablation procedure.
IC
Recommendations for postoperative anticoagulation after AF surgery
Long-term OAC is recommended in patients after AF surgery and appendage closure, based on the patient’s thrombo-embolic
risk assessed with the CHA
2
DS
2
-VASc score.
IC
Recommendations for patients with AF and an ACS, PCI, or CCS
In AF patients eligible for NOACs, it is recommended to use a NOAC in preference to a VKA in combination with antiplatelet
therapy.
IA
In AF patients with ACS undergoing an uncomplicated PCI, early cessation (<_1 week) of aspirin and continuation of dual therapy
with an OAC and a P2Y
12
inhibitor (preferably clopidogrel) for up to 12 months is recommended if the risk of stent thrombosis
is low or if concerns about bleeding risk prevail over concerns about risk of stent thrombosis, irrespective of the type of stent
used.
IB
After uncomplicated PCI, early cessation (<_1 week) of aspirin and continuation of dual therapy with OAC for up to 6 months
and clopidogrel is recommended if the risk of stent thrombosis is low or if concerns about bleeding risk prevail over concerns
about risk of stent thrombosis, irrespective of the type of stent used.
IB
Recommendations for secondary stroke prevention in AF patients after acute ischaemic stroke
In AF patients with an ischaemic stroke or TIA, long-term secondary prevention of stroke using OAC is recommended if there is
no strict contraindication to OAC use, with a preference for NOACs over VKAs in NOAC-eligible patients.
IA
In AF patients presenting with acute ischaemic stroke, very early anticoagulation (<48 h) using UFH, LMWH, or VKAs is not
recommended.
III B
Recommendations for patients with valvular heart disease and AF
NOACs are contraindicated in patients with a prosthetic mechanical valve.
III B
Use of NOACs is not recommended in patients with AF and moderate-to-severe mitral stenosis.
III C
Recommendations for the management of AF during pregnancy
Therapeutic anticoagulation with heparin or VKA according to the stage of pregnancy is recommended for patients with AF.
IC
Recommendations for the management of active bleeding on OAC
In an AF patient with severe active bleeding, it is recommended to:
•
Interrupt OAC until the cause of bleeding is identified and active bleeding is resolved; and
•
Promptly perform specific diagnostic and treatment interventions to identify and manage the cause(s) and source(s) of
bleeding.
IC
Recommendations for ventricular rate control in patients with AF
Beta-blockers, diltiazem, or verapamil are recommended as first-choice drugs to control heart rate in AF patients with
LVEF>_40%.
IB
Beta-blockers and/or digoxin are recommended to control heart rate in AF patients with LVEF<40%.
IB
Recommendations for the management of AF during pregnancy
Beta-selective blockers are recommended for rate control in AF.
IC
Recommendations for rhythm control
Rhythm control therapy is recommended for symptom and QoL improvement in symptomatic patients with AF.
IA
Recommendations for cardioversion
For pharmacological cardioversion of new-onset AF, i.v. vernakalant (excluding patients with recent ACS or severe HF) or flecai-
nide or propafenone (excluding patients with severe structural heart disease) is recommended.
IA
Intravenous amiodarone is recommended for cardioversion of AF in patients with HF or structural heart disease, if delayed cardi-
oversion is consistent with clinical situation.
IA
Cardioversion of AF (either electrical or pharmacological) is recommended in symptomatic patients with persistent or long-
standing persistent AF as part of rhythm control therapy.
IB
Pharmacological cardioversion of AF is indicated only in a haemodynamically stable patient, after consideration of the thrombo-
embolic risk.
IB
Continued
82 ESC Guidelines

Emergency electrical cardioversion is recommended in AF patients with acute or worsening haemodynamic instability.
IB
For patients with sick-sinus syndrome, atrioventricular conduction disturbances or prolonged QTc (>500 ms), pharmacological
cardioversion should not be attempted unless risks for proarrhythmia and bradycardia have been considered.
III C
Recommendations for the management of AF during pregnancy
Immediate electrical cardioversion is recommended in case of haemodynamic instability or pre-excited AF.
IC
Recommendations for rhythm control/catheter ablation of AF
For the decision on AF catheter ablation, it is recommended to take into consideration the procedural risks and the major risk
factors for AF recurrence following the procedure and discuss them with the patient.
IB
AF catheter ablation after failure of drug therapy
AF catheter ablation for PVI is recommended for rhythm control after one failed or intolerant class I or III AAD, to improve
symptoms of AF recurrences in patients with:
I
•
Paroxysmal AF, or
A
•
Persistent AF without major risk factors for AF recurrence, or
A
•
Persistent AF with major risk factors for AF recurrence.
B
First-line therapy
AF catheter ablation is recommended to reverse LV dysfunction in AF patients when tachycardia-induced cardiomyopathy is
highly probable, independent of their symptom status.
IB
Techniques and technologies
Complete electrical isolation of the pulmonary veins is recommended during all AF catheter-ablation procedures.
IA
Lifestyle modification and other strategies to improve outcomes of ablation
Weight loss is recommended in obese patients with AF, particularly those who are being evaluated to undergo AF ablation.
IB
Strict control of risk factors and avoidance of triggers are recommended as part of a rhythm control strategy.
IB
Recommendations for long-term antiarrhythmic drugs
Flecainide or propafenone are recommended for long-term rhythm control in AF patients with normal LV function and without
structural heart disease, including significant LVH and myocardial ischaemia.
IA
Dronedarone is recommended for long-term rhythm control in AF patients with:
•
Normal or mildly impaired (but stable) LV function, or
•
HFpEF, ischaemic, or VHD.
IA
Amiodarone is recommended for long-term rhythm control in all AF patients, including those with HFrEF. However, owing to its
extracardiac toxicity, other AADs should be considered first whenever possible.
IA
In AF patients treated with sotalol, close monitoring of QT interval, serum potassium levels, CrCl, and other proarrhythmia risk
factors is recommended.
IB
AAD therapy is not recommended in patients with permanent AF under rate control and in patients with advanced conduction
disturbances unless antibradycardia pacing is provided.
III C
Recommendations for lifestyle interventions and management of risk factors and concomitant diseases in patients with AF
Identification and management of risk factors and concomitant diseases is recommended as an integral part of treatment in AF
patients.
IB
Modification of unhealthy lifestyle and targeted therapy of intercurrent conditions is recommended to reduce AF burden and
symptom severity.
IB
Opportunistic screening for AF is recommended in hypertensive patients.
IB
Attention to good BP control is recommended in AF patients with hypertension to reduce AF recurrences and risk of stroke and
bleeding.
IB
Recommendations for sports activity in patients with AF
It is recommended to counsel professional athletes that long-lasting intense sports participation may promote AF, while moderate
physical activity is recommended to prevent AF.
IB
Recommendations for postoperative AF
Perioperative amiodarone or beta blocker therapy is recommended for the prevention of postoperative AF after cardiac surgery.
IA
Beta-blockers should not be used routinely for the prevention of postoperative AF in patients undergoing non-cardiac surgery.
III B
Continued
ESC Guidelines 83

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
21 Supplementary data
Supplementary Data with additional Supplementary Figures, Tables,
and text complementing the full text are available on the European
Heart Journal website and via the ESC website at www.escardio.org/
guidelines.
22 Appendix
Author/Task Force Member Affiliations: Nikolaos Dagres,
Department of Electrophysiology, Heart Center Leipzig at the
University of Leipzig, Leipzig, Germany; Elena Arbelo,Arrhythmia
Department, Cardiovascular Institute, Hospital Clinic de Barcelona,
Barcelona, Catalonia, Spain; Jeroen J. Bax, Cardiology, Leiden
University Medical Center, Leiden, Netherlands; Carina
Blomstro¨m-Lundqvist, Department of Medical Science and
Cardiology, Medicine, Uppsala, Sweden; Giuseppe Boriani,
Cardiology Division, Department of Biomedical, Metabolic and
Neural Sciences, University of Modena and Reggio Emilia, Policlinico
di Modena, Modena, Italy; Manuel Castella,
1
Cardiovascular
Surgery, Hospital Cl
ınic, University of Barcelona, Barcelona, Spain;
Gheorghe-Andrei Dan, Cardiology Department, Internal
Medicine Clinic, ‘Carol Davila’ University of Medicine, Colentina
University Hospital, Bucharest, Romania; Polychronis E. Dilaveris,
1
st
University Department of Cardiology, National & Kapodistrian
University of Athens School of Medicine, Athens, Attica, Greece;
Laurent Fauchier, Department of Cardiology, Centre Hospitalier
Universitaire Trousseau and University of Tours, Tours, France;
Gerasimos Filippatos, Department of Cardiology, Attikon
University Hospital, National and Kapodistrian University of Athens,
Athens, Greece; Jonathan M. Kalman, Department of Cardiology,
Royal Melbourne Hospital and University of Melbourne, Melbourne,
Australia; Mark La Meir,
1
Cardiac surgery, UZ Brussel, Brussels,
Belgium; Deirdre A. Lane, Liverpool Centre for Cardiovascular
Science, University of Liverpool and Liverpool Heart & Chest
Hospital, Liverpool, United Kingdom, and Department of Clinical
Medicine, Aalborg University, Aalborg, Denmark; Jean-Pierre
Lebeau, Department of General Practice, University of Tours,
Tours, France; Maddalena Lettino, Cardiovascular, San Gerardo
Hospital, ASST-Monza, Monza, Italy; Gregory Y. H. Lip,Liverpool
Centre for Cardiovascular Science, University of Liverpool and
Liverpool Heart & Chest Hospital, Liverpool, United Kingdom, and
Department of Clinical Medicine, Aalborg University, Aalborg,
Denmark; Fausto J. Pinto, Cardiology, CCUL, Faculdade de
Medicina, Universidade de Lisboa, Lisbon, Portugal; G. Neil
Thomas, Institute of Applied Health Research, University of
Birmingham, Birmingham, United Kingdom; Marco Valgimigli,
Cardiocentro Ticino, Lugano, Switzerland; Isabelle C. Van
Gelder, Department of Cardiology, University of Groningen,
University Medical Center Groningen, Groningen, Netherlands; Bart
P. Van Putte,
1
Cardiothoracic Surgery, St Antonius Hospital,
Nieuwegein, Netherlands; Caroline L. Watkins, Faculty of Health
and Wellbeing, University of Central Lancashire, Preston, United
Kingdom.
ESC Committee for Practice Guidelines (CPG):Stephan
Windecker (Chairperson) (Switzerland), Victor Aboyans (France),
Colin Baigent (United Kingdom), Jean-Philippe Collet (France),
Veronica Dean (France), Victoria Delgado (Netherlands), Donna
Fitzsimons (United Kingdom), Chris P. Gale (United Kingdom),
Diederick E. Grobbee (Netherlands), Sigrun Halvorsen (Norway),
Gerhard Hindricks (Germany), Bernard Iung (France), Peter Ju¨ni
(Canada), Hugo A. Katus (Germany), Ulf Landmesser (Germany),
Christophe Leclercq (France), Maddalena Lettino (Italy), Basil S.
Lewis (Israel), Be´la Merkely (Hungary), Christian Mueller
(Switzerland), Steffen E. Petersen (United Kingdom), Anna Sonia
Petronio (Italy), Dimitrios J. Richter (Greece), Marco Roffi
(Switzerland), Evgeny Shlyakhto (Russian Federation), Iain A.
Simpson (United Kingdom), Miguel Sousa-Uva (Portugal), Rhian M.
Touyz (United Kingdom).
ESC National Cardiac Societies actively involved in the review
process of the 2020 ESC Guidelines for the diagnosis and manage-
ment of atrial fibrillation.
Algeria: Algerian Society of Cardiology, Tahar Delassi; Armenia:
Armenian Cardiologists Association, Hamayak S. Sisakian; Austria:
Austrian Society of Cardiology, Daniel Scherr; Belarus:Belorussian
Scientific Society of Cardiologists, Alexandr Chasnoits; Belgium:
Belgian Society of Cardiology, Michel De Pauw; Bosnia and
Herzegovina: Association of Cardiologists of Bosnia and
Herzegovina, Elnur Smaji
c; Bulgaria: Bulgarian Society of
Cardiology, Tchavdar Shalganov; Cyprus: Cyprus Society of
Cardiology, Panayiotis Avraamides; Czech Republic: Czech
Society of Cardiology, Josef Kautzner; Denmark: Danish Society of
Cardiology, Christian Gerdes; Egypt: Egyptian Society of
Cardiology, Ahmad Abd Alaziz; Estonia: Estonian Society of
Cardiology, Priit Kampus; Finland: Finnish Cardiac Society, Pekka
Raatikainen; France: French Society of Cardiology, Serge Boveda;
Recommendations pertaining to sex-related differences in AF
It is recommended that women and men with AF are equally offered diagnostic assessment and therapies to prevent stroke and
other AF-related complications.
IA
AAD = antiarrhythmic drug; ACS = acute coronary syndrome; AF = atrial fibrillation; AFL = atrial flutter; AHRE = atrial high-rate episodes; BP = blood pressure; CCS = chronic
coronary syndrome; CHA
2
DS
2
-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 6574 years, Sex category
(female); CIED = cardiac implantable electronic device; CrCl = creatinine clearance; ECG = electrocardiogram; HF = heart failure; HFpEF = heart failure with preserved ejec-
tion fraction; HFrEF = heart failure with reduced ejection fraction; i.v. = intravenous; INR = international normalized ratio; LMWH = low-molecular-weight heparin; LV = left
ventricular; LVEF = left ventricular ejection fraction; LVH = left ventricular hypertrophy; NOAC = non-vitamin K antagonist oral anticoagulant; OAC = oral anticoagulant; PCI
= percutaneous coronary intervention; PRO = patient-reported outcome; PVI = pulmonary vein isolation; QoL = quality of life; TIA = transient ischaemic attack; TOE = trans-
oesophageal echocardiography; TTR = time in therapeutic range; UFH = unfractionated heparin; VHD = Valvular heart disease; VKA = vitamin K antagonist.
84 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Georgia: Georgian Society of Cardiology, Giorgi Papiashvili;
Germany: German Cardiac Society, Lars Eckardt; Greece:
Hellenic Society of Cardiology, Vassilios P. Vassilikos; Hungary:
Hungarian Society of Cardiology, Zolt
an Csan
adi; Iceland: Icelandic
Society of Cardiology, David O. Arnar; Ireland: Irish Cardiac
Society, Joseph Galvin; Israel: Israel Heart Society, Alon Barsheshet;
Italy: Italian Federation of Cardiology, Pasquale Caldarola;
Kazakhstan: Association of Cardiologists of Kazakhstan, Amina
Rakisheva; Kosovo (Republic of): Kosovo Society of Cardiology,
Ibadete Bytyc¸i; Kyrgyzstan: Kyrgyz Society of Cardiology, Alina
Kerimkulova; Latvia: Latvian Society of Cardiology, Oskars Kalejs;
Lebanon: Lebanese Society of Cardiology, Mario Njeim;
Lithuania: Lithuanian Society of Cardiology, Aras Puodziukynas;
Luxembourg: Luxembourg Society of Cardiology, Laurent
Groben; Malta: Maltese Cardiac Society, Mark A. Sammut;
Moldova (Republic of): Moldavian Society of Cardiology, Aurel
Grosu; Montenegro: Montenegro Society of Cardiology, Aneta
Boskovic; Morocco: Moroccan Society of Cardiology, Abdelhamid
Moustaghfir; Netherlands: Netherlands Society of Cardiology,
Natasja de Groot; North Macedonia: North Macedonian Society
of Cardiology, Lidija Poposka; Norway: Norwegian Society of
Cardiology, Ole-Gunnar Anfinsen; Poland: Polish Cardiac Society,
Przemyslaw P. Mitkowski; Portugal: Portuguese Society of
Cardiology, Diogo Magalh
~
aes Cavaco; Romania: Romanian Society
of Cardiology, Calin Siliste; Russian Federation: Russian Society of
Cardiology, Evgeny N. Mikhaylov; San Marino: San Marino Society
of Cardiology, Luca Bertelli; Serbia: Cardiology Society of Serbia,
Dejan Kojic; Slovakia: Slovak Society of Cardiology, Robert Hatala;
Slovenia: Slovenian Society of Cardiology, Zlatko Fras; Spain:
Spanish Society of Cardiology, Fernando Arribas; Sweden: Swedish
Society of Cardiology, Tord Juhlin; Switzerland: Swiss Society of
Cardiology, Christian Sticherling; Tunisia: Tunisian Society of
Cardiology and Cardio-Vascular Surgery, Leila Abid; Tu r k e y :
Turkish Society of Cardiology, Ilyas Atar; Ukraine: Ukrainian
Association of Cardiology, Oleg Sychov;
United Kingdom of
Great Britain and Northern Ireland: British Cardiovascular
Society, Matthew G. D. Bates; Uzbekistan: Association of
Cardiologists of Uzbekistan, Nodir U. Zakirov.
23 References
1. Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, Akar JG,
Badhwar V, Brugada J, Camm J, Chen PS, Chen SA, Chung MK, Nielsen JC, Curtis
AB, Davies DW, Day JD, d’Avila A, de Groot N, Di Biase L, Duytschaever M,
Edgerton JR, Ellenbogen KA, Ellinor PT, Ernst S, Fenelon G, Gerstenfeld EP,
Haines DE, Haissaguerre M, Helm RH, Hylek E, Jackman WM, Jalife J, Kalman JM,
Kautzner J, Kottkamp H, Kuck KH, Kumagai K, Lee R, Lewalter T, Lindsay BD,
Macle L, Mansour M, Marchlinski FE, Michaud GF, Nakagawa H, Natale A, Nattel
S, Okumura K, Packer D, Pokushalov E, Reynolds MR, Sanders P, Scanavacca M,
Schilling R, Tondo C, Tsao HM, Verma A, Wilber DJ, Yamane T. 2017 HRS/
EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and sur-
gical ablation of atrial fibrillation: executive summary. Europace 2018;20:157208.
2. Charitos EI, Stierle U, Ziegler PD, Baldewig M, Robinson DR, Sievers HH, Hanke
T. A comprehensive evaluation of rhythm monitoring strategies for the detection
of atrial fibrillation recurrence: insights from 647 continuously monitored patients
and implications for monitoring after therapeutic interventions. Circulation
2012;126:806814.
3. Gorenek B, Boriani G, Dan GA, Fauchier L, Fenelon G, Huang H, Kudaiberdieva
G, Lip GYH, Mahajan R, Potpara T, Ramirez JD, Vos MA, Marin F, ESC Scientific
Document Group. European Heart Rhythm Association (EHRA) position paper
on arrhythmia management and device therapies in endocrine disorders, endorsed
by Asia Pacific Heart Rhythm Society (APHRS) and Latin American Heart Rhythm
Society (LAHRS). Europace 2018;20:895896.
4. Freedman B, Boriani G, Glotzer TV, Healey JS, Kirchhof P, Potpara TS.
Management of atrial high-rate episodes detected by cardiac implanted electronic
devices. Nat Rev Cardiol 2017;14:701714.
5. Perino AC, Fan J, Askari M, Heidenreich PA, Keung E, Raitt MH, Piccini JP, Ziegler
PD, Turakhia MP. Practice variation in anticoagulation prescription and outcomes
after device-detected atrial fibrillation. Circulation 2019;139:25022512.
6. Steinberg JS, O’Connell H, Li S, Ziegler PD. Thirty-second gold standard definition
of atrial fibrillation and its relationship with subsequent arrhythmia patterns: analy-
sis of a large prospective device database. Circ Arrhythm Electrophysiol
2018;11:e006274.
7. Camm AJ, Simantirakis E, Goette A, Lip GY, Vardas P, Calvert M, Chlouverakis G,
Diener HC, Kirchhof P. Atrial high-rate episodes and stroke prevention. Europace
2017;19:169179.
8. Pollak WM, Simmons JD, Interian A, Jr., Atapattu SA, Castellanos A, Myerburg RJ,
Mitrani RD. Clinical utility of intraatrial pacemaker stored electrograms to diag-
nose atrial fibrillation and flutter. Pacing Clin Electrophysiol 2001;24:424429.
9. Kaufman ES, Israel CW, Nair GM, Armaganijan L, Divakaramenon S, Mairesse GH,
Brandes A, Crystal E, Costantini O, Sandhu RK, Parkash R, Connolly SJ,
Hohnloser SH, Healey JS; ASSERT Steering Committee and Investigators. Positive
predictive value of device-detected atrial high-rate episodes at different rates and
durations: an analysis from ASSERT. Heart Rhythm 2012;9:12411246.
10. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP,
Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind
MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL,
Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS,
Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M,
Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM,
Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW,
Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS, American Heart
Association Council on Epidemiology and Prevention Statistics Committee and
Stroke Statistics Subcommittee. Heart disease and stroke statistics 2019
update: a report from the American Heart Association. Circulation
2019;139:e56e528.
11. Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum
RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA,
Ezzati M, Murray CJ. Worldwide epidemiology of atrial fibrillation: a Global
Burden of Disease 2010 Study. Circulation 2014;129:837
847.
12. Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current
and future incidence and prevalence of atrial fibrillation in the US adult popula-
tion. Am J Cardiol 2013;112:11421147.
13. Krijthe BP, Kunst A, Benjamin EJ, Lip GY, Franco OH, Hofman A, Witteman JC,
Stricker BH, Heeringa J. Projections on the number of individuals with atrial fibril-
lation in the European Union, from 2000 to 2060. Eur Heart J
2013;34:27462751.
14. Dewland TA, Olgin JE, Vittinghoff E, Marcus GM. Incident atrial fibrillation among
Asians, Hispanics, blacks, and whites. Circulation 2013;128:24702477.
15. Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial fibrillation: epidemiology,
pathophysiology, and clinical outcomes. Circ Res 2017;120:15011517.
16. Alonso A, Agarwal SK, Soliman EZ, Ambrose M, Chamberlain AM, Prineas RJ,
Folsom AR. Incidence of atrial fibrillation in whites and African Americans: the
Atherosclerosis Risk in Communities (ARIC) study. Am Heart J
2009;158:111117.
17. Chao TF, Liu CJ, Tuan TC, Chen TJ, Hsieh MH, Lip GYH, Chen SA. Lifetime
risks, projected numbers, and adverse outcomes in Asian patients with atrial
fibrillation: a report from the Taiwan Nationwide AF Cohort Study. Chest
2018;153:453466.
18. Guo Y, Tian Y, Wang H, Si Q, Wang Y, Lip GYH. Prevalence, incidence, and life-
time risk of atrial fibrillation in China: new insights into the global burden of atrial
fibrillation. Chest 2015;147:109119.
19. Ko D, Rahman F, Schnabel RB, Yin X, Benjamin EJ, Christophersen IE. Atrial fibril-
lation in women: epidemiology, pathophysiology, presentation, and prognosis.
Nat Rev Cardiol 2016;13:321332.
20. Mou L, Norby FL, Chen LY, O’Neal WT, Lewis TT, Loehr LR, Soliman EZ,
Alonso A. Lifetime risk of atrial fibrillation by race and socioeconomic status:
ARIC study (Atherosclerosis Risk in Communities). Circ Arrhythm Electrophysiol
2018;11:e006350.
21. Boriani G, Savelieva I, Dan GA, Deharo JC, Ferro C, Israel CW, Lane DA, La Manna
G, Morton J, Mitjans AM, Vos MA, Turakhia MP, Lip GY. Chronic kidney disease in
patients with cardiac rhythm disturbances or implantable electrical devices: clinical
significance and implications for decision making a position paper of the European
Heart Rhythm Association endorsed by the Heart Rhythm Society and the Asia
Pacific Heart Rhythm Society. Europace 2015;17:11691196.
ESC Guidelines 85

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
22. Aune D, Feng T, Schlesinger S, Janszky I, Norat T, Riboli E. Diabetes mellitus,
blood glucose and the risk of atrial fibrillation: a systematic review and meta-
analysis of cohort studies. J Diabetes Complications 2018;32:501511.
23. Cadby G, McArdle N, Briffa T, Hillman DR, Simpson L, Knuiman M, Hung J.
Severity of OSA is an independent predictor of incident atrial fibrillation hospital-
ization in a large sleep-clinic cohort. Chest 2015;148:945952.
24. Hobbelt AH, Siland JE, Geelhoed B, Van Der Harst P, Hillege HL, Van Gelder IC,
Rienstra M. Clinical, biomarker, and genetic predictors of specific types of atrial
fibrillation in a community-based cohort: data of the PREVEND study. Europace
2017;19:226232.
25. Nalliah CJ, Sanders P, Kalman JM. The impact of diet and lifestyle on atrial fibrilla-
tion. Curr Cardiol Rep 2018;20:137.
26. Lip GYH, Coca A, Kahan T, Boriani G, Manolis AS, Olsen MH, Oto A, Potpara
TS, Steffel J, Marin F, de Oliveira Figueiredo MJ, de Simone G, Tzou WS, Chiang
CE, Williams B, Reviewers, Dan GA, Gorenek B, Fauchier L, Savelieva I, Hatala R,
van Gelder I, Brguljan-Hitij J, Erdine S, Lovic D, Kim YH, Salinas-Arce J, Field M.
Hypertension and cardiac arrhythmias: a consensus document from the
European Heart Rhythm Association (EHRA) and ESC Council on Hypertension,
endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm
Society (APHRS) and Sociedad Latinoamericana de Estimulacion Cardiaca y
Electrofisiologia (SOLEACE). Europace 2017;19:891911.
27. Gallagher C, Hendriks JML, Elliott AD, Wong CX, Rangnekar G, Middeldorp ME,
Mahajan R, Lau DH, Sanders P. Alcohol and incident atrial fibrillation a system-
atic review and meta-analysis. Int J Cardiol 2017;246:4652.
28. Ricci C, Gervasi F, Gaeta M, Smuts CM, Schutte AE, Leitzmann MF. Physical
activity volume in relation to risk of atrial fibrillation. A non-linear meta-regres-
sion analysis. Eur J Prev Cardiol 2018;25:857866.
29. Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH,
Stijnen T, Lip GY, Witteman JC. Prevalence, incidence and lifetime risk of atrial
fibrillation: the Rotterdam Study. Eur Heart J 2006;27:949953.
30. Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, D’Agostino
RB, Massaro JM, Beiser A, Wolf PA, Benjamin EJ. Lifetime risk for development
of atrial fibrillation: the Framingham Heart Study. Circulation 2004;110:1042-
1046.
31. Magnussen C, Niiranen TJ, Ojeda FM, Gianfagna F, Blankenberg S, Njolstad I,
Vartiainen E, Sans S, Pasterkamp G, Hughes M, Costanzo S, Donati MB, Jousilahti
P, Linneberg A, Palosaari T, de Gaetano G, Bobak M, den Ruijter HM, Mathiesen
E, Jorgensen T, Soderberg S, Kuulasmaa K, Zeller T, Iacoviello L, Salomaa V,
Schnabel RB, BiomarCaRE Consortium. Sex differences and similarities in atrial
fibrillation epidemiology, risk factors, and mortality in community cohorts: results
from the BiomarCaRE Consortium (Biomarker for Cardiovascular Risk Assessment
in Europe). Circulation 2017;136:15881597.
32. Staerk L, Wang B, Preis SR, Larson MG, Lubitz SA, Ellinor PT, McManus DD, Ko
D, Weng LC, Lunetta KL, Frost L, Benjamin EJ, Trinquart L. Lifetime risk of atrial
fibrillation according to optimal, borderline, or elevated levels of risk factors:
cohort study based on longitudinal data from the Framingham Heart Study. BMJ
2018;361:k1453.
33. Allan V, Honarbakhsh S, Casas JP, Wallace J, Hunter R, Schilling R, Perel P,
Morley K, Banerjee A, Hemingway H. Are cardiovascular risk factors also associ-
ated with the incidence of atrial fibrillation? A systematic review and field synop-
sis of 23 factors in 32 population-based cohorts of 20 million participants.
Thromb Haemost 2017;117
:837850.
34. Feghaly J, Zakka P, London B, MacRae CA, Refaat MM. Genetics of atrial fibrilla-
tion. J Am Heart Assoc 2018;7:e009884.
35. Abdulla J, Nielsen JR. Is the risk of atrial fibrillation higher in athletes than in the
general population? A systematic review and meta-analysis. Europace
2009;11:11561159.
36. Alonso A, Jensen PN, Lopez FL, Chen LY, Psaty BM, Folsom AR, Heckbert SR.
Association of sick sinus syndrome with incident cardiovascular disease and mor-
tality: the Atherosclerosis Risk in Communities Study and Cardiovascular Health
Study. PLoS One 2014;9:e109662.
37. Alonso A, Lopez FL, Matsushita K, Loehr LR, Agarwal SK, Chen LY, Soliman EZ,
Astor BC, Coresh J. Chronic kidney disease is associated with the incidence of
atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study.
Circulation 2011;123:29462953.
38. Andersen K, Farahmand B, Ahlbom A, Held C, Ljunghall S, Michaelsson K,
Sundstrom J. Risk of arrhythmias in 52 755 long-distance cross-country skiers: a
cohort study. Eur Heart J 2013;34:36243631.
39. Asad Z, Abbas M, Javed I, Korantzopoulos P, Stavrakis S. Obesity is associated
with incident atrial fibrillation independent of gender: a meta-analysis. J Cardiovasc
Electrophysiol 2018;29:725732.
40. Aune D, Sen A, Schlesinger S, Norat T, Janszky I, Romundstad P, Tonstad S,
Riboli E, Vatten LJ. Body mass index, abdominal fatness, fat mass and the risk of
atrial fibrillation: a systematic review and dose-response meta-analysis of pro-
spective studies. Eur J Epidemiol 2017;32:181192.
41. Bansal N, Zelnick LR, Alonso A, Benjamin EJ, de Boer IH, Deo R, Katz R,
Kestenbaum B, Mathew J, Robinson-Cohen C, Sarnak MJ, Shlipak MG,
Sotoodehnia N, Young B, Heckbert SR. eGFR and albuminuria in relation to risk
of incident atrial fibrillation: a meta-analysis of the Jackson Heart Study, the
Multi-Ethnic Study of Atherosclerosis, and the Cardiovascular Health Study. Clin J
Am Soc Nephrol 2017;12:13861398.
42. Baumgartner C, da Costa BR, Collet TH, Feller M, Floriani C, Bauer DC,
Cappola AR, Heckbert SR, Ceresini G, Gussekloo J, den Elzen WPJ, Peeters RP,
Luben R, Volzke H, Dorr M, Walsh JP, Bremner A, Iacoviello M, Macfarlane P,
Heeringa J, Stott DJ, Westendorp RGJ, Khaw KT, Magnani JW, Aujesky D,
Rodondi N, Thyroid Studies Collaboration. Thyroid function within the normal
range, subclinical hypothyroidism, and the risk of atrial fibrillation. Circulation
2017;136:21002116.
43. Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA.
Independent risk factors for atrial fibrillation in a population-based cohort. The
Framingham Heart Study. JAMA 1994;271:840844.
44. Bunch TJ, May HT, Bair TL, Anderson JL, Crandall BG, Cutler MJ, Jacobs V,
Mallender C, Muhlestein JB, Osborn JS, Weiss JP, Day JD. Long-term natural his-
tory of adult Wolff-Parkinson-White syndrome patients treated with and with-
out catheter ablation. Circ Arrhythm Electrophysiol 2015;8:14651471.
45. Chang SH, Kuo CF, Chou IJ, See LC, Yu KH, Luo SF, Huang LH, Zhang W,
Doherty M, Wen MS, Kuo CT, Yeh YH. Association of a family history of atrial
fibrillation with incidence and outcomes of atrial fibrillation: a population-based
family cohort study. JAMA Cardiol 2017;2:863870.
46. Chen LY, Leening MJ, Norby FL, Roetker NS, Hofman A, Franco OH, Pan W,
Polak JF, Witteman JC, Kronmal RA, Folsom AR, Nazarian S, Stricker BH,
Heckbert SR, Alonso A. Carotid intima-media thickness and arterial stiffness and
the risk of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC)
study, Multi-Ethnic Study of Atherosclerosis (MESA), and the Rotterdam Study. J
Am Heart Assoc 2016;5.
47. Cheng M, Hu Z, Lu X, Huang J, Gu D. Caffeine intake and atrial fibrillation inci-
dence: dose response meta-analysis of prospective cohort studies. Can J Cardiol
2014;30:448454.
48. Cheng S, Keyes MJ, Larson MG, McCabe EL, Newton-Cheh C, Levy D, Benjamin
EJ, Vasan RS, Wang TJ. Long-term outcomes in individuals with prolonged PR
interval or first-degree atrioventricular block. JAMA 2009;301:25712577.
49. Conen D, Chiuve SE, Everett BM, Zhang SM, Buring JE, Albert CM. Caffeine con-
sumption and incident atrial fibrillation in women. Am J Clin Nutr 2010;92:509514.
50. Desai R, Patel U, Singh S, Bhuva R, Fong HK, Nunna P, Zalavadia D, Dave H,
Savani S, Doshi R. The burden and impact of arrhythmia in chronic obstructive
pulmonary disease: insights from the National Inpatient Sample. Int J Cardiol
2019;281:4955.
51. Eaker ED, Sullivan LM, Kelly-Hayes M, D’Agostino RB Sr, Benjamin EJ. Anger and
hostility predict the development of atrial fibrillation in men in the Framingham
Offspring Study. Circulation 2004;109:12671271.
52. Fox CS, Parise H, D’Agostino RB Sr, Lloyd-Jones DM, Vasan RS, Wang TJ, Levy
D, Wolf PA, Benjamin EJ. Parental atrial fibrillation as a risk factor for atrial fibril-
lation in offspring. JAMA 2004;291:28512855.
53. Furberg CD, Psaty BM, Manolio TA, Gardin JM, Smith VE, Rautaharju PM.
Prevalence of atrial fibrillation in elderly subjects (the Cardiovascular Health
Study). Am J Cardiol 1994;74:236241.
54. Giacomantonio NB, Bredin SS, Foulds HJ, Warburton DE. A systematic review
of the health benefits of exercise rehabilitation in persons living with atrial fibril-
lation. Can J Cardiol 2013;29:483491.
55. Kirchhof P, Lip GY, Van Gelder IC, Bax J, Hylek E, Kaab S, Schotten U,
Wegscheider K, Boriani G, Brandes A, Ezekowitz M, Diener H, Haegeli L,
Heidbuchel H, Lane D, Mont L, Willems S, Dorian P, Aunes-Jansson M,
Blomstrom-Lundqvist C, Borentain M, Breitenstein S, Brueckmann M, Cater N,
Clemens A, Dobrev D, Dubner S, Edvardsson NG, Friberg L, Goette A, Gulizia
M, Hatala R, Horwood J, Szumowski L, Kappenberger L, Kautzner J, Leute A,
Lobban T, Meyer R, Millerhagen J, Morgan J, Muenzel F, Nabauer M, Baertels C,
Oeff M, Paar D, Polifka J, Ravens U, Rosin L, Stegink W, Steinbeck G, Vardas P,
Vincent A, Walter M, Breithardt G, Camm AJ. Comprehensive risk reduction in
patients with atrial fibrillation: emerging diagnostic and therapeutic options a
report from the 3rd Atrial Fibrillation Competence NETwork/European Heart
Rhythm Association consensus conference. Europace 2012;14:827.
56. Ko D, Benson MD, Ngo D, Yang Q, Larson MG, Wang TJ, Trinquart L, McManus
DD, Lubitz SA, Ellinor PT, Vasan RS, Gerszten RE, Benjamin EJ, Lin H.
Proteomics profiling and risk of new-onset atrial fibrillation: Framingham Heart
Study. J Am Heart Assoc 2019;
8:e010976.
57. Kwok CS, Anderson SG, Myint PK, Mamas MA, Loke YK. Physical activity and
incidence of atrial fibrillation: a systematic review and meta-analysis. Int J Cardiol
2014;177:467476.
58. Lip GYH, Collet JP, de Caterina R, Fauchier L, Lane DA, Larsen TB, Marin F,
Morais J, Narasimhan C, Olshansky B, Pierard L, Potpara T, Sarrafzadegan N,
86 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Sliwa K, Varela G, Vilahur G, Weiss T, Boriani G, Rocca B. Antithrombotic ther-
apy in atrial fibrillation associated with valvular heart disease: executive summary
of a joint consensus document from the European Heart Rhythm Association
(EHRA) and European Society of Cardiology Working Group on Thrombosis,
Endorsed by the ESC Working Group on Valvular Heart Disease, Cardiac
Arrhythmia Society of Southern Africa (CASSA), Heart Rhythm Society (HRS),
Asia Pacific Heart Rhythm Society (APHRS), South African Heart (SA Heart)
Association and Sociedad Latinoamericana de Estimulacion Cardiaca y
Electrofisiologia (SOLEACE). Thromb Haemost 2017;117:22152236.
59. Loomba RS, Buelow MW, Aggarwal S, Arora RR, Kovach J, Ginde S. Arrhythmias
in adults with congenital heart disease: what are risk factors for specific
arrhythmias?Pacing Clin Electrophysiol 2017;40:353361.
60. Lubitz SA, Yin X, Fontes JD, Magnani JW, Rienstra M, Pai M, Villalon ML, Vasan
RS, Pencina MJ, Levy D, Larson MG, Ellinor PT, Benjamin EJ. Association between
familial atrial fibrillation and risk of new-onset atrial fibrillation. JAMA
2010;304:22632269.
61. May AM, Blackwell T, Stone PH, Stone KL, Cawthon PM, Sauer WH, Varosy PD,
Redline S, Mehra R, Sleep MrOS (Outcomes of Sleep Disorders in Older Men)
Study Group. Central sleep-disordered breathing predicts incident atrial fibrilla-
tion in older men. Am J Respir Crit Care Med 2016;193:783791.
62. Michniewicz E, Mlodawska E, Lopatowska P, Tomaszuk-Kazberuk A, Malyszko J.
Patients with atrial fibrillation and coronary artery disease double trouble. Adv
Med Sci 2018;63:3035.
63. Monrad M, Sajadieh A, Christensen JS, Ketzel M, Raaschou-Nielsen O,
Tjonneland A, Overvad K, Loft S, Sorensen M. Long-term exposure to traffic-
related air pollution and risk of incident atrial fibrillation: a cohort study. Environ
Health Perspect 2017;125:422427.
64. O’Neal WT, Efird JT, Qureshi WT, Yeboah J, Alonso A, Heckbert SR, Nazarian
S, Soliman EZ. Coronary artery calcium progression and atrial fibrillation:
the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging 2015;8:pii:
e003786.
65. Qureshi WT, Alirhayim Z, Blaha MJ, Juraschek SP, Keteyian SJ, Brawner CA, Al-
Mallah MH. Cardiorespiratory fitness and risk of incident atrial fibrillation: results
from the Henry Ford Exercise Testing (FIT) Project. Circulation
2015;131:18271834.
66. Santhanakrishnan R, Wang N, Larson MG, Magnani JW, McManus DD, Lubitz SA,
Ellinor PT, Cheng S, Vasan RS, Lee DS, Wang TJ, Levy D, Benjamin EJ, Ho JE.
Atrial fibrillation begets heart failure and vice versa: temporal associations and
differences in preserved versus reduced ejection fraction. Circulation
2016;133:484492.
67. Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, Newton-
Cheh C, Lubitz SA, Magnani JW, Ellinor PT, Seshadri S, Wolf PA, Vasan RS,
Benjamin EJ, Levy D. 50-Year trends in atrial fibrillation prevalence, incidence,
risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet
2015;386:154162.
68. Shen J, Johnson VM, Sullivan LM, Jacques PF, Magnani JW, Lubitz SA, Pandey S,
Levy D, Vasan RS, Quatromoni PA, Junyent M, Ordovas JM, Benjamin EJ. Dietary
factors and incident atrial fibrillation: the Framingham Heart Study. Am J Clin Nutr
2011;93:261266.
69. Svensson T, Kitlinski M, Engstrom G, Melander O. Psychological stress and risk
of incident atrial fibrillation in men and women with known atrial fibrillation
genetic risk scores. Sci Rep 2017;7:42613.
70. Tung P, Levitzky YS, Wang R, Weng J, Quan SF, Gottlieb DJ, Rueschman M,
Punjabi NM, Mehra R, Bertisch S, Benjamin EJ, Redline S. Obstructive and central
sleep apnea and the risk of incident atrial fibrillation in a community cohort of
men and women. J Am Heart Assoc 2017;6:pii.
71. Walkey AJ, Greiner MA, Heckbert SR, Jensen PN, Piccini JP, Sinner MF, Curtis
LH, Benjamin EJ. Atrial fibrillation among Medicare beneficiaries hospitalized with
sepsis: incidence and risk factors. Am Heart J 2013;165:949955.e3.
72. Zoller B, Ohlsson H, Sundquist J, Sundquist K. High familial risk of atrial fibrilla-
tion/atrial flutter in multiplex families: a nationwide family study in Sweden. JAm
Heart Assoc 2012;2:e003384.
73. Lip GYH, Skjoth F, Nielsen PB, Larsen TB. Evaluation of the C2HEST risk score
as a possible opportunistic screening tool for incident atrial fibrillation in a
healthy population (from a nationwide Danish cohort study). Am J Cardiol
2020;125:4854.
74. Yiin GSC, Li L, Bejot Y, Rothwell PM. Time trends in atrial fibrillation-associated
stroke and premorbid anticoagulation. Stroke 2018:STROKEAHA118022249.
75. Akao M, Chun YH, Wada H, Esato M, Hashimoto T, Abe M, Hasegawa K, Tsuji
H, Furuke K; Fushimi AFRegistry Investigators. Current status of clinical back-
ground of patients with atrial fibrillation in a community-based survey: the
Fushimi AF Registry. J Cardiol 2013;61:260266.
76. An Y, Ogawa H, Yamashita Y, Ishii M, Iguchi M, Masunaga N, Esato M, Tsuji H,
Wada H, Hasegawa K, Abe M, Lip GYH, Akao M. Causes of death in Japanese
patients with atrial fibrillation: the Fushimi Atrial Fibrillation Registry. Eur Heart J
Qual Care Clin Outcomes 2019;5:3542.
77. Andersson T, Magnuson A, Bryngelsson IL, Frobert O, Henriksson KM,
Edvardsson N, Poci D. All-cause mortality in 272,186 patients hospitalized with
incident atrial fibrillation 19952008: a Swedish nationwide long-term case-con-
trol study. Eur Heart J 2013;34:10611067.
78. Andrew NE, Thrift AG, Cadilhac DA. The prevalence, impact and economic
implications of atrial fibrillation in stroke: what progress has been
made?Neuroepidemiology 2013;40:227239.
79. Bakhai A, Darius H, De Caterina R, Smart A, Le Heuzey JY, Schilling RJ,
Zamorano JL, Shah M, Bramlage P, Kirchhof P. Characteristics and outcomes of
atrial fibrillation patients with or without specific symptoms: results from the
PREFER in AF registry. Eur Heart J Qual Care Clin Outcomes 2016;2:299305.
80. Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact
of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation
1998;98:946952.
81. Blum S, Muff C, Aeschbacher S, Ammann P, Erne P, Moschovitis G, Di Valentino
M, Shah D, Schlapfer J, Fischer A, Merkel T, Kuhne M, Sticherling C, Osswald S,
Conen D. Prospective assessment of sex-related differences in symptom status
and health perception among patients with atrial fibrillation. J Am Heart Assoc
2017;6:e005401.
82. Boriani G, Laroche C, Diemberger I, Fantecchi E, Popescu MI, Rasmussen LH,
Sinagra G, Petrescu L, Tavazzi L, Maggioni AP, Lip GY. Asymptomatic atrial fibril-
lation: clinical correlates, management, and outcomes in the EORP-AF Pilot
General Registry. Am J Med 2015;128:509518.e2.
83. Ceornodolea AD, Bal R, Severens JL. Epidemiology and management of atrial
fibrillation and stroke: review of data from four European countries. Stroke Res
Treat 2017;2017:8593207.
84. Chao TF, Lip GY, Liu CJ, Tuan TC, Chen SJ, Wang KL, Lin YJ, Chang SL, Lo LW,
Hu YF, Chen TJ, Chiang CE, Chen SA. Validation of a modified CHA2DS2-VASc
score for stroke risk stratification in Asian patients with atrial fibrillation: a
nationwide cohort study. Stroke 2016;47:24622469.
85. Chao T-F, Liu C-J, Wang K-L, Lin Y-J, Chang S-L, Lo L-W, Hu Y-F, Tuan T-C,
Chen T-J, Lip GY. Should atrial fibrillation patients with 1 additional risk factor of
the CHA2DS2-VASc score (beyond sex) receive oral anticoagulation?J Am Coll
Cardiol 2015;65:635642.
86. Dagres N, Chao T-F, Fenelon G, Aguinaga L, Benhayon D, Benjamin EJ, Bunch TJ,
Chen LY, Chen S-A, Darrieux F, de Paola A, Fauchier L, Goette A, Kalman J,
Kalra L, Kim Y-H, Lane DA, Lip GYH, Lubitz SA, M
arquez MF, Potpara T, Pozzer
DL, Ruskin JN, Savelieva I, Teo WS, Tse H-F, Verma A, Zhang S, Chung MK,
Bautista-Vargas W-F, Chiang C-E, Cuesta A, Dan G-A, Frankel DS, Guo Y,
Hatala R, Lee YS, Murakawa Y, Pellegrini CN, Pinho C, Milan DJ, Morin DP,
Nadalin E, Ntaios G, Prabhu MA, Proietti M, Rivard L, Valentino M, Shantsila A.
European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia
Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society
(LAHRS) expert consensus on arrhythmias and cognitive function: what is the
best practice?EP Europace 2018;20:13991421.
87. Esato M, Chun YH, An Y, Ogawa H, Wada H, Hasegawa K, Tsuji H, Abe M, Lip
GYH, Akao M. Clinical impact of asymptomatic presentation status in patients
with paroxysmal and sustained atrial fibrillation: the Fushimi AF Registry. Chest
2017;152:12661275.
88. Freeman JV, Simon DN, Go AS, Spertus J, Fonarow GC, Gersh BJ, Hylek EM,
Kowey PR, Mahaffey KW, Thomas LE, Chang P, Peterson ED, Piccini JP;
Outcomes Registry for Better Informed Treatment of Atrial Fibrillation
Investigators. Association between atrial fibrillation symptoms, quality of life, and
patient outcomes: results from the Outcomes Registry for Better Informed
Treatment of Atrial Fibrillation (ORBIT-AF). Circ Cardiovasc Qual Outcomes
2015;8:393402.
89. Frost L, Engholm G, Johnsen S, Moller H, Henneberg EW, Husted S. Incident
thromboembolism in the aorta and the renal, mesenteric, pelvic, and extremity
arteries after discharge from the hospital with a diagnosis of atrial fibrillation.
Arch Intern Med 2001;161:272276.
90. Gaita F, Corsinovi L, Anselmino M, Raimondo C, Pianelli M, Toso E, Bergamasco
L, Boffano C, Valentini MC, Cesarani F, Scaglione M. Prevalence of silent cerebral
ischemia in paroxysmal and persistent atrial fibrillation and correlation with cog-
nitive function. J Am Coll Cardiol 2013;62:19901997.
91. Garcia-Fernandez A, Roldan V, Rivera-Caravaca JM, Lip GYH, Marin F.
Applicability of the modified CHA2DS2-VASc score for stroke risk stratification
in Caucasian atrial fibrillation patients. Eur J Intern Med 2017;38:e21e22.
92. Gleason KT, Nazarian S, Dennison Himmelfarb CR. Atrial fibrillation symptoms
and sex, race, and psychological distress: a literature review. J Cardiovasc Nurs
2018;33:137143.
93. Gomez-Outes A, Lagunar-Ruiz J, Terleira-Fernandez AI, Calvo-Rojas G, Suarez-
Gea ML, Vargas-Castrillon E. Causes of death in anticoagulated patients with
atrial fibrillation. J Am Coll Cardiol 2016;68:25082521.
94. Graves KG, May HT, Jacobs V, Bair TL, Stevens SM, Woller SC, Crandall BG,
Cutler MJ, Day JD, Mallender C, Osborn JS, Peter Weiss J, Jared Bunch T. Atrial
fibrillation incrementally increases dementia risk across all CHADS2 and
ESC Guidelines 87

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
CHA2DS2VASc strata in patients receiving long-term warfarin. Am Heart J
2017;188:9398.
95. John RM, Michaud GF, Stevenson WG. Atrial fibrillation hospitalization, mortality,
and therapy. Eur Heart J 2018;39:39583960.
96. Kalantarian S, Ruskin JN. Atrial fibrillation and cognitive decline: phenomenon or
epiphenomenon?Cardiol Clin 2016;34:279285.
97. Kalantarian S, Stern TA, Mansour M, Ruskin JN. Cognitive impairment associated
with atrial fibrillation: a meta-analysis. Ann Intern Med 2013;158:33846.
98. Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incre-
mental health care costs in patients with atrial fibrillation in the United States.
Circ Cardiovasc Qual Outcomes 2011;4:313320.
99. Kirchhof P, Schmalowsky J, Pittrow D, Rosin L, Kirch W, Wegscheider K,
Meinertz T, ATRIUM Study Group. Management of patients with atrial fibrillation
by primary-care physicians in Germany: 1-year results of the ATRIUM registry.
Clin Cardiol 2014;37:277284.
100. Kochhauser S, Joza J, Essebag V, Proietti R, Koehler J, Tsang B, Wulffhart Z,
Pantano A, Khaykin Y, Ziegler PD, Verma A. The impact of duration of atrial
fibrillation recurrences on measures of health-related quality of life and symp-
toms. Pacing Clin Electrophysiol 2016;39:16672.
101. Konig S, Ueberham L, Schuler E, Wiedemann M, Reithmann C, Seyfarth M,
Sause A, Tebbenjohanns J, Schade A, Shin DI, Staudt A, Zacharzowsky U,
Andrie R, Wetzel U, Neuser H, Wunderlich C, Kuhlen R, Tijssen JGP, Hindricks
G, Bollmann A. In-hospital mortality of patients with atrial arrhythmias: insights
from the German-wide Helios hospital network of 161 502 patients and 34 025
arrhythmia-related procedures. Eur Heart J 2018;39:39473957.
102. Kotecha D, Lam CS, Van Veldhuisen DJ, Van Gelder IC, Voors AA, Rienstra M.
Heart failure with preserved ejection fraction and atrial fibrillation: vicious
twins. J Am Coll Cardiol 2016;68:22172228.
103. Kupper N, van den Broek K, Haagh E, van der Voort P, Widdershoven J,
Denollet J. Type D personality affects health-related quality of life in patients
with lone atrial fibrillation by increasing symptoms related to sympathetic acti-
vation. J Psychosom Res 2018;115:4452.
104. Kwok CS, Loke YK, Hale R, Potter JF, Myint PK. Atrial fibrillation and
incidence of dementia: a systematic review and meta-analysis. Neurology
2011;76:914922.
105. Levy S, Maarek M, Coumel P, Guize L, Lekieffre J, Medvedowsky JL, Sebaoun A.
Characterization of different subsets of atrial fibrillation in general practice in
France: the ALFA study. The College of French Cardiologists. Circulation
1999;99:30283035.
106. Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, D’Agostino
RB. Stroke severity in atrial fibrillation. The Framingham Study. Stroke
1996;27:17601764.
107. Lip GY, Laroche C, Boriani G, Cimaglia P, Dan GA, Santini M, Kalarus Z,
Rasmussen LH, Popescu MI, Tica O, Hellum CF, Mortensen B, Tavazzi L,
Maggioni AP. Sex-related differences in presentation, treatment, and outcome
of patients with atrial fibrillation in Europe: a report from the Euro
Observational Research Programme Pilot Survey on Atrial Fibrillation. Europace
2015;17:2431.
108. McCabe PJ, Rhudy LM, DeVon HA. Patients’ experiences from symptom onset
to initial treatment for atrial fibrillation. J Clin Nurs 2015;24:786796.
109. McCabe PJ, Schumacher K, Barnason SA. Living with atrial fibrillation: a qualita-
tive study. J Cardiovasc Nurs 2011;26:336344.
110. Meyre P, Blum S, Berger S, Aeschbacher S, Schoepfer H, Briel M, Osswald S,
Conen D. Risk of hospital admissions in patients with atrial fibrillation: a system-
atic review and meta-analysis. Can J Cardiol 2019;35:13321343.
111. Nieuwlaat R, Capucci A, Camm AJ, Olsson SB, Andresen D, Davies DW,
Cobbe S, Breithardt G, Le Heuzey JY, Prins MH, Levy S, Crijns HJ; European
Heart Survey Investigators. Atrial fibrillation management: a prospective survey
in ESC member countries: the Euro Heart Survey on Atrial Fibrillation. Eur
Heart J 2005;26:24222434.
112. Overvad TF, Nielsen PB, Lip GY. Treatment thresholds for stroke prevention
in atrial fibrillation: observations on the CHA2DS2-VASc score. Eur Heart J
Cardiovasc Pharmacother 2017;3:3741.
113. Page RL, Wilkinson WE, Clair WK, McCarthy EA, Pritchett EL. Asymptomatic
arrhythmias in patients with symptomatic paroxysmal atrial fibrillation and par-
oxysmal supraventricular tachycardia. Circulation 1994;89:224227.
114. Piccini JP, Fauchier L. Rhythm control in atrial fibrillation. Lancet
2016;388:829840.
115. Pistoia F, Sacco S, Tiseo C, Degan D, Ornello R, Carolei A. The epidemiology
of atrial fibrillation and stroke. Cardiol Clin 2016;34:255268.
116. Pokorney SD, Piccini JP, Stevens SR, Patel MR, Pieper KS, Halperin JL,
Breithardt G, Singer DE, Hankey GJ, Hacke W, Becker RC, Berkowitz SD,
Nessel CC, Mahaffey KW, Fox KA, Califf RM; ROCKET AF Steering
Committee Investigators. Cause of death and predictors of all-cause mortality
in anticoagulated patients with nonvalvular atrial fibrillation: data from ROCKET
AF. J Am Heart Assoc 2016;5:e002197.
117. Potpara TS, Polovina MM, Marinkovic JM, Lip GY. A comparison of clinical char-
acteristics and long-term prognosis in asymptomatic and symptomatic patients
with first-diagnosed atrial fibrillation: the Belgrade Atrial Fibrillation Study. Int J
Cardiol 2013;168:47444749.
118. Randolph TC, Simon DN, Thomas L, Allen LA, Fonarow GC, Gersh BJ, Kowey
PR, Reiffel JA, Naccarelli GV, Chan PS, Spertus JA, Peterson ED, Piccini JP;
ORBIT AF Investigators. Patient factors associated with quality of life in atrial
fibrillation. Am Heart J 2016;182:135143.
119. Rienstra M, Lubitz SA, Mahida S, Magnani JW, Fontes JD, Sinner MF, Van Gelder
IC, Ellinor PT, Benjamin EJ. Symptoms and functional status of patients with
atrial fibrillation: state-of-the-art and future research opportunities. Circulation
2012;125:29332943.
120. Rienstra M, Vermond RA, Crijns HJ, Tijssen JG, Van Gelder IC; RACE
Investigators. Asymptomatic persistent atrial fibrillation and outcome: results of
the RACE study. Heart Rhythm 2014;11:939945.
121. Rivard L, Khairy P. Mechanisms, clinical significance, and prevention of cogni-
tive impairment in patients with atrial fibrillation. Can J Cardiol
2017;33:15561564.
122. Santangeli P, Di Biase L, Bai R, Mohanty S, Pump A, Cereceda Brantes M,
Horton R, Burkhardt JD, Lakkireddy D, Reddy YM, Casella M, Dello Russo A,
Tondo C, Natale A. Atrial fibrillation and the risk of incident dementia: a meta-
analysis. Heart Rhythm 2012;9:1761 1768.
123. Schnabel RB, Michal M, Wilde S, Wiltink J, Wild PS, Sinning CR, Lubos E, Ojeda
FM, Zeller T, Munzel T, Blankenberg S, Beutel ME. Depression in atrial fibrilla-
tion in the general population. PLoS One 2013;8:e79109.
124. Schnabel RB, Pecen L, Ojeda FM, Lucerna M, Rzayeva N, Blankenberg S, Darius
H, Kotecha D, Caterina R, Kirchhof P. Gender differences in clinical presenta-
tion and 1-year outcomes in atrial fibrillation. Heart 2017;103:10241030.
125. Senoo K, Suzuki S, Sagara K, Otsuka T, Matsuno S, Funada R, Uejima T, Oikawa
Y, Yajima J, Koike A, Nagashima K, Kirigaya H, Sawada H, Aizawa T, Yamashita
T. Distribution of first-detected atrial fibrillation patients without structural
heart diseases in symptom classifications. Circ J 2012;76:10201023.
126. Serpytis R, Navickaite A, Serpytiene E, Barysiene J, Marinskis G, Jatuzis D,
Petrulioniene Z, Laucevicius A, Serpytis P. Impact of atrial fibrillation on cogni-
tive function, psychological distress, quality of life, and impulsiveness. Am J Med
2018;131:703.e1-703e5.
127. Siontis KC, Gersh BJ, Killian JM, Noseworthy PA, McCabe P, Weston SA, Roger
VL, Chamberlain AM. Typical, atypical, and asymptomatic presentations of new-
onset atrial fibrillation in the community: characteristics and prognostic implica-
tions. Heart Rhythm 2016;13:14181424.
128. Steg PG, Alam S, Chiang CE, Gamra H, Goethals M, Inoue H, Krapf L, Lewalter
T, Merioua I, Murin J, Naditch-Brule L, Ponikowski P, Rosenqvist M, Silva-
Cardoso J, Zharinov O, Brette S, Neill JO; RealiseAF investigators. Symptoms,
functional status and quality of life in patients with controlled and uncontrolled
atrial fibrillation: data from the RealiseAF cross-sectional international registry.
Heart 2012;98:195201.
129. Steinberg BA, Kim S, Fonarow GC, Thomas L, Ansell J, Kowey PR, Mahaffey
KW, Gersh BJ, Hylek E, Naccarelli G, Go AS, Reiffel J, Chang P, Peterson ED,
Piccini JP. Drivers of hospitalization for patients with atrial fibrillation: results
from the Outcomes Registry for Better Informed Treatment of Atrial
Fibrillation (ORBIT-AF). Am Heart J 2014;167:735742.e2.
130. Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the
long-term risks associated with atrial fibrillation: 20-year follow-up of the
Renfrew/Paisley study. Am J Med 2002;
113:359364.
131. Streur M, Ratcliffe SJ, Ball J, Stewart S, Riegel B. Symptom clusters in adults with
chronic atrial fibrillation. J Cardiovasc Nurs 2017;32:296303.
132. Thrall G, Lip GY, Carroll D, Lane D. Depression, anxiety, and quality of life in
patients with atrial fibrillation. Chest 2007;132:12591264.
133. Ugowe FE, Jackson LRn. Atrial fibrillation and mortality risk: seeing the big pic-
ture. Eur Heart J Qual Care Clin Outcomes 2019;5:67.
134. Vermond RA, Crijns HJ, Tijssen JG, Alings AM, Van den Berg MP, Hillege HL,
Van Veldhuisen DJ, Van Gelder IC, Rienstra M; RACE II investigators. Symptom
severity is associated with cardiovascular outcome in patients with permanent
atrial fibrillation in the RACE II study. Europace 2014;16:14171425.
135. Walters TE, Wick K, Tan G, Mearns M, Joseph SA, Morton JB, Sanders P,
Bryant C, Kistler PM, Kalman JM. Psychological distress and suicidal ideation in
patients with atrial fibrillation: prevalence and response to management strat-
egy. J Am Heart Assoc 2018;7:e005502.
136. Walters TE, Wick K, Tan G, Mearns M, Joseph SA, Morton JB, Sanders P,
Bryant C, Kistler PM, Kalman JM. Symptom severity and quality of life in patients
with atrial fibrillation: psychological function outweighs clinical predictors. Int J
Cardiol 2019;279:8489.
137. Wang TJ, Massaro JM, Levy D, Vasan RS, Wolf PA, D’Agostino RB, Larson MG,
Kannel WB, Benjamin EJ. A risk score for predicting stroke or death in individu-
als with new-onset atrial fibrillation in the community: the Framingham Heart
Study. JAMA 2003;290:10491056.
88 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
138. Wijesurendra RS, Casadei B. Atrial fibrillation: effects beyond the
atrium?Cardiovasc Res 2015;105:238247.
139. Xiong Q, Proietti M, Senoo K, Lip GY. Asymptomatic versus symptomatic atrial
fibrillation: a systematic review of age/gender differences and cardiovascular
outcomes. Int J Cardiol 2015;191:172177.
140. Ziff OJ, Carter PR, McGowan J, Uppal H, Chandran S, Russell S, Bainey KR,
Potluri R. The interplay between atrial fibrillation and heart failure on long-term
mortality and length of stay: insights from the United Kingdom ACALM registry.
Int J Cardiol 2018;252:117121.
141. Sepehri Shamloo A, Dagres N, Mussigbrodt A, Stauber A, Kircher S, Richter S,
Dinov B, Bertagnolli L, Husser-Bollmann D, Bollmann A, Hindricks G, Arya A.
Atrial fibrillation and cognitive impairment: new insights and future directions.
Heart Lung Circ 2020;29:6985.
142. Conen D, Rodondi N, Muller A, Beer JH, Ammann P, Moschovitis G, Auricchio
A, Hayoz D, Kobza R, Shah D, Novak J, Schlapfer J, Di Valentino M,
Aeschbacher S, Blum S, Meyre P, Sticherling C, Bonati LH, Ehret G, Moutzouri
E, Fischer U, Monsch AU, Stippich C, Wuerfel J, Sinnecker T, Coslovsky M,
Schwenkglenks M, Kuhne M, Osswald S, Swiss AFSI. Relationships of overt and
silent brain lesions with cognitive function in patients with atrial fibrillation. JAm
Coll Cardiol 2019;73:989999.
143. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M,
Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J,
Popescu BA, Schotten U, Van Putte B, Vardas P, ESC Scientific Document
Group. 2016 ESC Guidelines for the management of atrial fibrillation developed
in collaboration with EACTS. Eur Heart J 2016;37:28932962.
144. Boriani G, Diemberger I, Ziacchi M, Valzania C, Gardini B, Cimaglia P,
Martignani C, Biffi M. AF burden is important fact or fiction?Int J Clin Pract
2014;68:444452.
145. Boriani G, Pettorelli D. Atrial fibrillation burden and atrial fibrillation type: clini-
cal significance and impact on the risk of stroke and decision making for long-
term anticoagulation. Vascul Pharmacol 2016;83:2635.
146. Charitos EI, Purerfellner H, Glotzer TV, Ziegler PD. Clinical classifications of
atrial fibrillation poorly reflect its temporal persistence: insights from 1,195
patients continuously monitored with implantable devices. J Am Coll Cardiol
2014;63:28402848.
147. Wyse DG, Van Gelder IC, Ellinor PT, Go AS, Kalman JM, Narayan SM, Nattel S,
Schotten U, Rienstra M. Lone atrial fibrillation: does it exist?J Am Coll Cardiol
2014;63:17151723.
148. Lip GYH, Collet JP, Caterina R, Fauchier L, Lane DA, Larsen TB, Marin F,
Morais J, Narasimhan C, Olshansky B, Pierard L, Potpara T, Sarrafzadegan N,
Sliwa K, Varela G, Vilahur G, Weiss T, Boriani G, Rocca B, ESC Scientific
Document Group. Antithrombotic therapy in atrial fibrillation associated with
valvular heart disease: a joint consensus document from the European Heart
Rhythm Association (EHRA) and European Society of Cardiology Working
Group on Thrombosis, endorsed by the ESC Working Group on Valvular
Heart Disease, Cardiac Arrhythmia Society of Southern Africa (CASSA), Heart
Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), South
African Heart (SA Heart) Association and Sociedad Latinoamericana de
Estimulacion Cardiaca y Electrofisiologia (SOLEACE). Europace
2017;19:17571758.
149. January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC, Jr., Ellinor
PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB,
Tracy CM, Yancy CW. 2019 AHA/ACC/HRS focused update of the 2014 AHA/
ACC/HRS Guideline for the management of patients with atrial fibrillation.
Circulation
2019;;140:e125e151.
150. NHFA CSANZ Atrial Fibrillation Guideline Working Group, Brieger D,
Amerena J, Attia J, Bajorek B, Chan KH, Connell C, Freedman B, Ferguson C,
Hall T, Haqqani H, Hendriks J, Hespe C, Hung J, Kalman JM, Sanders P,
Worthington J, Yan TD, Zwar N. National Heart Foundation of Australia and
the Cardiac Society of Australia and New Zealand: Australian Clinical
Guidelines for the diagnosis and management of atrial fibrillation 2018. Heart
Lung Circ 2018;27:12091266.
151. Potpara TS, Lip GYH, Blomstrom-Lundqvist C, Boriani G, Van Gelder IC,
Heidbuchel H, Hindricks G, Camm AJ. The 4S-AF scheme (Stroke Risk;
Symptoms; Severity of Burden; Substrate): A novel approach to in-depth char-
acterization (rather than Classification) of atrial fibrillation. Thromb Haemost
2020; doi: 10.1055/s-0040-1716408.
152. Chen LY, Chung MK, Allen LA, Ezekowitz M, Furie KL, McCabe P,
Noseworthy PA, Perez MV, Turakhia MP,American Heart Association
CouncilonClinicalCardiology,CouncilonCardiovascularandStroke
Nursing, Council on Quality of Care and Outcomes Research, and Stroke
Council. Atrial fibrillation burden: moving beyond atrial fibrillation as a binary
entity: a scientific statement from the American Heart Association. Circulation
2018;137:e623e644.
153. Ziegler PD, Koehler JL, Mehra R. Comparison of continuous versus intermittent
monitoring of atrial arrhythmias. Heart Rhythm 2006;3:14451452.
154. Boriani G, Proietti M, Laroche C, Fauchier L, Marin F, Nabauer M, Potpara T,
Dan GA, Kalarus Z, Diemberger I, Tavazzi L, Maggioni AP, Lip GYH; EORP-AF
Long-Term General Registry Investigators Steering Committee (National
Coordinators). Contemporary stroke prevention strategies in 11 096 European
patients with atrial fibrillation: a report from the EURObservational Research
Programme on Atrial Fibrillation (EORP-AF) long-term general registry.
Europace 2018;20:747757.
155. Pandey A, Kim S, Moore C, Thomas L, Gersh B, Allen LA, Kowey PR, Mahaffey
KW, Hylek E, Peterson ED, Piccini JP, Fonarow GC; ORBIT-AF Investigators
and Patients. Predictors and prognostic implications of incident heart failure in
patients with prevalent atrial fibrillation. JACC Heart Fail 2017;5:4452.
156. Ganesan AN, Chew DP, Hartshorne T, Selvanayagam JB, Aylward PE, Sanders
P, McGavigan AD. The impact of atrial fibrillation type on the risk of throm-
boembolism, mortality, and bleeding: a systematic review and meta-analysis. Eur
Heart J 2016;37:15911602.
157. Al-Khatib SM, Thomas L, Wallentin L, Lopes RD, Gersh B, Garcia D, Ezekowitz
J, Alings M, Yang H, Alexander JH, Flaker G, Hanna M, Granger CB. Outcomes
of apixaban vs. warfarin by type and duration of atrial fibrillation: results from
the ARISTOTLE trial. Eur Heart J 2013;34:24642471.
158. Link MS, Giugliano RP, Ruff CT, Scirica BM, Huikuri H, Oto A, Crompton AE,
Murphy SA, Lanz H, Mercuri MF, Antman EM, Braunwald E; ENGAGE AF-TIMI
48 Investigators. Stroke and mortality risk in patients with various patterns of
atrial fibrillation: results from the ENGAGE AF-TIMI 48 Trial (Effective
Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation-
Thrombolysis in Myocardial Infarction 48). Circ Arrhythm Electrophysiol
2017;10:e004267.
159. Steinberg BA, Hellkamp AS, Lokhnygina Y, Patel MR, Breithardt G, Hankey GJ,
Becker RC, Singer DE, Halperin JL, Hacke W, Nessel CC, Berkowitz SD,
Mahaffey KW, Fox KA, Califf RM, Piccini JP; ROCKET-AF Steering Committee
and Investigators. Higher risk of death and stroke in patients with persistent vs.
paroxysmal atrial fibrillation: results from the ROCKET-AF Trial. Eur Heart J
2015;36:288296.
160. Hart RG, Pearce LA, Rothbart RM, McAnulty JH, Asinger RW, Halperin JL.
Stroke with intermittent atrial fibrillation: incidence and predictors during
aspirin therapy. Stroke Prevention in Atrial Fibrillation Investigators. J Am Coll
Cardiol 2000;35:183
187.
161. Takabayashi K, Hamatani Y, Yamashita Y, Takagi D, Unoki T, Ishii M, Iguchi M,
Masunaga N, Ogawa H, Esato M, Chun YH, Tsuji H, Wada H, Hasegawa K, Abe
M, Lip GY, Akao M. Incidence of stroke or systemic embolism in paroxysmal
versus sustained atrial fibrillation: the Fushimi Atrial Fibrillation Registry. Stroke
2015;46:33543361.
162. Nieuwlaat R, Dinh T, Olsson SB, Camm AJ, Capucci A, Tieleman RG, Lip GY,
Crijns HJ; Euro Heart Survey Investigators. Should we abandon the common
practice of withholding oral anticoagulation in paroxysmal atrial fibrillation?Eur
Heart J 2008;29:915922.
163. Go AS, Reynolds K, Yang J, Gupta N, Lenane J, Sung SH, Harrison TN, Liu TI,
Solomon MD. Association of burden of atrial fibrillation with risk of ischemic
stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM Study.
JAMA Cardiol 2018;3:601608.
164. Ecker V, Knoery C, Rushworth G, Rudd I, Ortner A, Begley D, Leslie SJ. A
review of factors associated with maintenance of sinus rhythm after elective
electrical cardioversion for atrial fibrillation. Clin Cardiol 2018;41:862870.
165. Nyong J, Amit G, Adler AJ, Owolabi OO, Perel P, Prieto-Merino D, Lambiase P,
Casas JP, Morillo CA. Efficacy and safety of ablation for people with non-
paroxysmal atrial fibrillation. Cochrane Database Syst Rev 2016;11:CD012088.
166. Piccini JP, Passman R, Turakhia M, Connolly AT, Nabutovsky Y, Varma N. Atrial
fibrillation burden, progression, and the risk of death: a case-crossover analysis
in patients with cardiac implantable electronic devices. Europace
2019;21:404413.
167. Deng H, Bai Y, Shantsila A, Fauchier L, Potpara TS, Lip GYH. Clinical scores for
outcomes of rhythm control or arrhythmia progression in patients with atrial
fibrillation: a systematic review. Clin Res Cardiol 2017;106:813823.
168. Healey JS, Connolly SJ, Gold MR, Israel CW, Van Gelder IC, Capucci A, Lau
CP, Fain E, Yang S, Bailleul C, Morillo CA, Carlson M, Themeles E, Kaufman ES,
Hohnloser SH; ASSERT Investigators. Subclinical atrial fibrillation and the risk of
stroke. N Engl J Med 2012;366:120129.
169. Potpara TS, Stankovic GR, Beleslin BD, Polovina MM, Marinkovic JM, Ostojic
MC, Lip GYH. A 12-year follow-up study of patients with newly diagnosed lone
atrial fibrillation: implications of arrhythmia progression on prognosis: the
Belgrade Atrial Fibrillation Study. Chest 2012;141:339347.
170. Goette A, Kalman JM, Aguinaga L, Akar J, Cabrera JA, Chen SA, Chugh SS,
Corradi D, D’Avila A, Dobrev D, Fenelon G, Gonzalez M, Hatem SN, Helm R,
Hindricks G, Ho SY, Hoit B, Jalife J, Kim YH, Lip GY, Ma CS, Marcus GM,
Murray K, Nogami A, Sanders P, Uribe W, Van Wagoner DR, Nattel S. EHRA/
HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition,
characterization, and clinical implication. Europace 2016;18:14551490.
ESC Guidelines 89

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
171. Nattel S, Guasch E, Savelieva I, Cosio FG, Valverde I, Halperin JL, Conroy JM,
Al-Khatib SM, Hess PL, Kirchhof P, De Bono J, Lip GY, Banerjee A, Ruskin J,
Blendea D, Camm AJ. Early management of atrial fibrillation to prevent cardio-
vascular complications. Eur Heart J 2014;35:14481456.
172. Freedman B, Camm J, Calkins H, Healey JS, Rosenqvist M, Wang J, Albert CM,
Anderson CS, Antoniou S, Benjamin EJ, Boriani G, Brachmann J, Brandes A,
Chao TF, Conen D, Engdahl J, Fauchier L, Fitzmaurice DA, Friberg L, Gersh BJ,
Gladstone DJ, Glotzer TV, Gwynne K, Hankey GJ, Harbison J, Hillis GS, Hills
MT, Kamel H, Kirchhof P, Kowey PR, Krieger D, Lee VWY, Levin LA, Lip GYH,
Lobban T, Lowres N, Mairesse GH, Martinez C, Neubeck L, Orchard J, Piccini
JP, Poppe K, Potpara TS, Puererfellner H, Rienstra M, Sandhu RK, Schnabel RB,
Siu CW, Steinhubl S, Svendsen JH, Svennberg E, Themistoclakis S, Tieleman
RG, Turakhia MP, Tveit A, Uittenbogaart SB, Van Gelder IC, Verma A, Wachter
R, Yan BP, SCREEN CollaboratorsAF-. Screening for atrial fibrillation: a report
of the AF-SCREEN International Collaboration. Circulation
2017;135:18511867.
173. Mairesse GH, Moran P, Van Gelder IC, Elsner C, Rosenqvist M, Mant J, Banerjee A,
GorenekB,BrachmannJ,VarmaN,GlotzdeLimaG,KalmanJ,ClaesN,LobbanT,
Lane D, Lip GYH, Boriani G, ESC Scientific Document Group. Screening for atrial
fibrillation: a European Heart Rhythm Association (EHRA) consensus document
endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society
(APHRS), and Sociedad Latinoamericana de Estimulacion Cardiaca y
Electrofisiologia (SOLAECE). Europace 2017;19:15891623.
174. Padfield GJ, Steinberg C, Swampillai J, Qian H, Connolly SJ, Dorian P, Green
MS, Humphries KH, Klein GJ, Sheldon R, Talajic M, Kerr CR. Progression of par-
oxysmal to persistent atrial fibrillation: 10-year follow-up in the Canadian
Registry of Atrial Fibrillation. Heart Rhythm 2017;14:801807.
175. Vidal-Perez R, Otero-Ravina F, Lado-Lopez M, Turrado-Turrado V, Rodriguez-
Moldes E, Gomez-Vazquez JL, de Frutos-de Marcos C, de Blas-Abad P, Besada-
Gesto R, Gonzalez-Juanatey JR; BARBANZA Investigators. The change in the
atrial fibrillation type as a prognosis marker in a community study: long-term
data from AFBAR (Atrial Fibrillation in the BARbanza) study. Int J Cardiol
2013;168:21462152.
176. de Vos CB, Pisters R, Nieuwlaat R, Prins MH, Tieleman RG, Coelen RJ, van den
Heijkant AC, Allessie MA, Crijns HJ. Progression from paroxysmal to persistent
atrial fibrillation clinical correlates and prognosis. J Am Coll Cardiol
2010;55:725731.
177. Hobbelt AH, Spronk HM, Crijns H, Ten Cate H, Rienstra M, Van Gelder IC.
Prethrombotic state in young very low-risk patients with atrial fibrillation. JAm
Coll Cardiol 2017;69:19901992.
178. Habibi M, Samiei S, Ambale Venkatesh B, Opdahl A, Helle-Valle TM, Zareian M,
Almeida AL, Choi EY, Wu C, Alonso A, Heckbert SR, Bluemke DA, Lima JA.
Cardiac magnetic resonance-measured left atrial volume and function and inci-
dent atrial fibrillation: results from MESA (Multi-Ethnic Study of
Atherosclerosis). Circ Cardiovasc Imaging 2016;9:e004299.
179. Brambatti M, Connolly SJ, Gold MR, Morillo CA, Capucci A, Muto C, Lau CP,
Van Gelder IC, Hohnloser SH, Carlson M, Fain E, Nakamya J, Mairesse GH,
Halytska M, Deng WQ, Israel CW, Healey JS; ASSERT Investigators. Temporal
relationship between subclinical atrial fibrillation and embolic events. Circulation
2014;129:20942099.
180. Guichard JB, Nattel S. Atrial Cardiomyopathy: A useful notion in cardiac disease
management or a passing fad?J Am Coll Cardiol 2017;70:756765.
181. Hirsh BJ, Copeland-Halperin RS, Halperin JL. Fibrotic atrial cardiomyopathy,
atrial fibrillation, and thromboembolism: mechanistic links and clinical infer-
ences. J Am Coll Cardiol 2015;65:22392251.
182. Freedman B, Potpara TS, Lip GY. Stroke prevention in atrial fibrillation. Lancet
2016;388:806
817.
183. Martinez C, Katholing A, Freedman SB. Adverse prognosis of incidentally
detected ambulatory atrial fibrillation. A cohort study. Thromb Haemost
2014;112:276286.
184. Wilson JM, Jungner YG. [Principles and practice of mass screening for disease].
Bol Oficina Sanit Panam 1968;65:281393.
185. Welton NJ, McAleenan A, Thom HH, Davies P, Hollingworth W, Higgins JP,
Okoli G, Sterne JA, Feder G, Eaton D, Hingorani A, Fawsitt C, Lobban T,
Bryden P, Richards A, Sofat R. Screening strategies for atrial fibrillation: a sys-
tematic review and cost-effectiveness analysis. Health Technol Assess
2017;21:1236.
186. Steinhubl SR, Waalen J, Edwards AM, Ariniello LM, Mehta RR, Ebner GS,
Carter C, Baca-Motes K, Felicione E, Sarich T, Topol EJ. Effect of a home-based
wearable continuous ECG monitoring patch on detection of undiagnosed atrial
fibrillation: the mSToPS randomized clinical trial. JAMA 2018;320:146155.
187. Schnabel RB, Haeusler KG, Healey JS, Freedman B, Boriani G, Brachmann J,
Brandes A, Bustamante A, Casadei B, Crijns H, Doehner W, Engstrom G,
Fauchier L, Friberg L, Gladstone DJ, Glotzer TV, Goto S, Hankey GJ, Harbison
JA, Hobbs FDR, Johnson LSB, Kamel H, Kirchhof P, Korompoki E, Krieger DW,
Lip GYH, Lochen ML, Mairesse GH, Montaner J, Neubeck L, Ntaios G, Piccini
JP, Potpara TS, Quinn TJ, Reiffel JA, Ribeiro ALP, Rienstra M, Rosenqvist M,
Sakis T, Sinner MF, Svendsen JH, Van Gelder IC, Wachter R, Wijeratne T, Yan
B. Searching for atrial fibrillation poststroke: a white paper of the AF-SCREEN
International Collaboration. Circulation 2019;140:18341850.
188. Yan BP, Lai WHS, Chan CKY, Chan SC, Chan LH, Lam KM, Lau HW, Ng CM,
Tai LY, Yip KW, To OTL, Freedman B, Poh YC, Poh MZ. Contact-free screen-
ing of atrial fibrillation by a smartphone using facial pulsatile photoplethysmo-
graphic signals. J Am Heart Assoc 2018;7.
189. Orchard J, Lowres N, Freedman SB, Ladak L, Lee W, Zwar N, Peiris D,
Kamaladasa Y, Li J, Neubeck L. Screening for atrial fibrillation during influenza
vaccinations by primary care nurses using a smartphone electrocardiograph
(iECG): a feasibility study. Eur J Prev Cardiol 2016;23:1320.
190. Lampert R. Screening for atrial fibrillation using smartphone-based technology
and layperson volunteers: high-tech meets community participatory research
for the best of both worlds. Heart Rhythm 2018;15:13121313.
191. Lahdenoja O, Hurnanen T, Iftikhar Z, Nieminen S, Knuutila T, Saraste A,
Kiviniemi T, Vasankari T, Airaksinen J, Pankaala M, Koivisto T. Atrial fibrillation
detection via accelerometer and gyroscope of a smartphone. IEEE J Biomed
Health Inform 2018;22:108118.
192. Freedman B. Screening for atrial fibrillation using a smartphone: is there an app
for that?J Am Heart Assoc 2016;5.
193. Chan NY, Choy CC. Screening for atrial fibrillation in 13 122 Hong Kong citi-
zens with smartphone electrocardiogram. Heart 2017;103:2431.
194. Chan PH, Wong CK, Poh YC, Pun L, Leung WW, Wong YF, Wong MM, Poh
MZ, Chu DW, Siu CW. Diagnostic performance of a smartphone-based photo-
plethysmographic application for atrial fibrillation screening in a primary care
setting. J Am Heart Assoc 2016;5.
195. Brasier N, Raichle CJ, Dorr M, Becke A, Nohturfft V, Weber S, Bulacher F,
Salomon L, Noah T, Birkemeyer R, Eckstein J. Detection of atrial fibrillation
with a smartphone camera: first prospective, international, two-centre, clinical
validation study (DETECT AF PRO). Europace 2019;21:4147.
196. Tison GH, Sanchez JM, Ballinger B, Singh A, Olgin JE, Pletcher MJ, Vittinghoff E,
Lee ES, Fan SM, Gladstone RA, Mikell C, Sohoni N, Hsieh J, Marcus GM. Passive
detection of atrial fibrillation using a commercially available smartwatch. JAMA
Cardiol 2018;3:409416.
197. Li KHC, White FA, Tipoe T, Liu T, Wong MC, Jesuthasan A, Baranchuk A, Tse
G, Yan BP. The current state of mobile phone apps for monitoring heart rate,
heart rate variability, and atrial fibrillation: narrative review. JMIR Mhealth
Uhealth 2019;7:e11606.
198. Bumgarner JM, Lambert CT, Hussein AA, Cantillon DJ, Baranowski B, Wolski K,
Lindsay BD, Wazni OM, Tarakji KG. Smartwatch algorithm for automated
detection of atrial fibrillation. J Am Coll Cardiol 2018;71:23812388.
199. Wasserlauf J, You C, Patel R, Valys A, Albert D, Passman R. Smartwatch per-
formance for the detection and quantification of atrial fibrillation. Circ Arrhythm
Electrophysiol 2019;12:e006834.
200. Attia ZI, Noseworthy PA, Lopez-Jimenez F, Asirvatham SJ, Deshmukh AJ, Gersh
BJ, Carter RE, Yao X, Rabinstein AA, Erickson BJ, Kapa S, Friedman PA.
Anartificial intelligence-enabled ECG algorithm for the identification of patients
with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome
prediction. Lancet 2019;394:861867.
201. Turakhia MP, Desai M, Hedlin H, Rajmane A, Talati N, Ferris T, Desai S, Nag D,
Patel M, Kowey P, Rumsfeld JS, Russo AM, Hills MT, Granger CB, Mahaffey
KW, Perez MV. Rationale and design of a large-scale, app-based study to iden-
tify cardiac arrhythmias using a smartwatch: the Apple Heart Study. Am Heart J
2019;207:6675.
202. Guo Y, Wang H, Zhang H, Liu T, Liang Z, Xia Y, Yan L, Xing Y, Shi H, Li S, Liu
Y, Liu F, Feng M, Chen Y, Lip GYH; MAFA II Investigators. Mobile photoplethys-
mographic technology to detect atrial fibrillation. J Am Coll Cardiol
2019;74:23652375.
203. Harris K, Edwards D, Mant J. How can we best detect atrial fibrillation?J R Coll
Physicians Edinb 2012;42 Suppl 18:522.
204. Wiesel J, Wiesel D, Suri R, Messineo FC. The use of a modified sphygmoman-
ometer to detect atrial fibrillation in outpatients. Pacing Clin Electrophysiol
2004;27:639643.
205. Wiesel J, Fitzig L, Herschman Y, Messineo FC. Detection of atrial fibrillation
using a modified microlife blood pressure monitor. Am J Hypertens
2009;22:848852.
206. Stergiou GS, Karpettas N, Protogerou A, Nasothimiou EG, Kyriakidis M.
Diagnostic accuracy of a home blood pressure monitor to detect atrial fibrilla-
tion. J Hum Hypertens 2009;23:654658.
207. Willits I, Keltie K, Craig J, Sims A. WatchBP Home A for opportunistically
detecting atrial fibrillation during diagnosis and monitoring of hypertension:
a
NICE Medical Technology Guidance. Appl Health Econ Health Policy
2014;12:255265.
208. Desteghe L, Raymaekers Z, Lutin M, Vijgen J, Dilling-Boer D, Koopman P,
Schurmans J, Vanduynhoven P, Dendale P, Heidbuchel H. Performance of
90 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
handheld electrocardiogram devices to detect atrial fibrillation in a cardiology
and geriatric ward setting. Europace 2017;19:2939.
209. Kaasenbrood F, Hollander M, Rutten FH, Gerhards LJ, Hoes AW, Tieleman RG.
Yield of screening for atrial fibrillation in primary care with a hand-held, single-
lead electrocardiogram device during influenza vaccination. Europace
2016;18:15141520.
210. Wiesel J, Abraham S, Messineo FC. Screening for asymptomatic atrial
fibrillation while monitoring the blood pressure at home: trial of regular versus
irregular pulse for prevention of stroke (TRIPPS 2.0). Am J Cardiol
2013;111:15981601.
211. Jacobs MS, Kaasenbrood F, Postma MJ, van Hulst M, Tieleman RG. Cost-effec-
tiveness of screening for atrial fibrillation in primary care with a handheld,
single-lead electrocardiogram device in the Netherlands. Europace
2018;20:1218.
212. Lowres N, Neubeck L, Salkeld G, Krass I, McLachlan AJ, Redfern J, Bennett AA,
Briffa T, Bauman A, Martinez C, Wallenhorst C, Lau JK, Brieger DB, Sy RW,
Freedman SB. Feasibility and cost-effectiveness of stroke prevention through
community screening for atrial fibrillation using iPhone ECG in pharmacies. The
SEARCH-AF study. Thromb Haemost 2014;111:11671176.
213. William AD, Kanbour M, Callahan T, Bhargava M, Varma N, Rickard J,
Saliba W, Wolski K, Hussein A, Lindsay BD, Wazni OM, Tarakji KG.
Assessing the accuracy of an automated atrial fibrillation detection algo-
rithm using smartphone technology: the iREAD Study. Heart Rhythm
2018;15:15611565.
214. Nemati S, Ghassemi MM, Ambai V, Isakadze N, Levantsevych O, Shah A,
Clifford GD. Monitoring and detecting atrial fibrillation using wearable technol-
ogy. Conf Proc IEEE Eng Med Biol Soc 2016;2016:33943397.
215. Petryszyn P, Niewinski P, Staniak A, Piotrowski P, Well A, Well M, Jeskowiak I,
Lip G, Ponikowski P. Effectiveness of screening for atrial fibrillation and its
determinants. A meta-analysis. PLoS One 2019;14:e0213198.
216. Orchard J, Lowres N, Neubeck L, Freedman B. Atrial fibrillation: is there
enough evidence to recommend opportunistic or systematic screening?Int J
Epidemiol 2018;47:1361.
217. Svennberg E, Engdahl J, Al-Khalili F, Friberg L, Frykman V, Rosenqvist M. Mass
screening for untreated atrial fibrillation: the STROKESTOP Study. Circulation
2015;131:21762184.
218. Halcox JPJ, Wareham K, Cardew A, Gilmore M, Barry JP, Phillips C, Gravenor
MB. Assessment of remote heart rhythm sampling using the AliveCor heart
monitor to screen for atrial fibrillation: the REHEARSE-AF Study. Circulation
2017;136:17841794.
219. Turakhia MP, Shafrin J, Bognar K, Goldman DP, Mendys PM, Abdulsattar Y,
Wiederkehr D, Trocio J. Economic burden of undiagnosed nonvalvular atrial
fibrillation in the United States. Am J Cardiol 2015;116:733739.
220. Fay MR, Fitzmaurice DA, Freedman B. Screening of older patients for atrial
fibrillation in general practice: current evidence and its implications for future
practice. Eur J Gen Pract
2017;23:246253.
221. Boriani G, Valzania C, Biffi M, Diemberger I, Ziacchi M, Martignani C.
Asymptomatic lone atrial fibrillation how can we detect the arrhythmia?Curr
Pharm Des 2015;21:659666.
222. Hobbs FD, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, Raftery J,
Davies M, Lip G. A randomised controlled trial and cost-effectiveness study of
systematic screening (targeted and total population screening) versus routine
practice for the detection of atrial fibrillation in people aged 65 and over. The
SAFE study. Health Technol Assess 2005;9:iii-iv, ix-x, 174.
223. Aronsson M, Svennberg E, Rosenqvist M, Engdahl J, Al-Khalili F, Friberg L, Frykman-
Kull V, Levin LA. Cost-effectiveness of mass screening for untreated atrial fibrillation
using intermittent ECG recording. Europace 2015;17:10231029.
224. Lowres N, Neubeck L, Redfern J, Freedman SB. Screening to identify unknown
atrial fibrillation. A systematic review. Thromb Haemo st 2013;110:213222.
225. Engdahl J, Andersson L, Mirskaya M, Rosenqvist M. Stepwise screening of atrial
fibrillation in a 75-year-old population: implications for stroke prevention.
Circulation 2013;127:930937.
226. Boriani G, Glotzer TV, Santini M, West TM, De Melis M, Sepsi M, Gasparini M,
Lewalter T, Camm JA, Singer DE. Device-detected atrial fibrillation and risk for
stroke: an analysis of >10,000 patients from the SOS AF project (Stroke
preventiOn Strategies based on Atrial Fibrillation information from implanted
devices). Eur Heart J 2014;35:508516.
227. Lowres N, Krass I, Neubeck L, Redfern J, McLachlan AJ, Bennett AA, Freedman
SB. Atrial fibrillation screening in pharmacies using an iPhone ECG: a qualitative
review of implementation. Int J Clin Pharm 2015;37:11111120.
228. Wynn GJ, Todd DM, Webber M, Bonnett L, McShane J, Kirchhof P, Gupta D.
The European Heart Rhythm Association symptom classification for atrial fibril-
lation: validation and improvement through a simple modification. Europace
2014;16:965972.
229. De With RR, Rienstra M, Smit MD, Weijs B, Zwartkruis VW, Hobbelt AH,
Alings M, Tijssen JGP, Brugemann J, Geelhoed B, Hillege HL, Tukkie R, Hemels
ME, Tieleman RG, Ranchor AV, Van Veldhuisen DJ, Crijns H, Van Gelder IC.
Targeted therapy of underlying conditions improves quality of life in patients
with persistent atrial fibrillation: results of the RACE 3 study. Europace
2019;21:563571.
230. Schnabel RB, Pecen L, Rzayeva N, Lucerna M, Purmah Y, Ojeda FM, De
Caterina R, Kirchhof P. Symptom burden of atrial fibrillation and its relation to
interventions and outcome in Europe. J Am Heart Assoc 2018;7.
231. Bjo¨ rkenheim A, Brandes A, Magnuson A, Chemnitz A, Svedberg L, Edvardsson
N, Poc¸i D. Assessment of atrial fibrillation specific symptoms before and 2
years after atrial fibrillation ablation: do patients and physicians differ in their
perception of symptom relief?JACC: Clinical Electrophysiology 2017;
3:11681176.
232. Sandhu RK, Smigorowsky M, Lockwood E, Savu A, Kaul P, McAlister FA. Impact
of electrical cardioversion on quality of life for the treatment of atrial fibrilla-
tion. Can J Cardiol 2017;33:450455.
233. Singh BN, Singh SN, Reda DJ, Tang XC, Lopez B, Harris CL, Fletcher RD,
Sharma SC, Atwood JE, Jacobson AK, Lewis HD, Jr., Raisch DW, Ezekowitz
MD; Sotalol Amiodarone Atrial Fibrillation Efficacy Trial Investigators.
Amiodarone versus sotalol for atrial fibrillation. N Engl J Med
2005;352:18611872.
234. Gilbert KA, Hogarth AJ, MacDonald W, Lewis NT, Tan LB, Tayebjee MH.
Restoration of sinus rhythm results in early and late improvements in the func-
tional reserve of the heart following direct current cardioversion of persistent
AF: FRESH-AF. Int J Cardiol 2015;199:121125.
235. Jais P, Cauchemez B, Macle L, Daoud E, Khairy P, Subbiah R, Hocini M,
Extramiana F, Sacher F, Bordachar P, Klein G, Weerasooriya R, Clementy J,
Haissaguerre M. Catheter ablation versus antiarrhythmic drugs for atrial fibrilla-
tion: the A4 study. Circulation 2008;118:24982505.
236. Oral H, Pappone C, Chugh A, Good E, Bogun F, Pelosi F, Jr., Bates ER,
Lehmann MH, Vicedomini G, Augello G, Agricola E, Sala S, Santinelli V, Morady
F. Circumferential pulmonary-vein ablation for chronic atrial fibrillation. N Engl J
Med 2006;354:934941.
237. Mont L, Bisbal F, Hernandez-Madrid A, Perez-Castellano N, Vinolas X, Arenal
A, Arribas F, Fernandez-Lozano I, Bodegas A, Cobos A, Matia R, Perez-
Villacastin J, Guerra JM, Avila P, Lopez-Gil M, Castro V, Arana JI, Brugada J;
SARA investigators. Catheter ablation vs. antiarrhythmic drug treatment of per-
sistent atrial fibrillation: a multicentre, randomized, controlled trial (SARA
study). Eur Heart J 2014;35:501507.
238. Forleo GB, Mantica M, De Luca L, Leo R, Santini L, Panigada S, De Sanctis V,
Pappalardo A, Laurenzi F, Avella A, Casella M, Dello Russo A, Romeo F,
Pelargonio G, Tondo C. Catheter ablation of atrial fibrillation in patients with
diabetes mellitus type 2: results from a randomized study comparing pulmonary
vein isolation versus antiarrhythmic drug therapy. J Cardiovasc Electrophysiol
2009;20:2228.
239. Wilber DJ, Pappone C, Neuzil P, De Paola A, Marchlinski F, Natale A, Macle L,
Daoud EG, Calkins H, Hall B, Reddy V, Augello G, Reynolds MR, Vinekar C, Liu
CY, Berry SM, Berry DA; ThermoCool AF Trial Investigators. Comparison of
antiarrhythmic drug therapy and radiofrequency catheter ablation in patients
with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA
2010;303:333340.
240. Wazni OM, Marrouche NF, Martin DO, Verma A, Bhargava M, Saliba W, Bash
D, Schweikert R, Brachmann J, Gunther J, Gutleben K, Pisano E, Potenza D,
Fanelli R, Raviele A, Themistoclakis S, Rossillo A, Bonso A, Natale A.
Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symp-
tomatic atrial fibrillation: a randomized trial. JAMA 2005;293:26342640.
241. Morillo CA, Verma A, Connolly SJ, Kuck KH, Nair GM, Champagne J, Sterns
LD, Beresh H, Healey JS, Natale A; RAAFT Investigators. Radiofrequency abla-
tion vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrilla-
tion (RAAFT-2): a randomized trial. JAMA 2014;311:692700.
242. Cosedis Nielsen J, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H,
Kongstad O, Pehrson S, Englund A, Hartikainen J, Mortensen LS, Hansen PS.
Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl
J Med 2012;367:1587
1595.
243. Pokorney SD, Kim S, Thomas L, Fonarow GC, Kowey PR, Gersh BJ, Mahaffey
KW, Peterson ED, Piccini JP; Outcomes Registry for Better Informed Treatment
of Atrial Fibrillation Investigators. Cardioversion and subsequent quality of life and
natural history of atrial fibrillation. Am Heart J 2017;185:5966.
244. Mantovan R, Macle L, De Martino G, Chen J, Morillo CA, Novak P, Calzolari V,
Khaykin Y, Guerra PG, Nair G, Torrecilla EG, Verma A. Relationship of quality
of life with procedural success of atrial fibrillation (AF) ablation and postabla-
tion AF burden: substudy of the STAR AF randomized trial. Can J Cardiol
2013;29:12111217.
245. Rienstra M, Hobbelt AH, Alings M, Tijssen JGP, Smit MD, Brugemann J,
Geelhoed B, Tieleman RG, Hillege HL, Tukkie R, Van Veldhuisen DJ, Crijns H,
Van Gelder IC; RACE Investigators. Targeted therapy of underlying conditions
improves sinus rhythm maintenance in patients with persistent atrial fibrillation:
results of the RACE 3 trial. Eur Heart J 2018;39:29872996.
ESC Guidelines 91

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
246. Blomstrom-Lundqvist C, Gizurarson S, Schwieler J, Jensen SM, Bergfeldt L,
Kenneback G, Rubulis A, Malmborg H, Raatikainen P, Lonnerholm S, Hoglund
N, Mortsell D. Effect of catheter ablation vs antiarrhythmic medication on qual-
ity of life in patients with atrial fibrillation: the CAPTAF randomized clinical trial.
JAMA 2019;321:10591068.
247. Mark DB, Anstrom KJ, Sheng S, Piccini JP, Baloch KN, Monahan KH, Daniels
MR, Bahnson TD, Poole JE, Rosenberg Y, Lee KL, Packer DL; CABANA
Investigators. Effect of catheter ablation vs medical therapy on quality of life
among patients with atrial fibrillation: the CABANA randomized clinical trial.
JAMA 2019.
248. Gaita F, Scaglione M, Battaglia A, Matta M, Gallo C, Galata M, Caponi D, Di
Donna P, Anselmino M. Very long-term outcome following transcatheter abla-
tion of atrial fibrillation. Are results maintained after 10 years of follow-
up?Europace 2018;20:443450.
249. Donal E, Lip GY, Galderisi M, Goette A, Shah D, Marwan M, Lederlin M,
Mondillo S, Edvardsen T, Sitges M, Grapsa J, Garbi M, Senior R, Gimelli A,
Potpara TS, Van Gelder IC, Gorenek B, Mabo P, Lancellotti P, Kuck KH,
Popescu BA, Hindricks G, Habib G, Cardim NM, Cosyns B, Delgado V, Haugaa
KH, Muraru D, Nieman K, Boriani G, Cohen A. EACVI/EHRA Expert
Consensus Document on the role of multi-modality imaging for the evaluation
of patients with atrial fibrillation. Eur Heart J Cardiovasc Imaging
2016;17:355383.
250. Delgado V, Di Biase L, Leung M, Romero J, Tops LF, Casadei B, Marrouche N,
Bax JJ. Structure and function of the left atrium and left atrial appendage: AF
and stroke implications. J Am Coll Cardiol 2017;70:31573172.
251. Oakes RS, Badger TJ, Kholmovski EG, Akoum N, Burgon NS, Fish EN, Blauer JJ,
Rao SN, DiBella EV, Segerson NM, Daccarett M, Windfelder J, McGann CJ,
Parker D, MacLeod RS, Marrouche NF. Detection and quantification of left
atrial structural remodeling with delayed-enhancement magnetic resonance
imaging in patients with atrial fibrillation. Circulation 2009;119:17581767.
252. Cameli M, Lisi M, Righini FM, Massoni A, Natali BM, Focardi M, Tacchini D,
Geyer A, Curci V, Di Tommaso C, Lisi G, Maccherini M, Chiavarelli M, Massetti
M, Tanganelli P, Mondillo S. Usefulness of atrial deformation analysis to predict
left atrial fibrosis and endocardial thickness in patients undergoing mitral valve
operations for severe mitral regurgitation secondary to mitral valve prolapse.
Am J Cardiol 2013;111:595601.
253. Nakamori S, Nezafat M, Ngo LH, Manning WJ, Nezafat R. Left atrial epicardial
fat volume is associated with atrial fibrillation: a prospective cardiovascular mag-
netic resonance 3D Dixon Study. J Am Heart Assoc 2018;7.
254. Murphy A, Banerjee A, Breithardt G, Camm AJ, Commerford P, Freedman B,
Gonzalez-Hermosillo JA, Halperin JL, Lau CP, Perel P, Xavier D, Wood D,
Jouven X, Morillo CA. The World Heart Federation roadmap for nonvalvular
atrial fibrillation. Glob Heart 2017;12:273284.
255. Timmis A, Townsend N, Gale CP, Torbica A, Lettino M, Petersen SE, Mossialos
EA, Maggioni AP, Kazakiewicz D, May HT, De Smedt D, Flather M, Zuhlke L,
Beltrame JF, Huculeci R, Tavazzi L, Hindricks G, Bax J, Casadei B, Achenbach S,
Wright L, Vardas P. European Society of Cardiology: Cardiovascular Disease
Statistics 2019. Eur Heart J 2020;41:1285.
256. Charles C, Whelan T, Gafni A. What do we mean by partnership in making
decisions about treatment?BMJ 1999;319:780782.
257. Lane DA, Aguinaga L, Blomstrom-Lundqvist C, Boriani G, Dan GA, Hills MT,
Hylek EM, LaHaye SA, Lip GY, Lobban T, Mandrola J, McCabe PJ, Pedersen SS,
Pisters R, Stewart S, Wood K, Potpara TS, Gorenek B, Conti JB, Keegan R,
Power S, Hendriks J, Ritter P, Calkins H, Violi F, Hurwitz J. Cardiac tachyar-
rhythmias and patient values and preferences for their management: the
European Heart Rhythm Association (EHRA) consensus document endorsed
by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society
(APHRS), and Sociedad Latinoamericana de Estimulacion Cardiaca y
Electrofisiologia (SOLEACE). Europace 2015;17:1747
1769.
258. Bergtun S, Oterhals K, Fridlund B. Patients’ experiences 1-6 months after atrial
fibrillation ablation: an holistic perspective. J Adv Nurs 2019;75:150160.
259. Borg Xuereb C, Shaw RL, Lane DA. Patients’ and physicians’ experiences of
atrial fibrillation consultations and anticoagulation decision-making: a multi-
perspective IPA design. Psychol Health 2016;31:436455.
260. Loewen PS, Ji AT, Kapanen A, McClean A. Patient values and preferences for
antithrombotic therapy in atrial fibrillation. A narrative systematic review.
Thromb Haemost 2017;117:10071022.
261. Seaburg L, Hess EP, Coylewright M, Ting HH, McLeod CJ, Montori VM. Shared
decision making in atrial fibrillation: where we are and where we should be
going. Circulation 2014;129:704710.
262. Bajorek BV, Ogle SJ, Duguid MJ, Shenfield GM, Krass I. Management of warfarin
in atrial fibrillation: views of health professionals, older patients and their carers.
Med J Aust 2007;186:175180.
263. HessEP,KnoedlerMA,ShahND,KlineJA,BreslinM,BrandaME,PencilleLJ,Asplin
BR,NestlerDM,SadostyAT,StiellIG,TingHH,MontoriVM.Thechestpainchoice
decision aid: a randomized trial. Cir c Cardiovasc Qual Outcomes 2012;5:251259.
264. Lane DA, Meyerhoff J, Rohner U, Lip GYH. Atrial fibrillation patient preferences
for oral anticoagulation and stroke knowledge: results of a conjoint analysis. Clin
Cardiol 2018;41:855861.
265. Lindberg T, Sanmartin Berglund J, Elmstahl S, Bohman DM. Older individuals’
need for knowledge and follow-up about their chronic atrial fibrillation, lifelong
medical treatment and medical controls. Scand J Caring Sci 2017;31:10221030.
266. Palacio AM, Kirolos I, Tamariz L. Patient values and preferences when choosing
anticoagulants. Patient Prefer Adherence 2015;9:133138.
267. Lane DA, Lip GY. Patient’s values and preferences for stroke prevention in
atrial fibrillation: balancing stroke and bleeding risk with oral anticoagulation.
Thromb Haemost 2014;111:381383.
268. MacLean S, Mulla S, Akl EA, Jankowski M, Vandvik PO, Ebrahim S, McLeod S,
Bhatnagar N, Guyatt GH. Patient values and preferences in decision making for
antithrombotic therapy: a systematic review: Antithrombotic Therapy and
Prevention of Thrombosis, 9th ed: American College of Chest Physicians
Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e1Se23S.
269. Desteghe L, Engelhard L, Raymaekers Z, Kluts K, Vijgen J, Dilling-Boer D,
Koopman P, Schurmans J, Dendale P, Heidbuchel H. Knowledge gaps in patients
with atrial fibrillation revealed by a new validated knowledge questionnaire. Int J
Cardiol 2016;223
:906914.
270. Frankel DS, Parker SE, Rosenfeld LE, Gorelick PB. HRS/NSA 2014 Survey of
atrial fibrillation and stroke: gaps in knowledge and perspective, opportunities
for improvement. J Stroke Cerebro vasc Dis 2015;24:1691700.
271. Lane DA, Ponsford J, Shelley A, Sirpal A, Lip GY. Patient knowledge and per-
ceptions of atrial fibrillation and anticoagulant therapy: effects of an educational
intervention programme. The West Birmingham Atrial Fibrillation Project. Int J
Cardiol 2006;110:354358.
272. McCabe PJ, Schad S, Hampton A, Holland DE. Knowledge and self-management
behaviors of patients with recently detected atrial fibrillation. Heart Lung
2008;37:7990.
273. Ihara M, Washida K. Linking atrial fibrillation with Alzheimer’s disease: epide-
miological, pathological, and mechanistic evidence. J Alzheimers Dis
2018;62:6172.
274. Lip GYH, Lane DA, Sarwar S. Streamlining primary and secondary care manage-
ment pathways for stroke prevention in atrial fibrillation. Eur Heart J
2017;38:29802982.
275. Guo Y, Lane DA, Wang L, Chen Y, Lip GYH; mAF-App II Trial investigators.
Mobile Health (mHealth) technology for improved screening, patient involve-
ment and optimising integrated care in atrial fibrillation: the mAFA (mAF-App)
II randomised trial. Int J Clin Pract 2019:e13352.
276. Franchi C, Antoniazzi S, Ardoino I, Proietti M, Marcucci M, Santalucia P,
Monzani V, Mannucci PM, Nobili A, Collaborators S-A. Simulation-based educa-
tion for physicians to increase oral anticoagulants in hospitalized elderly patients
with atrial fibrillation. Am J Med 2019;132:e634e647.
277. Vinereanu D, Lopes RD, Bahit MC, Xavier D, Jiang J, Al-Khalidi HR, He W, Xian
Y, Ciobanu AO, Kamath DY, Fox KA, Rao MP, Pokorney SD, Berwanger O,
Tajer C, de Barros ESPGM, Roettig ML, Huo Y, Granger CB; IMPACT-AF
Investigators. A multifaceted intervention to improve treatment with oral anti-
coagulants in atrial fibrillation (IMPACT-AF): an international, cluster-
randomised trial. Lancet 2017;390:17371746.
278. Raparelli V, Proietti M, Cangemi R, Lip GY, Lane DA, Basili S. Adherence to
oral anticoagulant therapy in patients with atrial fibrillation. Focus on non-
vitamin K antagonist oral anticoagulants. Thromb Haemost 2017;117:209218.
279. Parimbelli E, Sacchi L, Budasu R, Napolitano C, Peleg M, Quaglini S. The role of
nurses in e-health: the MobiGuide project experience. Stud Health Technol
Inform 2016;225:153157.
280. Guo Y, Chen Y, Lane DA, Liu L, Wang Y, Lip GYH. Mobile health technology
for atrial fibrillation management integrating decision support, education, and
patient involvement: mAF App trial. Am J Med 2017;130:13881396.e6.
281. Kotecha D, Chua WWL, Fabritz L, Hendriks J, Casadei B, Schotten U, Vardas P,
Heidbuchel H, Dean V, Kirchhof P, European Society of Cardiology (ESC)
Atrial Fibrillation Guidelines Taskforce, the CATCH ME consortium, and the
European Heart Rhythm Association (EHRA). European Society of Cardiology
smartphone and tablet applications for patients with atrial fibrillation and their
health care providers. Europace 2018;20:225
233.
282. Lee J-A, Evangelista LS, Moore AA, Juth V, Guo Y, Gago-Masague S, Lem
CG, Nguyen M, Khatibi P, Baje M, Amin AN. Feasibility study of a mobile
health intervention for older adults on oral anticoagulation therapy.
Gerontol Geriatr Med 2016;2. doi:10.1177/2333721416672970. Published
2016 Oct 7.
283. Stephan LS, Dytz Almeida E, Guimaraes RB, Ley AG, Mathias RG, Assis MV,
Leiria TL. Processes and recommendations for creating mHealth apps for low-
income populations. JMIR Mhealth Uhealth 2017;5:e41.
284. Clarkesmith DE, Pattison HM, Khaing PH, Lane DA. Educational and behaviou-
ral interventions for anticoagulant therapy in patients with atrial fibrillation.
Cochrane Database Syst Rev 2017;4:CD008600.
92 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
285. Man-Son-Hing M, Laupacis A, O’Connor AM, Biggs J, Drake E, Yetisir E, Hart
RG. A patient decision aid regarding antithrombotic therapy for stroke preven-
tion in atrial fibrillation: a randomized controlled trial. JAMA
1999;282:737743.
286. McAlister FA, Man-Son-Hing M, Straus SE, Ghali WA, Anderson D, Majumdar
SR, Gibson P, Cox JL, Fradette M; Decision Aid in Atrial Fibrillation
Investigators. Impact of a patient decision aid on care among patients with
nonvalvular atrial fibrillation: a cluster randomized trial. CMAJ
2005;173:496501.
287. Thomson RG, Eccles MP, Steen IN, Greenaway J, Stobbart L, Murtagh MJ, May
CR. A patient decision aid to support shared decision-making on anti-
thrombotic treatment of patients with atrial fibrillation: randomised controlled
trial. Qual Saf Health Care 2007;16:216223.
288. Eckman MH, Costea A, Attari M, Munjal J, Wise RE, Knochelmann C, Flaherty
ML, Baker P, Ireton R, Harnett BM, Leonard AC, Steen D, Rose A, Kues J.
Shared decision-making tool for thromboprophylaxis in atrial fibrillation a
feasibility study. Am Heart J 2018;199:1321.
289. Eckman MH, Lip GY, Wise RE, Speer B, Sullivan M, Walker N, Kissela B,
Flaherty ML, Kleindorfer D, Baker P, Ireton R, Hoskins D, Harnett BM, Aguilar
C, Leonard AC, Arduser L, Steen D, Costea A, Kues J. Impact of an atrial fibril-
lation decision support tool on thromboprophylaxis for atrial fibrillation. Am
Heart J 2016;176:1727.
290. Karlsson LO, Nilsson S, Bang M, Nilsson L, Charitakis E, Janzon M. A clinical
decision support tool for improving adherence to guidelines on anticoagulant
therapy in patients with atrial fibrillation at risk of stroke: a cluster-randomized
trial in a Swedish primary care setting (the CDS-AF study). PLoS Med
2018;15:e1002528.
291. Vinereanu D, Lopes RD, Mulder H, Gersh BJ, Hanna M, de Barros ESPGM, Atar
D, Wallentin L, Granger CB, Alexander JH; ARISTOTLE Investigators.
Echocardiographic risk factors for stroke and outcomes in patients with atrial
fibrillation anticoagulated with apixaban or warfarin. Stroke
2017;48:32663273.
292. Hendriks JM, de Wit R, Crijns HJ, Vrijhoef HJ, Prins MH, Pisters R, Pison LA,
Blaauw Y, Tieleman RG. Nurse-led care vs. usual care for patients with atrial
fibrillation: results of a randomized trial of integrated chronic care vs. routine
clinical care in ambulatory patients with atrial fibrillation. Eur Heart J
2012;33:26922699.
293. Stewart S, Ball J, Horowitz JD, Marwick TH, Mahadevan G, Wong C,
Abhayaratna WP, Chan YK, Esterman A, Thompson DR, Scuffham PA,
Carrington MJ. Standard versus atrial fibrillation-specific management strategy
(SAFETY) to reduce recurrent admission and prolong survival: pragmatic, multi-
centre, randomised controlled trial. Lancet 2015;385:775784.
294. Carter L, Gardner M, Magee K, Fearon A, Morgulis I, Doucette S, Sapp JL, Gray
C, Abdelwahab A, Parkash R. An integrated management approach to atrial
fibrillation. J Am Heart Assoc 2016;5.
295. Wijtvliet E, Tieleman RG, van Gelder IC, Pluymaekers NAHA, Rienstra M,
Folkeringa RJ, Bronzwaer P, Elvan A, Elders J, Tukkie R, Luermans JGLM, Van
Asselt ADIT, Van Kuijk SMJ, Tijssen JG, Crijns HJGM; RACE Investigators.
Nurse-led vs. usual-care for atrial fibrillation. Eur Heart J 2020;41:634641.
296. Gallagher C, Elliott AD, Wong CX, Rangnekar G, Middeldorp ME, Mahajan R,
Lau DH, Sanders P, Hendriks JML. Integrated care in atrial fibrillation: a system-
atic review and meta-analysis. Heart 2017;103:1947 1953.
297. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method
for characterising and designing behaviour change interventions.
Implement Sci
2011;6:42.
298. Lip GYH, Lane DA, Potpara TS. Innovative strategies to improve adherence to
non-vitamin K antagonist oral anticoagulants for stroke prevention in atrial
fibrillation. Eur Heart J 2018;39:14041406.
299. Seligman WH, Das-Gupta Z, Jobi-Odeneye AO, Arbelo E, Banerjee A,
Bollmann A, Caffrey-Armstrong B, Cehic DA, Corbalan R, Collins M,
Dandamudi G, Dorairaj P, Fay M, Van Gelder IC, Goto S, Granger CB, Gyorgy
B, Healey JS, Hendriks JM, Hills MT, Hobbs FDR, Huisman MV, Koplan KE, Lane
DA, Lewis WR, Lobban T, Steinberg BA, McLeod CJ, Moseley S, Timmis A,
Yutao G, Camm AJ. Development of an international standard set of outcome
measures for patients with atrial fibrillation: a report of the International
Consortium for Health Outcomes Measurement (ICHOM) atrial fibrillation
working group. Eur Heart J 2020;41:11321140.
300. Dobler CC, Harb N, Maguire CA, Armour CL, Coleman C, Murad MH.
Treatment burden should be included in clinical practice guidelines. BMJ
2018;363:k4065.
301. Eton DT, Ramalho de Oliveira D, Egginton JS, Ridgeway JL, Odell L, May CR,
Montori VM. Building a measurement framework of burden of treatment in
complex patients with chronic conditions: a qualitative study. Patient Relat
Outcome Meas 2012;3:3949.
302. Tran VT, Montori VM, Eton DT, Baruch D, Falissard B, Ravaud P. Development
and description of measurement properties of an instrument to assess
treatment burden among patients with multiple chronic conditions. BMC Med
2012;10:68.
303. Vijan S, Hayward RA, Ronis DL, Hofer TP. Brief report: the burden of diabetes
therapy: implications for the design of effective patient-centered treatment regi-
mens. J Gen Intern Med 2005;20:479482.
304. Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to
treatment: three decades of research. A comprehensive review. J Clin Pharm
Ther 2001;26:331342.
305. Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF,
Magid DJ. Effect of medication nonadherence on hospitalization and mor-
tality among patients with diabetes mellitus. Arch Intern Med
2006;166:18361841.
306. Rasmussen JN, Chong A, Alter DA. Relationship between adherence to
evidence-based pharmacotherapy and long-term mortality after acute myocar-
dial infarction. JAMA 2007;297:177186.
307. May C, Montori VM, Mair FS. We need minimally disruptive medicine. BMJ
2009;339:b2803.
308. Wilcox AR, Dragnev MC, Darcey CJ, Siegel CA. A new tool to measure the
burden of Crohn’s disease and its treatment: do patient and physician percep-
tions match?Inflamm Bowel Dis 2010;16:645650.
309. Bohlen K, Scoville E, Shippee ND, May CR, Montori VM. Overwhelmed
patients: a videographic analysis of how patients with type 2 diabetes and clini-
cians articulate and address treatment burden during clinical encounters.
Diabetes Care 2012;
35:4749.
310. Buffel du Vaure C, Ravaud P, Baron G, Barnes C, Gilberg S, Boutron I.
Potential workload in applying clinical practice guidelines for patients with
chronic conditions and multimorbidity: a systematic analysis. BMJ Open
2016;6:e010119.
311. Potpara TS, Mihajlovic M, Zec N, Marinkovic M, Kovacevic V, Simic J, Kocijancic
A, Vajagic L, Jotic A, Mujovic N, Stankovic G. Self-reported treatment burden in
patients with atrial fibrillation: quantification, major determinants and implica-
tions for integrated holistic management of the arrhythmia. Europace 2020;
doi:10.1093/europace/euaa210.
312. Tran VT, Harrington M, Montori VM, Barnes C, Wicks P, Ravaud P. Adaptation
and validation of the Treatment Burden Questionnaire (TBQ) in English using
an internet platform. BMC Med 2014;12:109.
313. Steinberg BA, Dorian P, Anstrom KJ, Hess R, Mark DB, Noseworthy PA,
Spertus JA, Piccini JP. Patient-reported outcomes in atrial fibrillation research:
results of a Clinicaltrials.gov analysis. JACC Clin Electrophysiol 2019;5:599605.
314. Calvert M, Kyte D, Price G, Valderas JM, Hjollund NH. Maximising the impact
of patient reported outcome assessment for patients and society. BMJ
2019;364:k5267.
315. Rotenstein LS, Huckman RS, Wagle NW. Making patients and doctors happier
the potential of patient-reported outcomes. N Engl J Med
2017;377:13091312.
316. Van Der Wees PJ, Nijhuis-Van Der Sanden MW, Ayanian JZ, Black N, Westert
GP, Schneider EC. Integrating the use of patient-reported outcomes for both
clinical practice and performance measurement: views of experts from 3 coun-
tries. Milbank Q 2014;92:754775.
317. Arbelo E, Aktaa S, Bollmann A, D’Avila A, Drossart I, Dwight J, Hills MT,
Hindricks G, Kusumoto FM, Lane DA, Lau DH, Lettino M, Lip GYH, Lobban T,
Pak H-N, Potpara T, Saenz LC, Van Gelder IC, Varosy P, Gale CP, Dagres N.
Quality indicators for the care and outcomes of adults with atrial fibrillation.
Task Force for the development of quality indicators in Atrial Fibrillation of the
European Heart Rhythm Association (EHRA) and of the European Society of
Cardiology (ESC): Developed in collaboration with the Heart Rhythm Society
(HRS), the Asia Pacific Heart Rhythm Society (APHRS) and the Latin-American
Heart Rhythm Society (LAHRS). Europace 2020;doi:10.1093/europace/euaa253.
318. Lip GYH. The ABC pathway: an integrated approach to improve AF manage-
ment. Nat Rev Cardiol 2017;14:627628.
319. Proietti M, Romiti GF, Olshansky B, Lane DA, Lip GYH. Improved outcomes by
integrated care of anticoagulated patients with atrial fibrillation using the simple
ABC (Atrial Fibrillation Better Care) Pathway. Am J Med
2018;131:13591366.e6.
320. Yoon M, Yang PS, Jang E, Yu HT, Kim TH, Uhm JS, Kim JY, Sung JH, Pak HN,
Lee MH, Joung B, Lip GYH. Improved population-based clinical outcomes of
patients with atrial fibrillation by compliance with the simple ABC (Atrial
Fibrillation Better Care) pathway for integrated care management: a nationwide
cohort study. Thromb Haemost 2019;19:16951703.
321. Pastori D, Pignatelli P, Menichelli D, Violi F, Lip GYH. Integrated care manage-
ment of patients with atrial fibrillation and risk of cardiovascular events: the
ABC (Atrial fibrillation Better Care) pathway in the ATHERO-AF study cohort.
Mayo Clin Proc 2019;94:12611267
322. Pastori D, Farcomeni A, Pignatelli P, Violi F, Lip GY. ABC (Atrial fibrillation
Better Care) pathway and healthcare costs in atrial fibrillation: the ATHERO-
AF study. Am J Med 2019;132:856861.
ESC Guidelines 93

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
323. Guo Y, Lane DA, Wang L, Zhang H, Wang H, Zhang W, Wen J, Xing Y, Wu F,
Xia Y, Liu T, Wu F, Liang Z, Liu F, Zhao Y, Li R, Li X, Zhang L, Guo J, Burnside
G, Chen Y, Lip GYH; mAF-App II Trial Investigators. Mobile health technology
to improve care for patients with atrial fibrillation. J Am Coll Cardiol
2020;75:15231534.
324. Pisters R, Lane DA, Marin F, Camm AJ, Lip GY. Stroke and thromboembolism
in atrial fibrillation. Circ J 2012;76:22892304.
325. Szymanski FM, Lip GY, Filipiak KJ, Platek AE, Hrynkiewicz-Szymanska A, Opolski
G. Stroke risk factors beyond the CHA(2)DS(2)-VASc score: can we improve
our identification of ‘high stroke risk’ patients with atrial fibrillation?Am J Cardiol
2015;116:17811788.
326. Atrial Fibrillation Investigators. Echocardiographic predictors of stroke in
patients with atrial fibrillation: a prospective study of 1066 patients from 3 clini-
cal trials. Arch Intern Med 1998;158:13161320.
327. Ntaios G, Lip GY, Lambrou D, Papavasileiou V, Manios E, Milionis H, Spengos
K, Makaritsis K, Vemmos K. Leukoaraiosis and stroke recurrence risk in patients
with and without atrial fibrillation. Neurology 2015;84:12131219.
328. Esteve-Pastor MA, Roldan V, Rivera-Caravaca JM, Ramirez-Macias I, Lip GYH,
Marin F. The use of biomarkers in clinical management guidelines: a critical
appraisal. Thromb Haemost 2019;119:19011919.
329. Hijazi Z, Oldgren J, Siegbahn A, Wallentin L. Application of biomarkers for risk
stratification in patients with atrial fibrillation. Clin Chem 2017;63:152164.
330. Yaghi S, Kamel H. Stratifying stroke risk in atrial fibrillation: beyond clinical risk
scores. Stroke 2017;48:26652670.
331. Ioannou A, Papageorgiou N, Falconer D, Rehal O, Sewart E, Zacharia E,
Toutouzas K, Vlachopoulos C, Siasos G, Tsioufis C, Tousoulis D. Biomarkers
associated with stroke risk in atrial fibrillation. Curr Med Chem
2019;26:803823.
332. Sepehri Shamloo A, Bollmann A, Dagres N, Hindricks G, Arya A. Natriuretic
peptides: biomarkers for atrial fibrillation management. Clin Res Cardiol
2020;109:957966.
333. Decker JJ, Norby FL, Rooney MR, Soliman EZ, Lutsey PL, Pankow JS, Alonso A,
Chen LY. Metabolic syndrome and risk of ischemic stroke in atrial fibrillation:
ARIC Study. Stroke 2019;50:30453050.
334. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratifi-
cation for predicting stroke and thromboembolism in atrial fibrillation using a
novel risk factor-based approach: the Euro Heart Survey on atrial fibrillation.
Chest 2010;137:263272.
335. Banerjee A, Taillandier S, Olesen JB, Lane DA, Lallemand B, Lip GY, Fauchier L.
Ejection fraction and outcomes in patients with atrial fibrillation and heart fail-
ure: the Loire Valley Atrial Fibrillation Project. Eur J Heart Fail
2012;14:295301.
336. Jung H, Sung JH, Yang PS, Jang E, Yu HT, Kim TH, Pak HN, Lee MH, Joung B,
Lip GYH. Stroke risk stratification for atrial fibrillation patients with hypertro-
phic cardiomyopathy. J Am Coll Cardiol 2018;72:24092411.
337. Jung H, Yang PS, Jang E, Yu HT, Kim TH, Uhm JS, Kim JY, Pak HN, Lee MH,
Joung B, Lip GYH. Effectiveness and safety of non-vitamin K antagonist oral anti-
coagulants in patients with atrial fibrillation with hypertrophic cardiomyopathy:
a nationwide cohort study. Chest 2019;155:354363.
338. Kim D, Yang PS, Kim TH, Jang E, Shin H, Kim HY, Yu HT, Uhm JS, Kim JY, Pak
HN, Lee MH, Joung B, Lip GYH. Ideal blood pressure in patients with atrial
fibrillation. J Am Coll Cardiol 2018;72:12331245.
339. Lip GY, Clementy N, Pericart L, Banerjee A, Fauchier L. Stroke and major
bleeding risk in elderly patients aged >/=75 years with atrial fibrillation: the
Loire Valley Atrial Fibrillation Project. Stroke 2015;46:14350.
340. Overvad TF, Skjoth F, Lip GY, Lane DA, Albertsen IE, Rasmussen LH, Larsen
TB. Duration of diabetes mellitus and risk of thromboembolism and bleeding in
atrial fibrillation: nationwide cohort study. Stroke 2015;46:216874.
341. Lip GYH, Clementy N, Pierre B, Boyer M, Fauchier L. The impact of associated
diabetic retinopathy on stroke and severe bleeding risk in diabetic patients with
atrial fibrillation: the Loire Valley Atrial Fibrillation Project. Chest
2015;147:11031110.
342. Fangel MV, Nielsen PB, Larsen TB, Christensen B, Overvad TF, Lip GYH,
Goldhaber SZ, Jensen MB. Type 1 versus type 2 diabetes and thromboembolic
risk in patients with atrial fibrillation: a Danish nationwide cohort study. Int J
Cardiol 2018;268:137142.
343. Chao TF, Liu CJ, Liao JN, Wang KL, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC,
Chung FP, Chen TJ, Lip GY, Chen SA. Use of oral anticoagulants for stroke pre-
vention in patients with atrial fibrillation who have a history of intracranial hem-
orrhage. Circulation 2016;133:15401547.
344. Bronnum Nielsen P, Larsen TB, Gorst-Rasmussen A, Skjoth F, Rasmussen LH,
Lip GYH. Intracranial hemorrhage and subsequent ischemic stroke in patients
with atrial fibrillation: a nationwide cohort study. Chest 2015;147:16511658.
345. Nielsen PB, Larsen TB, Skjoth F, Gorst-Rasmussen A, Rasmussen LH, Lip GY.
Restarting anticoagulant treatment after intracranial hemorrhage in patients
with atrial fibrillation and the impact on recurrent stroke, mortality, and bleed-
ing: a nationwide cohort study. Circulation 2015;132:517525.
346. Lin LY, Lee CH, Yu CC, Tsai CT, Lai LP, Hwang JJ, Chen PC, Lin JL. Risk
factors and incidence of ischemic stroke in Taiwanese with nonvalvular
atrial fibrillation
a nation-wide database analysis. Atherosclerosis
2011;217:292295.
347. Anandasundaram B, Lane DA, Apostolakis S, Lip GY. The impact of atheroscler-
otic vascular disease in predicting a stroke, thromboembolism and mortality in
atrial fibrillation patients: a systematic review. J Thromb Haemost
2013;11:975987.
348. Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for
ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the
Swedish Atrial Fibrillation cohort study. Eur Heart J 2012;33:15001510.
349. Steensig K, Olesen KKW, Thim T, Nielsen JC, Jensen SE, Jensen LO, Kristensen
SD, Botker HE, Lip GYH, Maeng M. Should the presence or extent of coronary
artery disease be quantified in the CHA2DS2-VASc score in atrial fibrillation? A
report from the Western Denmark Heart Registry. Thromb Haemost
2018;118:21622170.
350. Zabalgoitia M, Halperin JL, Pearce LA, Blackshear JL, Asinger RW, Hart RG.
Transesophageal echocardiographic correlates of clinical risk of thromboembo-
lism in nonvalvular atrial fibrillation. Stroke Prevention in Atrial Fibrillation III
Investigators. J Am Coll Cardiol 1998;31:16221626.
351. Kim TH, Yang PS, Yu HT, Jang E, Uhm JS, Kim JY, Pak HN, Lee MH, Joung B, Lip
GYH. Age threshold for ischemic stroke risk in atrial fibrillation. Stroke
2018;49:18721879.
352. Chao TF, Wang KL, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Chung
FP, Liao JN, Chen TJ, Chiang CE, Lip GY, Chen SA. Age threshold for increased
stroke risk among patients with atrial fibrillation: a nationwide cohort study
from Taiwan. J Am Coll Cardiol 2015;66:13391347.
353. Nielsen PB, Skjoth F, Overvad TF, Larsen TB, Lip GYH. Female sex is a risk modi-
fier rather than a risk factor for stroke in atrial fibrillation: should we use a
CHA2DS2-VA score rather than CHA2DS2-VASc?Circulation 2018;137:832840.
354. Killu AM, Granger CB, Gersh BJ. Risk stratification for stroke in atrial fibrillation:
a critique. Eur Heart J 2019;40:12941302.
355. Rivera-Caravaca JM, Roldan V, Esteve-Pastor MA, Valdes M, Vicente V, Lip
GYH, Marin F. Long-term stroke risk prediction in patients with atrial fibrilla-
tion: comparison of the ABC-Stroke and CHA2DS2-VASc scores. J Am Heart
Assoc 2017;6: pii: JAHA.117.006490. doi: 10.1161/JAHA.117.006490.
356. Alkhouli M, Friedman PA. Ischemic stroke risk in patients with nonvalvular atrial
fibrillation: JACC review topic of the week. J Am Coll Cardiol
2019;74:30503065.
357. Wu VC, Wu M, Aboyans V, Chang SH, Chen SW, Chen MC, Wang CL, Hsieh
IC, Chu PH, Lin YS. Female sex as a risk factor for ischaemic stroke varies with
age in patients with atrial fibrillation. Heart 2020;106:534540.
358. Tomasdottir M, Friberg L, Hijazi Z, Lindback J, Oldgren J. Risk of ischemic
stroke and utility of CHA2 DS2 -VASc score in women and men with atrial
fibrillation.
Clin Cardiol 2019;42:10031009.
359. Friberg L, Benson L, Rosenqvist M, Lip GY. Assessment of female sex as a risk
factor in atrial fibrillation in Sweden: nationwide retrospective cohort study.
BMJ 2012;344:e3522.
360. Overvad TF, Potpara TS, Nielsen PB. Stroke risk stratification: CHA2DS2-VA
or CHA2DS2-VASc?Heart Lung Circ 2019;28:e14e15.
361. Nielsen PB, Overvad TF. Female sex as a risk modifier for stroke risk in atrial
fibrillation: using CHA2DS2-VASc versus CHA2DS2-VA for stroke risk stratifi-
cation in atrial fibrillation: a note of caution. Thromb Haemost 2020. doi:
10.1055/s-0040-1710014. Epub ahead of print.
362. Marzona I, Proietti M, Farcomeni A, Romiti GF, Romanazzi I, Raparelli V, Basili
S, Lip GYH, Nobili A, Roncaglioni MC. Sex differences in stroke and major
adverse clinical events in patients with atrial fibrillation: a systematic review and
meta-analysis of 993,600 patients. Int J Cardiol 2018;269:182191.
363. Friberg L, Benson L, Lip GY. Balancing stroke and bleeding risks in patients with
atrial fibrillation and renal failure: the Swedish Atrial Fibrillation Cohort study.
Eur Heart J 2015;36:297306.
364. Poli M, Philip P, Taillard J, Debruxelles S, Renou P, Orgogozo JM, Rouanet F,
Sibon I. Atrial fibrillation is a major cause of stroke in apneic patients: a pro-
spective study. Sleep Med 2017;30:251254.
365. Bassand JP, Accetta G, Al Mahmeed W, Corbalan R, Eikelboom J, Fitzmaurice
DA, Fox KAA, Gao H, Goldhaber SZ, Goto S, Haas S, Kayani G, Pieper K,
Turpie AGG, van Eickels M, Verheugt FWA, Kakkar AK; GARFIELD-AF
Investigators. Risk factors for death, stroke, and bleeding in 28,628 patients
from the GARFIELD-AF registry: rationale for comprehensive management of
atrial fibrillation. PLoS One 2018;13:e0191592.
366. Overvad TF, Rasmussen LH, Skjoth F, Overvad K, Lip GY, Larsen TB. Body
mass index and adverse events in patients with incident atrial fibrillation. Am J
Med 2013;126:640.e9-17.
94 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
367. Lip GY, Lane D, Van Walraven C, Hart RG. Additive role of plasma von
Willebrand factor levels to clinical factors for risk stratification of patients with
atrial fibrillation. Stroke 2006;37:2294 2300.
368. Fox KAA, Lucas JE, Pieper KS, Bassand JP, Camm AJ, Fitzmaurice DA,
Goldhaber SZ, Goto S, Haas S, Hacke W, Kayani G, Oto A, Mantovani LG,
Misselwitz F, Piccini JP, Turpie AGG, Verheugt FWA, Kakkar AK; GARFIELD-
AF Investigators. Improved risk stratification of patients with atrial fibrillation:
an integrated GARFIELD-AF tool for the prediction of mortality, stroke and
bleed in patients with and without anticoagulation. BMJ Open 2017;7:e017157.
369. Zhu W, Fu L, Ding Y, Huang L, Xu Z, Hu J, Hong K. Meta-analysis of ATRIA
versus CHA2DS2-VASc for predicting stroke and thromboembolism in patients
with atrial fibrillation. Int J Cardiol 2017;227:436442.
370. Singer DE, Chang Y, Borowsky LH, Fang MC, Pomernacki NK, Udaltsova N,
Reynolds K, Go AS. A new risk scheme to predict ischemic stroke and other
thromboembolism in atrial fibrillation: the ATRIA study stroke risk score. JAm
Heart Assoc 2013;2:e000250.
371. Graves KG, May HT, Knowlton KU, Muhlestein JB, Jacobs V, Lappe DL,
Anderson JL, Horne BD, Bunch TJ. Improving CHA2DS2-VASc stratification of
non-fatal stroke and mortality risk using the Intermountain Mortality Risk Score
among patients with atrial fibrillation. Open Heart 2018;5:e000907.
372. Hijazi Z, Lindback J, Alexander JH, Hanna M, Held C, Hylek EM, Lopes RD,
Oldgren J, Siegbahn A, Stewart RA, White HD, Granger CB, Wallentin L;
ARISTOTLE and STABILITY Investigators. The ABC (age, biomarkers, clinical
history) stroke risk score: a biomarker-based risk score for predicting stroke in
atrial fibrillation. Eur Heart J 2016;37:158290.
373. Hijazi Z, Lindahl B, Oldgren J, Andersson U, Lindback J, Granger CB, Alexander
JH, Gersh BJ, Hanna M, Harjola VP, Hylek EM, Lopes RD, Siegbahn A, Wallentin
L. Repeated measurements of cardiac biomarkers in atrial fibrillation and valida-
tion of the ABC stroke score over time. J Am Heart Assoc 2017;6.
374. Oldgren J, Hijazi Z, Lindback J, Alexander JH, Connolly SJ, Eikelboom JW,
Ezekowitz MD, Granger CB, Hylek EM, Lopes RD, Siegbahn A, Yusuf S,
Wallentin L; RE-LY and ARISTOTLE Investigators. Performance and validation
of a novel biomarker-based stroke risk score for atrial fibrillation. Circulation
2016;134:16971707.
375. Berg DD, Ruff CT, Jarolim P, Giugliano RP, Nordio F, Lanz HJ, Mercuri MF,
Antman EM, Braunwald E, Morrow DA. Performance of the ABC scores for
assessing the risk of stroke or systemic embolism and bleeding in patients with
atrial fibrillation in ENGAGE AF-TIMI 48. Circulation 2019;139:760771.
376. Rivera-Caravaca JM, Marin F, Vilchez JA, Galvez J, Esteve-Pastor MA, Vicente V,
Lip GYH, Roldan V. Refining stroke and bleeding prediction in atrial fibrillation
by adding consecutive biomarkers to clinical risk scores. Stroke
2019;50:13721379.
377. Esteve-Pastor MA, Rivera-Caravaca JM, Roldan V, Vicente V, Valdes M, Marin F,
Lip GY. Long-term bleeding risk prediction in ‘real world’patients with atrial
fibrillation: comparison of the HAS-BLED and ABC-Bleeding risk scores.
Thromb Haemost 2017;117:18481858.
378. Shin SY, Han SJ, Kim JS, Im SI, Shim J, Ahn J, Lee EM, Park YM, Kim JH, Lip GYH,
Lim HE. Identification of markers associated with development of stroke in
‘clinically low-risk’ atrial fibrillation patients. J Am Heart Assoc 2019;8:e012697.
379. Chao TF, Lip GYH, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung
FP, Chen TJ, Chen SA. Age threshold for the use of non-vitamin K antagonist
oral anticoagulants for stroke prevention in patients with atrial fibrillation:
insights into the optimal assessment of age and incident comorbidities. Eur
Heart J 2019;40:15041514.
380. Nielsen PB, Larsen TB, Skjoth F, Overvad TF, Lip GY. Stroke and thromboem-
bolic event rates in atrial fibrillation according to different guideline treatment
thresholds: a nationwide cohort study. Sci Rep 2016;6:27410.
381. Fauchier L, Clementy N, Bisson A, Ivanes F, Angoulvant D, Babuty D, Lip GY.
Should atrial fibrillation patients with only 1 nongender-related CHA2DS2-
VASc risk factor be anticoagulated?Stroke 2016;47:1831 1836.
382. Chao TF, Lip GYH, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN,
Chung FP, Chen TJ, Chen SA. Relationship of aging and incident comorbidities
to stroke risk in patients with atrial fibrillation. J Am Coll Cardiol
2018;71:122132.
383. Yoon M, Yang PS, Jang E, Yu HT, Kim TH, Uhm JS, Kim JY, Pak HN, Lee MH,
Lip GYH, Joung B. Dynamic changes of CHA2DS2-VASc score and the risk of
ischaemic stroke in Asian patients with atrial fibrillation: a nationwide cohort
study. Thromb Haemost 2018;118:12961304.
384. Chao TF, Chiang CE, Chen TJ, Lip GYH, Chen SA. Reassessment of risk for
stroke during follow-up of patients with atrial fibrillation. Ann Intern Med
2019;170:663664.
385. Potpara TS, Polovina MM, Licina MM, Marinkovic JM, Prostran MS, Lip GY.
Reliable identification of ‘truly low’ thromboembolic risk in patients initially
diagnosed with ‘lone’ atrial fibrillation: the Belgrade Atrial Fibrillation Study. Circ
Arrhythm Electrophysiol 2012;5:319326.
386. Weijs B, Dudink E, de Vos CB, Limantoro I, Tieleman RG, Pisters R, Cheriex
EC, Luermans J, Crijns H. Idiopathic atrial fibrillation patients rapidly outgrow
their low thromboembolic risk: a 10-year follow-up study. Neth Heart J
2019;27:487497.
387. Chao TF, Liao JN, Tuan TC, Lin YJ, Chang SL, Lo LW, Hu YF, Chung FP, Chen
TJ, Lip GYH, Chen SA. Incident co-morbidities in patients with atrial fibrillation
initially with a CHA2DS2-VASc score of 0 (males) or 1 (females): implications
for reassessment of stroke risk in initially ‘low-risk’ patients. Thromb Haemost
2019;119:11621170.
388. Borre ED, Goode A, Raitz G, Shah B, Lowenstern A, Chatterjee R, Sharan L,
Allen LaPointe NM, Yapa R, Davis JK, Lallinger K, Schmidt R, Kosinski A, Al-
Khatib SM, Sanders GD. Predicting thromboembolic and bleeding event risk in
patients with non-valvular atrial fibrillation: a systematic review. Thromb
Haemost 2018;118:21712187.
389. Chao TF, Lip GYH, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung
FP, Chen TJ, Chen SA. Incident risk factors and major bleeding in patients with
atrial fibrillation treated with oral anticoagulants: a comparison of baseline,
follow-up and Delta HAS-BLED scores with an approach focused on modifiable
bleeding risk factors. Thromb Haemost 2018;118:768777.
390. Man-Son-Hing M, Nichol G, Lau A, Laupacis A. Choosing antithrombotic ther-
apy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern
Med 1999;159:677685.
391. Gage BF, Yan Y, Milligan PE, Waterman AD, Culverhouse R, Rich MW, Radford
MJ. Clinical classification schemes for predicting hemorrhage: results from the
National Registry of Atrial Fibrillation (NRAF). Am Heart J 2006;151:713719.
392. Fang MC, Go AS, Chang Y, Borowsky LH, Pomernacki NK, Udaltsova N, Singer
DE. A new risk scheme to predict warfarin-associated hemorrhage: the ATRIA
(Anticoagulation and Risk Factors in Atrial Fibrillation) study. J Am Coll Cardiol
2011;58:395401.
393. O’Brien EC, Simon DN, Thomas LE, Hylek EM, Gersh BJ, Ansell JE, Kowey PR,
Mahaffey KW, Chang P, Fonarow GC, Pencina MJ, Piccini JP, Peterson ED. The
ORBIT bleeding score: a simple bedside score to assess bleeding risk in atrial
fibrillation. Eur Heart J 2015;36:32583264.
394. Rohla M, Weiss TW, Pecen L, Patti G, Siller-Matula JM, Schnabel RB, Schilling R,
Kotecha D, Lucerna M, Huber K, De Caterina R, Kirchhof P. Risk factors for
thromboembolic and bleeding events in anticoagulated patients with atrial fibril-
lation: the prospective, multicentre observational PREvention oF thromboem-
bolic events European Registry in Atrial Fibrillation (PREFER in AF). BMJ
Open 2019;9:e022478.
395. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-
friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients
with atrial fibrillation: the Euro Heart Survey. Chest 2010;138:10931100.
396. Mori N, Sotomi Y, Hirata A, Hirayama A, Sakata Y, Higuchi Y. External valida-
tion of the ORBIT bleeding score and the HAS-BLED score in nonvalvular atrial
fibrillation patients using direct oral anticoagulants (Asian data from the
DIRECT registry). Am J Cardiol 2019;124:10441048.
397. Yao X, Gersh BJ, Sangaralingham LR, Kent DM, Shah ND, Abraham NS,
Noseworthy PA. Comparison of the CHA2DS2-VASc, CHADS2, HAS-BLED,
ORBIT, and ATRIA risk scores in predicting non-vitamin K antagonist oral
anticoagulants-associated bleeding in patients with atrial fibrillation. Am J Cardiol
2017;120:15491556.
398. Rutherford OW, Jonasson C, Ghanima W, Holst R, Halvorsen S. New score
for assessing bleeding risk in patients with atrial fibrillation treated with
NOACs. Open Heart 2018;5:e000931.
399. Thomas MR, Lip GY. Novel risk markers and risk assessments for cardiovascu-
lar disease. Circ Res 2017;120:133149.
400. Khan AA, Lip GYH. The prothrombotic state in atrial fibrillation: pathophysio-
logical and management implications. Cardiovasc Res 2019;115:3145.
401. Ban N, Siegfried CJ, Lin JB, Shui YB, Sein J, Pita-Thomas W, Sene A, Santeford
A, Gordon M, Lamb R, Dong Z, Kelly SC, Cavalli V, Yoshino J, Apte RS. GDF15
is elevated in mice following retinal ganglion cell death and in glaucoma patients.
JCI Insight 2017;2:pii: 91455. doi: 10.1172/jci.insight.91455.
402. Hijazi Z, Oldgren J, Lindback J, Alexander JH, Connolly SJ, Eikelboom JW,
Ezekowitz MD, Held C, Hylek EM, Lopes RD, Siegbahn A, Yusuf S, Granger CB,
Wallentin L; ARISTOTLE and RE-LY Investigators. The novel biomarker-based
ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial
fibrillation: a derivation and validation study. Lancet 2016;387:23022311.
403. Esteve-Pastor MA, Rivera-Caravaca JM, Roldan V, Vicente V, Valdes M, Marin F,
Lip GYH. Long-term bleeding risk prediction in ‘real world’ patients with atrial
fibrillation: comparison of the HAS-BLED and ABC-Bleeding risk scores. The
Murcia Atrial Fibrillation Project. Thromb Haemost 2017;117:18481858.
404. Caldeira D, Costa J, Fernandes RM, Pinto FJ, Ferreira JJ. Performance of the
HAS-BLED high bleeding-risk category, compared to ATRIA and
HEMORR2HAGES in patients with atrial fibrillation: a systematic review and
meta-analysis. J Interv Card Electrophysiol 2014;40:277284.
ESC Guidelines 95

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
405. Zhu W, He W, Guo L, Wang X, Hong K. The HAS-BLED score for predicting
major bleeding risk in anticoagulated patients with atrial fibrillation: a systematic
review and meta-analysis. Clin Cardiol 2015;38:555561.
406. Chang G, Xie Q, Ma L, Hu K, Zhang Z, Mu G, Cui Y. Accuracy of HAS-BLED
and other bleeding risk assessment tools in predicting major bleeding events in
atrial fibrillation: a network meta-analysis. J Thromb Haemost 2020;18:791801.
407. Lip GY, Lane DA. Bleeding risk assessment in atrial fibrillation: observations on
the use and misuse of bleeding risk scores. J Thromb Haemost
2016;14:17111714.
408. Chao TF, Lip GYH, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung
FP, Chen TJ, Chen SA. Major bleeding and intracranial hemorrhage risk predic-
tion in patients with atrial fibrillation: attention to modifiable bleeding risk fac-
tors or use of a bleeding risk stratification score? A nationwide cohort study. Int
J Cardiol 2018;254:157161.
409. Guo Y, Zhu H, Chen Y, Lip GYH. Comparing bleeding risk assessment focused
on modifiable risk factors only versus validated bleeding risk scores in atrial
fibrillation. Am J Med 2018;131:185192.
410. Esteve-Pastor MA, Rivera-Caravaca JM, Shantsila A, Roldan V, Lip GYH, Marin
F. Assessing bleeding risk in atrial fibrillation patients: comparing a bleeding risk
score based only on modifiable bleeding risk factors against the HAS-BLED
score. The AMADEUS trial. Thromb Haemost 2017;117:22612266.
411. Guo Y, Lane DA, Chen Y, Lip GYH; mAF-App II Trial investigators. Regular
bleeding risk assessment associated with reduction in bleeding outcomes: the
mAFA-II randomized trial. Am J Med 2020:pii: S0002-9343(20)30274-6.
412. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to pre-
vent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med
2007;146:857867.
413. De Caterina R, Husted S, Wallentin L, Andreotti F, Arnesen H, Bachmann F,
Baigent C, Huber K, Jespersen J, Kristensen SD, Lip GY, Morais J, Rasmussen
LH, Siegbahn A, Verheugt FW, Weitz JI. Vitamin K antagonists in heart disease:
current status and perspectives (Section III). Position paper of the ESC working
group on thrombosis Task Force on anticoagulants in heart disease. Thromb
Haemost 2013;110:10871107.
414. WanY,HeneghanC,PereraR,RobertsN,HollowellJ,GlasziouP,BankheadC,Xu
Y. Anticoagulation control and prediction of adverse events in patients with atrial
fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes 2008;1:8491.
415. Sjalander S, Sjogren V, Renlund H, Norrving B, Sjalander A. Dabigatran, rivarox-
aban and apixaban vs. high TTR warfarin in atrial fibrillation. Thromb Res
2018;167:113118.
416. Amin A, Deitelzweig S, Jing Y, Makenbaeva D, Wiederkehr D, Lin J, Graham J.
Estimation of the impact of warfarin’s time-in-therapeutic range on stroke and
major bleeding rates and its influence on the medical cost avoidance associated
with novel oral anticoagulant use-learnings from ARISTOTLE, ROCKET-AF,
and RE-LY trials. J Thromb Thrombolysis 2014;38:150159.
417. Apostolakis S, Sullivan RM, Olshansky B, Lip GYH. Factors affecting quality of
anticoagulation control among patients with atrial fibrillation on warfarin: the
SAMe-TT(2)R(2) score. Chest 2013;144:15551563.
418. Proietti M, Lip GY. Simple decision-making between a vitamin K antagonist and
a non-vitamin K antagonist oral anticoagulant: using the SAMe-TT2R2 score.
Eur Heart J Cardiovasc Pharmacother 2015;1:150152.
419. Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J,
Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R,
Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L; RE-LY Steering
Committee Investigators. Dabigatran versus warfarin in patients with atrial fibril-
lation. N Engl J Med 2009;361:11391151.
420. Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G,
Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz
SD, Fox KA, Califf RM; ROCKET AF Investigators. Rivaroxaban versus warfarin
in nonvalvular atrial fibrillation. N Engl J Med 2011;365:883891.
421. Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-
Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz
JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo
AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL,
Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L; ARISTOTLE
Committees and Investigators. Apixaban versus warfarin in patients with atrial
fibrillation. N Engl J Med 2011;365:981992.
422. Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL,
Waldo AL, Ezekowitz MD, Weitz JI, Spinar J, Ruzyllo W, Ruda M, Koretsune Y,
Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM;
ENGAGE AF-TIMI Investigators. Edoxaban versus warfarin in patients with
atrial fibrillation. N Engl J Med 2013;369:20932104.
423. Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz
MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM.
Comparison of the efficacy and safety of new oral anticoagulants with warfarin
in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet
2014;383:955962.
424. Wang KL, Lip GY, Lin SJ, Chiang CE. Non-vitamin K antagonist oral anticoagu-
lants for stroke prevention in Asian patients with nonvalvular atrial fibrillation:
meta-analysis. Stroke 2015;46:25552561.
425. Connolly SJ, Eikelboom J, Joyner C, Diener HC, Hart R, Golitsyn S, Flaker G,
Avezum A, Hohnloser SH, Diaz R, Talajic M, Zhu J, Pais P, Budaj A,
Parkhomenko A, Jansky P, Commerford P, Tan RS, Sim KH, Lewis BS, Van
Mieghem W, Lip GY, Kim JH, Lanas-Zanetti F, Gonzalez-Hermosillo A, Dans
AL, Munawar M, O’Donnell M, Lawrence J, Lewis G, Afzal R, Yusuf S;
AVERROES Steering Committee Investigators. Apixaban in patients with atrial
fibrillation. N Engl J Med 2011;364:806817.
426. Carmo J, Moscoso Costa F, Ferreira J, Mendes M. Dabigatran in real-world atrial
fibrillation. Meta-analysis of observational comparison studies with vitamin K
antagonists. Thromb Haemost 2016;116:754763.
427. Huisman MV, Rothman KJ, Paquette M, Teutsch C, Diener HC, Dubner SJ,
Halperin JL, Ma CS, Zint K, Elsaesser A, Lu S, Bartels DB, Lip GYH; GLORIA-
AF Investigators. Two-year follow-up of patients treated with dabigatran for
stroke prevention in atrial fibrillation: Global Registry on Long-Term
Antithrombotic Treatment in Patients with Atrial Fibrillation (GLORIA-AF)
registry. Am Heart J 2018;198:5563.
428. Camm AJ, Amarenco P, Haas S, Hess S, Kirchhof P, Kuhls S, van Eickels M,
Turpie AG; XANTUS Investigators. XANTUS: a real-world, prospective, obser-
vational study of patients treated with rivaroxaban for stroke prevention in
atrial fibrillation. Eur Heart J
2016;37:11451153.
429. Martinez CAA, Lanas F, Radaideh G, Kharabsheh SM, Lambelet M, Viaud MAL,
Ziadeh NS, Turpie AGG; XANTUS Investigators. XANTUS-EL: a real-world,
prospective, observational study of patients treated with rivaroxaban for stroke
prevention in atrial fibrillation in Eastern Europe, Middle East, Africa and Latin
America. Egypt Heart J 2018;70:307313.
430. Li XS, Deitelzweig S, Keshishian A, Hamilton M, Horblyuk R, Gupta K, Luo X,
Mardekian J, Friend K, Nadkarni A, Pan X, Lip GYH. Effectiveness and safety of
apixaban versus warfarin in non-valvular atrial fibrillation patients in ‘real-world’
clinical practice. A propensity-matched analysis of 76,940 patients. Thromb
Haemost 2017;117:10721082.
431. Lee SR, Choi EK, Han KD, Jung JH, Oh S, Lip GYH. Edoxaban in Asian patients
with atrial fibrillation: effectiveness and safety. J Am Coll Cardiol
2018;72:838853.
432. Ingrasciotta Y, Crisafulli S, Pizzimenti V, Marciano I, Mancuso A, Ando G,
Corrao S, Capranzano P, Trifiro G. Pharmacokinetics of new oral anticoagu-
lants: implications for use in routine care. Expert Opin Drug Metab Toxicol
2018;14:10571069.
433. Chao TF, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP,
Chen TJ, Lip GYH, Chen SA. Oral anticoagulation in very elderly patients with
atrial fibrillation: a nationwide cohort study. Circulation 2018;138:3747.
434. Stanton BE, Barasch NS, Tellor KB. Comparison of the safety and effectiveness
of apixaban versus warfarin in patients with severe renal impairment.
Pharmacotherapy 2017;37:412419.
435. Siontis KC, Zhang X, Eckard A, Bhave N, Schaubel DE, He K, Tilea A, Stack
AG, Balkrishnan R, Yao X, Noseworthy PA, Shah ND, Saran R, Nallamothu BK.
Outcomes associated with apixaban use in patients with end-stage kidney dis-
ease and atrial fibrillation in the United States. Circulation 2018;138:15191529.
436. Steinberg BA, Shrader P, Thomas L, Ansell J, Fonarow GC, Gersh BJ, Kowey
PR, Mahaffey KW, Naccarelli G, Reiffel J, Singer DE, Peterson ED, Piccini JP;
ORBIT-AF Investigators and Patients. Off-label dosing of non-vitamin K antago-
nist oral anticoagulants and adverse outcomes: the ORBIT-AF II registry. JAm
Coll Cardiol 2016;68:25972604.
437. Yao X, Shah ND, Sangaralingham LR, Gersh BJ, Noseworthy PA. Non-vitamin K
antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal
dysfunction. J Am Coll Cardiol 2017;69:27792790.
438. ACTIVE Writing Group of the ACTIVE Investigators, Connolly S, Pogue J, Hart
R, Pfeffer M, Hohnloser S, Chrolavicius S, Pfeffer M, Hohnloser S, Yusuf S.
Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the
Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular
Events (ACTIVE W): a randomised controlled trial. Lancet
2006;367:19031912.
439. ACTIVE Investigators, Connolly SJ, Pogue J, Hart RG, Hohnloser SH, Pfeffer M,
Chrolavicius S, Yusuf S. Effect of clopidogrel added to aspirin in patients with
atrial fibrillation. N Engl J Med 2009;360:20662078.
440. Sjalander S, Sjalander A, Svensson PJ, Friberg L. Atrial fibrillation patients do not
benefit from acetylsalicylic acid. Europace
2014;16:631638.
441. Mant J, Hobbs FD, Fletcher K, Roalfe A, Fitzmaurice D, Lip GY, Murray E;
BAFTA investigators, Midland Research Practices Network (MidReC). Warfarin
versus aspirin for stroke prevention in an elderly community population with
atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged
Study, BAFTA): a randomised controlled trial. Lancet 2007;370:493503.
442. Lip GY. The role of aspirin for stroke prevention in atrial fibrillation. Nat Rev
Cardiol 2011;8:602606.
96 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
443. Verheugt FWA, Gao H, Al Mahmeed W, Ambrosio G, Angchaisuksiri P, Atar
D, Bassand JP, Camm AJ, Cools F, Eikelboom J, Kayani G, Lim TW, Misselwitz F,
Pieper KS, van Eickels M, Kakkar AK; GARFIELD-AF Investigators.
Characteristics of patients with atrial fibrillation prescribed antiplatelet mono-
therapy compared with those on anticoagulants: insights from the GARFIELD-
AF registry. Eur Heart J 2018;39:464473.
444. Holmes DR, Reddy VY, Turi ZG, Doshi SK, Sievert H, Buchbinder M, Mullin
CM, Sick P; PROTECT AF Investigators. Percutaneous closure of the left atrial
appendage versus warfarin therapy for prevention of stroke in patients with
atrial fibrillation: a randomised non-inferiority trial. Lancet 2009;374:534542.
445. Reddy VY, Doshi SK, Sievert H, Buchbinder M, Neuzil P, Huber K, Halperin JL,
Holmes D; PROTECT AF Investigators. Percutaneous left atrial appendage clo-
sure for stroke prophylaxis in patients with atrial fibrillation: 2.3-year follow-up
of the PROTECT AF (Watchman Left Atrial Appendage System for Embolic
Protection in Patients with Atrial Fibrillation) trial. Circulation
2013;127:720729.
446. Holmes DR Jr, Kar S, Price MJ, Whisenant B, Sievert H, Doshi SK, Huber K,
Reddy VY. Prospective randomized evaluation of the Watchman left atrial
appendage closure device in patients with atrial fibrillation versus long-term
warfarin therapy: the PREVAIL trial. J Am Coll Cardiol 2014;64:112.
447. Holmes DR, Jr., Doshi SK, Kar S, Price MJ, Sanchez JM, Sievert H, Valderrabano
M, Reddy VY. Left atrial appendage closure as an alternative to warfarin for
stroke prevention in atrial fibrillation: a patient-level meta-analysis. J Am Coll
Cardiol 2015;65:26142623.
448. Reddy VY, Mobius-Winkler S, Miller MA, Neuzil P, Schuler G, Wiebe J, Sick P,
Sievert H. Left atrial appendage closure with the Watchman device in patients
with a contraindication for oral anticoagulation: the ASAP study (ASA Plavix
Feasibility Study With Watchman Left Atrial Appendage Closure Technology). J
Am Coll Cardiol 2013;61:25512556.
449. Boersma LV, Schmidt B, Betts TR, Sievert H, Tamburino C, Teiger E,
Pokushalov E, Kische S, Schmitz T, Stein KM, Bergmann MW, on behalf of the
EWOLUTION investigators. Implant success and safety of left atrial appendage
closure with the WATCHMAN device: peri-procedural outcomes from the
EWOLUTION registry. Eur Heart J 2016;37:24652474.
450. Boersma LV, Ince H, Kische S, Pokushalov E, Schmitz T, Schmidt B, Gori T,
Meincke F, Protopopov AV, Betts T, Foley D, Sievert H, Mazzone P, De Potter
T, Vireca E, Stein K, Bergmann MW, for the EWOLUTION Investigators.
Efficacy and safety of left atrial appendage closure with WATCHMAN in
patients with or without contraindication to oral anticoagulation: 1-year follow-
up outcome data of the EWOLUTION trial. Heart Rhythm
2017;14:13021308.
451. Badheka AO, Chothani A, Mehta K, Patel NJ, Deshmukh A, Hoosien M, Shah
N, Singh V, Grover P, Savani GT, Panaich SS, Rathod A, Patel N, Arora S,
Bhalara V, Coffey JO, O’Neill W, Makkar R, Grines CL, Schreiber T, Di Biase L,
Natale A, Viles-Gonzalez JF. Utilization and adverse outcomes of percutaneous
left atrial appendage closure for stroke prevention in atrial fibrillation in the
United States: influence of hospital volume. Circ Arrhythm Electrophysiol
2015;8:4248.
452. Pison L, Potpara TS, Chen J, Larsen TB, Bongiorni MG, Blomstrom-Lundqvist C;
Scientific Initiative Committee EHRA. Left atrial appendage closure-indications,
techniques, and outcomes: results of the European Heart Rhythm Association
Survey. Europace 2015;17:642646.
453. Price MJ, Gibson DN, Yakubov SJ, Schultz JC, Di Biase L, Natale A, Burkhardt
JD, Pershad A, Byrne TJ, Gidney B, Aragon JR, Goldstein J, Moulton K, Patel T,
Knight B, Lin AC, Valderrabano M. Early safety and efficacy of percutaneous left
atrial appendage suture ligation: results from the US transcatheter LAA ligation
consortium. J Am Coll Cardiol 2014;64:565572.
454. Fauchier L, Cinaud A, Brigadeau F, Lepillier A, Pierre B, Abbey S, Fatemi M,
Franceschi F, Guedeney P, Jacon P, Paziaud O, Venier S, Deharo JC, Gras D,
Klug D, Mansourati J, Montalescot G, Piot O, Defaye P. Device-related throm-
bosis after percutaneous left atrial appendage occlusion for atrial fibrillation. J
Am Coll Cardiol 2018;71:15281536.
455. Lakkireddy D, Afzal MR, Lee RJ, Nagaraj H, Tschopp D, Gidney B, Ellis C,
Altman E, Lee B, Kar S, Bhadwar N, Sanchez M, Gadiyaram V, Evonich R,
Rasekh A, Cheng J, Cuoco F, Chandhok S, Gunda S, Reddy M, Atkins D,
Bommana S, Cuculich P, Gibson D, Nath J, Ferrell R, Matthew E, Wilber D.
Short and long-term outcomes of percutaneous left atrial appendage suture
ligation: results from a US multicenter evaluation. Heart Rhythm
2016;13:10301036.
456. van Laar C, Verberkmoes NJ, van Es HW, Lewalter T, Dunnington G, Stark S,
Longoria J, Hofman FH, Pierce CM, Kotecha D, van Putte BP. Thoracoscopic
left atrial appendage clipping: a multicenter cohort analysis. JACC Clin
Electrophysiol 2018;4:893901.
457. Healey JS, Crystal E, Lamy A, Teoh K, Semelhago L, Hohnloser SH, Cybulsky I,
Abouzahr L, Sawchuck C, Carroll S, Morillo C, Kleine P, Chu V, Lonn E,
Connolly SJ. Left Atrial Appendage Occlusion Study (LAAOS): results of a
randomized controlled pilot study of left atrial appendage occlusion during cor-
onary bypass surgery in patients at risk for stroke. Am Heart J
2005;150:288293.
458. Whitlock RP, Vincent J, Blackall MH, Hirsh J, Fremes S, Novick R, Devereaux PJ,
Teoh K, Lamy A, Connolly SJ, Yusuf S, Carrier M, Healey JS. Left Atrial
Appendage Occlusion Study II (LAAOS II). Can J Cardiol 2013;29:14431447.
459. Tsai YC, Phan K, Munkholm-Larsen S, Tian DH, La Meir M, Yan TD. Surgical
left atrial appendage occlusion during cardiac surgery for patients with atrial
fibrillation: a meta-analysis. Eur J Cardiothorac Surg 2015;47:847854.
460. Aryana A, Singh SK, Singh SM, O’Neill PG, Bowers MR, Allen SL, Lewandowski
SL, Vierra EC, d’Avila A. Association between incomplete surgical ligation of left
atrial appendage and stroke and systemic embolization. Heart Rhythm
2015;12:14311437.
461. Gillinov AM, Gelijns AC, Parides MK, DeRose JJ Jr, Moskowitz AJ, Voisine P,
Ailawadi G, Bouchard D, Smith PK, Mack MJ, Acker MA, Mullen JC, Rose EA,
Chang HL, Puskas JD, Couderc JP, Gardner TJ, Varghese R, Horvath KA, Bolling
SF, Michler RE, Geller NL, Ascheim DD, Miller MA, Bagiella E, Moquete EG,
Williams P, Taddei-Peters WC, O’Gara PT, Blackstone EH, Argenziano M;
CTSN Investigators. Surgical ablation of atrial fibrillation during mitral-valve sur-
gery. N Engl J Med 2015;372:13991409.
462. Whitlock R, Healey J, Vincent J, Brady K, Teoh K, Royse A, Shah P, Guo Y,
Alings M, Folkeringa RJ, Paparella D, Colli A, Meyer SR, Legare JF, Lamontagne
F, Reents W, Boning A, Connolly S. Rationale and design of the Left Atrial
Appendage Occlusion Study (LAAOS) III. Ann Cardiothorac Surg 2014;3:4554.
463. Nielsen PB, Skjoth F, Sogaard M, Kjaeldgaard JN, Lip GY, Larsen TB.
Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoa-
gulants and warfarin in patients with atrial fibrillation: propensity weighted
nationwide cohort study. BMJ 2017;356:j510.
464. Larsen TB, Skjoth F, Nielsen PB, Kjaeldgaard JN, Lip GY. Comparative effective-
ness and safety of non-vitamin K antagonist oral anticoagulants and warfarin in
patients with atrial fibrillation: propensity weighted nationwide cohort study.
BMJ 2016;
353:i3189.
465. Tilz RR, Potpara T, Chen J, Dobreanu D, Larsen TB, Haugaa KH, Dagres N. Left
atrial appendage occluder implantation in Europe: indications and anticoagula-
tion post-implantation. Results of the European Heart Rhythm Association
Survey. Europace 2017;19:17371742.
466. Ogawa H, An Y, Ikeda S, Aono Y, Doi K, Ishii M, Iguchi M, Masunaga N, Esato
M, Tsuji H, Wada H, Hasegawa K, Abe M, Lip GYH, Akao M; Fushimi AF
Registry Investigators. Progression from paroxysmal to sustained atrial fibrilla-
tion is associated with increased adverse events. Stroke 2018;49:23012308.
467. Mahajan R, Perera T, Elliott AD, Twomey DJ, Kumar S, Munwar DA, Khokhar
KB, Thiyagarajah A, Middeldorp ME, Nalliah CJ, Hendriks JML, Kalman JM, Lau
DH, Sanders P. Subclinical device-detected atrial fibrillation and stroke risk: a
systematic review and meta-analysis. Eur Heart J 2018;39:14071415.
468. Van Gelder IC, Healey JS, Crijns H, Wang J, Hohnloser SH, Gold MR, Capucci
A, Lau CP, Morillo CA, Hobbelt AH, Rienstra M, Connolly SJ. Duration of
device-detected subclinical atrial fibrillation and occurrence of stroke in
ASSERT. Eur Heart J 2017;38:13391344.
469. Boriani G, Glotzer TV, Ziegler PD, De Melis M, Mangoni di SSL, Sepsi M,
Landolina M, Lunati M, Lewalter T, Camm AJ. Detection of new atrial fibrillation
in patients with cardiac implanted electronic devices and factors associated
with transition to higher device-detected atrial fibrillation burden. Heart Rhythm
2018;15:376383.
470. Pastori D, Lip GYH, Farcomeni A, Del Sole F, Sciacqua A, Perticone F, Marcucci
R, Grifoni E, Pignatelli P, Violi F, ATHERO-AF study group. Incidence of bleed-
ing in patients with atrial fibrillation and advanced liver fibrosis on treatment
with vitamin K or non-vitamin K antagonist oral anticoagulants. Int J Cardiol
2018;264:5863.
471. Kuo L, Chao TF, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN,
Chung FP, Chen TJ, Lip GYH, Chen SA. Liver cirrhosis in patients with atrial
fibrillation: would oral anticoagulation have a net clinical benefit for stroke
prevention?J Am Heart Assoc 2017;6.
472. Lee SR, Lee HJ, Choi EK, Han KD, Jung JH, Cha MJ, Oh S, Lip GYH. Direct oral
anticoagulants in patients with atrial fibrillation and liver disease. J Am Coll
Cardiol 2019;73:32953308.
473. Staerk L, Lip GY, Olesen JB, Fosbol EL, Pallisgaard JL, Bonde AN, Gundlund A,
Lindhardt TB, Hansen ML, Torp-Pedersen C, Gislason GH. Stroke and recur-
rent haemorrhage associated with antithrombotic treatment after gastrointesti-
nal bleeding in patients with atrial fibrillation: nationwide cohort study. BMJ
2015;351:h5876.
474. Eckman MH, Singer DE, Rosand J, Greenberg SM. Moving the tipping point: the
decision to anticoagulate patients with atrial fibrillation. Circ Cardiovasc Qual
Outcomes 2011;4:1421.
475. Proietti M, Lip GY. Major outcomes in atrial fibrillation patients with one risk
factor: impact of time in therapeutic range observations from the SPORTIF tri-
als. Am J Med 2016;129:11101116.
ESC Guidelines 97

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
476. Lip GY, Nielsen PB. Should patients with atrial fibrillation and 1 stroke risk fac-
tor (CHA2DS2-VASc Score 1 in Men, 2 in Women) be anticoagulated? Yes:
even 1 stroke risk factor confers a real risk of stroke. Circulation
2016;133:14981503; discussion 1503.
477. Lip GY, Lane DA. Stroke prevention in atrial fibrillation: a systematic review.
JAMA 2015;313:19501962.
478. Hijazi Z, Hohnloser SH, Andersson U, Alexander JH, Hanna M, Keltai M,
Parkhomenko A, Lopez-Sendon JL, Lopes RD, Siegbahn A, Granger CB,
Wallentin L. Efficacy and safety of apixaban compared with warfarin in patients
with atrial fibrillation in relation to renal function over time: insights from the
ARISTOTLE randomized clinical trial. JAMA Cardiol 2016;1:451460.
479. Bohm M, Ezekowitz MD, Connolly SJ, Eikelboom JW, Hohnloser SH, Reilly PA,
Schumacher H, Brueckmann M, Schirmer SH, Kratz MT, Yusuf S, Diener HC,
Hijazi Z, Wallentin L. Changes in renal function in patients with atrial fibrillation:
an analysis from the RE-LY trial. J Am Coll Cardiol 2015;65:24812493.
480. Clarkesmith DE, Pattison HM, Lip GY, Lane DA. Educational intervention
improves anticoagulation control in atrial fibrillation patients: the TREAT rando-
mised trial. PLoS One 2013;8:e74037.
481. Teiger E, Thambo JB, Defaye P, Hermida JS, Abbey S, Klug D, Juliard JM, Pasquie
JL, Rioufol G, Lepillier A, Elbaz M, Horvilleur J, Brenot P, Pierre B, Le
Corvoisier P. Percutaneous left atrial appendage closure is a reasonable option
for patients with atrial fibrillation at high risk for cerebrovascular events. Circ
Cardiovasc Interv 2018;11:e005841.
482. Saw J, Fahmy P, Azzalini L, Marquis JF, Hibbert B, Morillo C, Carrizo A, Ibrahim
R. Early Canadian multicenter experience with WATCHMAN for percutaneous
left atrial appendage closure. J Cardiovasc Electrophysiol 2017;28:396401.
483. Martin Gutierrez E, Castano M, Gualis J, Martinez-Comendador JM, Maiorano P,
Castillo L, Laguna G. Beneficial effect of left atrial appendage closure during car-
diac surgery: a meta-analysis of 280 585 patients. Eur J Cardiothorac Surg
2020;57:252262.
484. Al-Khatib SM, Allen LaPointe NM, Chatterjee R, Crowley MJ, Dupre ME, Kong
DF, Lopes RD, Povsic TJ, Raju SS, Shah B, Kosinski AS, McBroom AJ, Sanders
GD. Rate- and rhythm-control therapies in patients with atrial fibrillation: a sys-
tematic review. Ann Intern Med 2014;160:760773.
485. Tamariz LJ, Bass EB. Pharmacological rate control of atrial fibrillation. Cardiol
Clin 2004;22:35 45.
486. Nikolaidou T, Channer KS. Chronic atrial fibrillation: a systematic review of
medical heart rate control management. Postgrad Med J 2009;85:303312.
487. Groenveld HF, Crijns HJ, Van den Berg MP, Van Sonderen E, Alings AM, Tijssen
JG, Hillege HL, Tuininga YS, Van Veldhuisen DJ, Ranchor AV, Van Gelder IC;
RACE II Investigators. The effect of rate control on quality of life in patients
with permanent atrial fibrillation: data from the RACE II (Rate Control Efficacy
in Permanent Atrial Fibrillation II) study. J Am Coll Cardiol 2011;58:17951803.
488. Van Gelder IC, Groenveld HF, Crijns HJ, Tuininga YS, Tijssen JG, Alings AM,
Hillege HL, Bergsma-Kadijk JA, Cornel JH, Kamp O, Tukkie R, Bosker HA, Van
Veldhuisen DJ, Van den Berg MP; RACE II Investigators. Lenient versus strict
rate control in patients with atrial fibrillation. N Engl J Med
2010;362:13631373.
489. Van Gelder IC, Wyse DG, Chandler ML, Cooper HA, Olshansky B, Hagens VE,
Crijns HJ; RACE and AFFIRM Investigators. Does intensity of rate-control influ-
ence outcome in atrial fibrillation? An analysis of pooled data from the RACE
and AFFIRM studies. Europace 2006;8:935942.
490. Van Gelder IC, Rienstra M, Crijns HJ, Olshansky B. Rate control in atrial fibrilla-
tion. Lancet 2016;388:818828.
491. Kotecha D, Holmes J, Krum H, Altman DG, Manzano L, Cleland JG, Lip GY,
Coats AJ, Andersson B, Kirchhof P, von Lueder TG, Wedel H, Rosano G,
Shibata MC, Rigby A, Flather MD. Efficacy of beta blockers in patients with
heart failure plus atrial fibrillation: an individual-patient data meta-analysis.
Lancet 2014;384:22352243.
492. Ulimoen SR, Enger S, Carlson J, Platonov PG, Pripp AH, Abdelnoor M, Arnesen
H, Gjesdal K, Tveit A. Comparison of four single-drug regimens on ventricular
rate and arrhythmia-related symptoms in patients with permanent atrial fibrilla-
tion. Am J Cardiol 2013;111:225230.
493. Ulimoen SR, Enger S, Pripp AH, Abdelnoor M, Arnesen H, Gjesdal K, Tveit A.
Calcium channel blockers improve exercise capacity and reduce N-terminal
Pro-B-type natriuretic peptide levels compared with beta-blockers in patients
with permanent atrial fibrillation. Eur Heart J 2014;35:517524.
494. Figulla HR, Gietzen F, Zeymer U, Raiber M, Hegselmann J, Soballa R, Hilgers R.
Diltiazem improves cardiac function and exercise capacity in patients with idio-
pathic dilated cardiomyopathy. Results of the Diltiazem in Dilated
Cardiomyopathy trial. Circulation 1996;94:346352.
495. Hallberg P, Lindback J, Lindahl B, Stenestrand U, Melhus H, group R-H. Digoxin
and mortality in atrial fibrillation: a prospective cohort study. Eur J Clin
Pharmacol 2007;63:959971.
496. Turakhia MP, Santangeli P, Winkelmayer WC, Xu X, Ullal AJ, Than CT, Schmitt
S, Holmes TH, Frayne SM, Phibbs CS, Yang F, Hoang DD, Ho PM, Heidenreich
PA. Increased mortality associated with digoxin in contemporary patients with
atrial fibrillation: findings from the TREAT-AF study. J Am Coll Cardiol
2014;64:660668.
497. Whitbeck MG, Charnigo RJ, Khairy P, Ziada K, Bailey AL, Zegarra MM, Shah J,
Morales G, Macaulay T, Sorrell VL, Campbell CL, Gurley J, Anaya P, Nasr H, Bai
R, Di Biase L, Booth DC, Jondeau G, Natale A, Roy D, Smyth S, Moliterno DJ,
Elayi CS. Increased mortality among patients taking digoxin analysis from the
AFFIRM study. Eur Heart J 2013;34:14811488.
498. Andrey JL, Romero S, Garcia-Egido A, Escobar MA, Corzo R, Garcia-
Dominguez G, Lechuga V, Gomez F. Mortality and morbidity of heart failure
treated with digoxin. A propensity-matched study. Int J Clin Pract
2011;65:12501258.
499. Flory JH, Ky B, Haynes K, S MB, Munson J, Rowan, C, Strom BL, Hennessy S.
Observational cohort study of the safety of digoxin use in women with heart
failure. BMJ Open 2012;
2:e000888.
500. Gheorghiade M, Fonarow GC, van Veldhuisen DJ, Cleland JG, Butler J, Epstein
AE, Patel K, Aban IB, Aronow WS, Anker SD, Ahmed A. Lack of evidence of
increased mortality among patients with atrial fibrillation taking digoxin: findings
from post hoc propensity-matched analysis of the AFFIRM trial. Eur Heart J
2013;34:14891497.
501. Aguirre Davila L, Weber K, Bavendiek U, Bauersachs J, Wittes J, Yusuf S, Koch
A. Digoxin-mortality: randomized vs. observational comparison in the DIG trial.
Eur Heart J 2019;40:33363341.
502. Ziff OJ, Lane DA, Samra M, Griffith M, Kirchhof P, Lip GY, Steeds RP, Townend
J, Kotecha D. Safety and efficacy of digoxin: systematic review and meta-analysis
of observational and controlled trial data. BMJ 2015;351:h4451.
503. Bavendiek U, Berliner D, Davila LA, Schwab J, Maier L, Philipp SA, Rieth A,
Westenfeld R, Piorkowski C, Weber K, Hanselmann A, Oldhafer M, Schallhorn
S, von der Leyen H, Schroder C, Veltmann C, Stork S, Bohm M, Koch A,
Bauersachs J; DIGIT-HF Investigators and Committees. Rationale and design of
the DIGIT-HF trial (DIGitoxin to Improve ouTcomes in patients with advanced
chronic Heart Failure): a randomized, double-blind, placebo-controlled study.
Eur J Heart Fail 2019;21:676684.
504. Clemo HF, Wood MA, Gilligan DM, Ellenbogen KA. Intravenous amiodarone
for acute heart rate control in the critically ill patient with atrial tachyarrhyth-
mias. Am J Cardiol 1998;81:594598.
505. Klijn CJ, Paciaroni M, Berge E, Korompoki E, Korv J, Lal A, Putaala J, Werring
DJ. Antithrombotic treatment for secondary prevention of stroke and other
thromboembolic events in patients with stroke or transient ischemic attack and
non-valvular atrial fibrillation: a European Stroke Organisation guideline. Eur
Stroke J 2019;4:198223.
506. Gosselink AT, Crijns HJ, Van Gelder IC, Hillige H, Wiesfeld AC, Lie KI. Low-
dose amiodarone for maintenance of sinus rhythm after cardioversion of atrial
fibrillation or flutter. JAMA 1992;267:32893293.
507. Scheuermeyer FX, Grafstein E, Stenstrom R, Christenson J, Heslop C, Heilbron
B, McGrath L, Innes G. Safety and efficiency of calcium channel blockers versus
beta-blockers for rate control in patients with atrial fibrillation and no acute
underlying medical illness. Acad Emerg Med 2013;20:222230.
508. Schreck DM, Rivera AR, Tricarico VJ. Emergency management of atrial fibrilla-
tion and flutter: intravenous diltiazem versus intravenous digoxin. Ann Emerg
Med 1997;29:135140.
509. Segal JB, McNamara RL, Miller MR, Kim N, Goodman SN, Powe NR, Robinson
K, Yu D, Bass EB. The evidence regarding the drugs used for ventricular rate
control. J Fam Pract 2000;49:4759.
510. Siu CW, Lau CP, Lee WL, Lam KF, Tse HF. Intravenous diltiazem is superior to
intravenous amiodarone or digoxin for achieving ventricular rate control in
patients with acute uncomplicated atrial fibrillation. Crit Care Med
2009;37:21742179; quiz 2180.
511. Tisdale JE, Padhi ID, Goldberg AD, Silverman NA, Webb CR, Higgins RS, Paone
G, Frank DM, Borzak S. A randomized, double-blind comparison of intravenous
diltiazem and digoxin for atrial fibrillation after coronary artery bypass surgery.
Am Heart J 1998;135:739
747.
512. Darby AE, Dimarco JP. Management of atrial fibrillation in patients with struc-
tural heart disease. Circulation 2012;125:945957.
513. Kotecha D, Piccini JP. Atrial fibrillation in heart failure: what should we do?Eur
Heart J 2015;36:32503257.
514. Delle Karth G, Geppert A, Neunteufl T, Priglinger U, Haumer M,
Gschwandtner M, Siostrzonek P, Heinz G. Amiodarone versus diltiazem for
rate control in critically ill patients with atrial tachyarrhythmias. Crit Care Med
2001;29:11491153.
515. Hou ZY, Chang MS, Chen CY, Tu MS, Lin SL, Chiang HT, Woosley RL. Acute
treatment of recent-onset atrial fibrillation and flutter with a tailored dosing
regimen of intravenous amiodarone. A randomized, digoxin-controlled study.
Eur Heart J 1995;16:521528.
98 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
516. Lim KT, Davis MJ, Powell A, Arnolda L, Moulden K, Bulsara M, Weerasooriya R.
Ablate and pace strategy for atrial fibrillation: long-term outcome of AIRCRAFT
trial. Europace 2007;9:498505.
517. Queiroga A, Marshall HJ, Clune M, Gammage MD. Ablate and pace revisited:
long term survival and predictors of permanent atrial fibrillation. Heart
2003;89:10351038.
518. Geelen P, Brugada J, Andries E, Brugada P. Ventricular fibrillation and sudden
death after radiofrequency catheter ablation of the atrioventricular junction.
Pacing Clin Electrophysiol 1997;20:343348.
519. Wang RX, Lee HC, Hodge DO, Cha YM, Friedman PA, Rea RF, Munger
TM, Jahangir A, Srivathsan K, Shen WK. Effect of pacing method on risk
of sudden death after atrioventricular node ablation and pacemaker
implantation in patients with atrial fibrillation. Heart Rhythm
2013;10:696701.
520. Chatterjee NA, Upadhyay GA, Ellenbogen KA, McAlister FA, Choudhry NK,
Singh JP. Atrioventricular nodal ablation in atrial fibrillation: a meta-analysis and
systematic review. Circ Arrhythm Electrophysiol 2012;5:6876.
521. Bradley DJ, Shen WK. Overview of management of atrial fibrillation in sympto-
matic elderly patients: pharmacologic therapy versus AV node ablation. Clin
Pharmacol Ther 2007;81:284287.
522. Ozcan C, Jahangir A, Friedman PA, Patel PJ, Munger TM, Rea RF, Lloyd MA,
Packer DL, Hodge DO, Gersh BJ, Hammill SC, Shen WK. Long-term survival
after ablation of the atrioventricular node and implantation of a permanent
pacemaker in patients with atrial fibrillation. N Engl J Med
2001;344:10431051.
523. Wood MA, Brown-Mahoney C, Kay GN, Ellenbogen KA. Clinical outcomes
after ablation and pacing therapy for atrial fibrillation: a meta-analysis. Circulation
2000;101:11381144.
524. Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt
OA, Cleland J, Deharo JC, Delgado V, Elliott PM, Gorenek B, Israel CW,
Leclercq C, Linde C, Mont L, Padeletti L, Sutton R, Vardas PE, ESC Committee
for Practice Guidelines, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ,
Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW,
Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P,
Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns
W, Windecker S, Document R, Kirchhof P, Blomstrom-Lundqvist C, Badano
LP, Aliyev F, Bansch D, Baumgartner H, Bsata W, Buser P, Charron P, Daubert
JC, Dobreanu D, Faerestrand S, Hasdai D, Hoes AW, Le Heuzey JY, Mavrakis
H, McDonagh T, Merino JL, Nawar MM, Nielsen JC, Pieske B, Poposka L,
Ruschitzka F, Tendera M, Van Gelder IC, Wilson CM. 2013 ESC Guidelines on
cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac
pacing and resynchronization therapy of the European Society of Cardiology
(ESC). Developed in collaboration with the European Heart Rhythm
Association (EHRA). Eur Heart J 2013;34:22812329.
525. Chatterjee NA, Upadhyay GA, Ellenbogen KA, Hayes DL, Singh JP.
Atrioventricular nodal ablation in atrial fibrillation: a meta-analysis of biven-
tricular vs. right ventricular pacing mode. Eur J Heart Fail
2012;14:661667.
526. Huang W, Su L, Wu S. Pacing treatment of atrial fibrillation patients with heart
failure: His bundle pacing combined with atrioventricular node ablation. Card
Electrophysiol Clin 2018;10:519535.
527. Brignole M, Pokushalov E, Pentimalli F, Palmisano P, Chieffo E, Occhetta E,
Quartieri F, Calo L, Ungar A, Mont L; APAF-CRT Investigators. A randomized
controlled trial of atrioventricular junction ablation and cardiac resynchroniza-
tion therapy in patients with permanent atrial fibrillation and narrow QRS.
Eur
Heart J 2018;39:39994008.
528. Huang W, Su L, Wu S, Xu L, Xiao F, Zhou X, Ellenbogen KA. Benefits of per-
manent His bundle pacing combined with atrioventricular node ablation in atrial
fibrillation patients with heart failure with both preserved and reduced left ven-
tricular ejection fraction. J Am Heart Assoc 2017;6.
529. Farshi R, Kistner D, Sarma JS, Longmate JA, Singh BN. Ventricular rate control
in chronic atrial fibrillation during daily activity and programmed exercise: a
crossover open-label study of five drug regimens. J Am Coll Cardiol
1999;33:304310.
530. Khand AU, Rankin AC, Martin W, Taylor J, Gemmell I, Cleland JG. Carvedilol
alone or in combination with digoxin for the management of atrial fibrillation in
patients with heart failure?J Am Coll Cardiol 2003;42:19441951.
531. Lewis RV, Irvine N, McDevitt DG. Relationships between heart rate, exercise
tolerance and cardiac output in atrial fibrillation: the effects of treatment with
digoxin, verapamil and diltiazem. Eur Heart J 1988;9:777781.
532. Mulder BA, Van Veldhuisen DJ, Crijns HJ, Tijssen JG, Hillege HL, Alings M,
Rienstra M, Van den Berg MP, Van Gelder IC. Digoxin in patients with perma-
nent atrial fibrillation: data from the RACE II study. Heart Rhythm
2014;11:15431550.
533. Roth A, Harrison E, Mitani G, Cohen J, Rahimtoola SH, Elkayam U. Efficacy and
safety of medium- and high-dose diltiazem alone and in combination with
digoxin for control of heart rate at rest and during exercise in patients with
chronic atrial fibrillation. Circulation 1986;73:316324.
534. David D, Segni ED, Klein HO, Kaplinsky E. Inefficacy of digitalis in the control of
heart rate in patients with chronic atrial fibrillation: beneficial effect of an added
beta adrenergic blocking agent. Am J Cardiol 1979;44:13781382.
535. Weerasooriya R, Davis M, Powell A, Szili-Torok T, Shah C, Whalley D,
Kanagaratnam L, Heddle W, Leitch J, Perks A, Ferguson L, Bulsara M. The
Australian Intervention Randomized Control of Rate in Atrial Fibrillation Trial
(AIRCRAFT). J Am Coll Cardiol 2003;41:16971702.
536. Vijayaraman P, Subzposh FA, Naperkowski A. Atrioventricular node ablation
and His bundle pacing. Europace 2017;19:iv10iv16.
537. Shiga T, Yoshioka K, Watanabe E, Omori H, Yagi M, Okumura Y, Matsumoto
N, Kusano K, Oshiro C, Ikeda T, Takahashi N, Komatsu T, Suzuki A, Suzuki T,
Sato Y, Yamashita T; AF-QOL study investigators. Paroxysmal atrial fibrillation
recurrences and quality of life in symptomatic patients: a crossover study of fle-
cainide and pilsicainide. J Arrhythm 2017;33:310317.
538. Capucci A, Piangerelli L, Ricciotti J, Gabrielli D, Guerra F. Flecainide-metoprolol
combination reduces atrial fibrillation clinical recurrences and improves toler-
ability at 1-year follow-up in persistent symptomatic atrial fibrillation. Europace
2016;18:1698
1704.
539. Shi LZ, Heng R, Liu SM, Leng FY. Effect of catheter ablation versus antiarrhyth-
mic drugs on atrial fibrillation: a meta-analysis of randomized controlled trials.
Exp Ther Med 2015;10:816822.
540. Siontis KC, Ioannidis JPA, Katritsis GD, Noseworthy PA, Packer DL, Hummel
JD, Jais P, Krittayaphong R, Mont L, Morillo CA, Nielsen JC, Oral H, Pappone C,
Santinelli V, Weerasooriya R, Wilber DJ, Gersh BJ, Josephson ME, Katritsis DG.
Radiofrequency ablation versus antiarrhythmic drug therapy for atrial fibrilla-
tion: meta-analysis of quality of life, morbidity, and mortality. JACC Clin
Electrophysiol 2016;2:170180.
541. Kim YG, Shim J, Choi JI, Kim YH. Radiofrequency catheter ablation improves
the quality of life measured with a short form-36 questionnaire in atrial fibrilla-
tion patients: a systematic review and meta-analysis. PLoS One
2016;11:e0163755.
542. Bayes de Luna A, Platonov P, Cosio FG, Cygankiewicz I, Pastore C, Baranowski
R, Bayes-Genis A, Guindo J, Vinolas X, Garcia-Niebla J, Barbosa R, Stern S,
Spodick D. Interatrial blocks. A separate entity from left atrial enlargement: a
consensus report. J Electrocardiol 2012;45:445451.
543. Jadidi A, Muller-Edenborn B, Chen J, Keyl C, Weber R, Allgeier J, Moreno-
Weidmann Z, Trenk D, Neumann FJ, Lehrmann H, Arentz T. The duration of
the amplified sinus-p-wave identifies presence of left atrial low voltage substrate
and predicts outcome after pulmonary vein isolation in patients with persistent
atrial fibrillation. JACC Clin Electrophysiol 2018;4:531543.
544. Dudink E, Erkuner O, Berg J, Nieuwlaat R, de Vos CB, Weijs B, Capucci A,
Camm AJ, Breithardt G, Le Heuzey JY, Luermans J, Crijns H. The influence of
progression of atrial fibrillation on quality of life: a report from the Euro Heart
Survey. Europace 2018;20:929934.
545. Zhang YY, Qiu C, Davis PJ, Jhaveri M, Prystowsky EN, Kowey P, Weintraub
WS. Predictors of progression of recently diagnosed atrial fibrillation in
REgistry on Cardiac Rhythm DisORDers Assessing the Control of Atrial
Fibrillation (RecordAF) United States cohort. Am J Cardiol 2013;112:7984.
546. Bunch TJ, May HT, Bair TL, Johnson DL, Weiss JP, Crandall BG, Osborn JS,
Anderson JL, Muhlestein JB, Lappe DL, Day JD. Increasing time between first
diagnosis of atrial fibrillation and catheter ablation adversely affects long-term
outcomes. Heart Rhythm 2013;10:12571262.
547. Andrade JG, Champagne J, Deyell MW, Essebag V, Lauck S, Morillo C, Sapp J,
Skanes A, Theoret-Patrick P, Wells GA, Verma A; EARLY-AF Study
Investigators. A randomized clinical trial of early invasive intervention for atrial
fibrillation (EARLY-AF) methods and rationale. Am Heart J
2018;206:94104.
548. Teh AW, Kistler PM, Lee G, Medi C, Heck PM, Spence SJ, Morton JB, Sanders
P, Kalman JM. Long-term effects of catheter ablation for lone atrial fibrillation:
progressive atrial electroanatomic substrate remodeling despite successful abla-
tion. Heart Rhythm 2012;9:473480.
549. Aliot E, Brandes A, Eckardt L, Elvan A, Gulizia M, Heidbuchel H, Kautzner J,
Mont L, Morgan J, Ng A, Szumowski L, Themistoclakis S, Van Gelder IC,
Willems S, Kirchhof P. The EAST study: redefining the role of rhythmcontrol
therapy in atrial fibrillation: EAST, the Early treatment of Atrial fibrillation for
Stroke prevention Trial. Eur Heart J 2015;36:255256.
550. Michelena HI, Powell BD, Brady PA, Friedman PA, Ezekowitz MD. Gender in
atrial fibrillation: ten years later. Gend Med 2010;7
:206217.
551. Sethi NJ, Feinberg J, Nielsen EE, Safi S, Gluud C, Jakobsen JC. The effects of
rhythm control strategies versus rate control strategies for atrial fibrillation and
atrial flutter: a systematic review with meta-analysis and trial sequential analysis.
PLoS One 2017;12:e0186856.
552. Ha AC, Breithardt G, Camm AJ, Crijns HJ, Fitzmaurice GM, Kowey PR, Le
Heuzey JY, Naditch-Brule L, Prystowsky EN, Schwartz PJ, Torp-Pedersen C,
ESC Guidelines 99

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Weintraub WS, Dorian P. Health-related quality of life in patients with atrial
fibrillation treated with rhythm control versus rate control: insights from a pro-
spective international registry (Registry on Cardiac Rhythm Disorders Assessing
the Control of Atrial Fibrillation: RECORD-AF). Circ Cardiovasc Qual Outcomes
2014;7:896904.
553. Bulkova V, Fiala M, Havranek S, Simek J, Sknouril L, Januska J, Spinar J,
Wichterle D. Improvement in quality of life after catheter ablation for paroxys-
mal versus long-standing persistent atrial fibrillation: a prospective study with 3-
year follow-up. J Am Heart Assoc 2014;3.
554. Kirchhof P, Monnig G, Wasmer K, Heinecke A, Breithardt G, Eckardt L, Bocker
D. A trial of self-adhesive patch electrodes and hand-held paddle electrodes for
external cardioversion of atrial fibrillation (MOBIPAPA). Eur Heart J
2005;26:12921297.
555. Kirchhof P, Eckardt L, Loh P, Weber K, Fischer RJ, Seidl KH, Bocker D,
Breithardt G, Haverkamp W, Borggrefe M. Anterior-posterior versus anterior-
lateral electrode positions for external cardioversion of atrial fibrillation: a rand-
omised trial. Lancet 2002;360:12751279.
556. Um KJ, McIntyre WF, Healey JS, Mendoza PA, Koziarz A, Amit G, Chu VA,
Whitlock RP, Belley-Cote EP. Pre- and post-treatment with amiodarone for
elective electrical cardioversion of atrial fibrillation: a systematic review and
meta-analysis. Europace 2019;21:856863.
557. Schmidt AS, Lauridsen KG, Torp P, Bach LF, Rickers H, Lofgren B. Maximum-
fixed energy shocks for cardioverting atrial fibrillation. Eur Heart J
2020;41:626631.
558. Pluymaekers N, Dudink E, Luermans J, Meeder JG, Lenderink T, Widdershoven
J, Bucx JJJ, Rienstra M, Kamp O, Van Opstal JM, Alings M, Oomen A, Kirchhof
CJ, Van Dijk VF, Ramanna H, Liem A, Dekker LR, Essers BAB, Tijssen JGP, Van
Gelder IC, Crijns H; RACE ACWAS Investigators. Early or delayed cardiover-
sion in recent-onset atrial fibrillation. N Engl J Med 2019;380:14991508.
559. Baranchuk A, Yeung C. Advanced interatrial block predicts atrial fibrillation
recurrence across different populations: learning Bayes syndrome. Int J Cardiol
2018;272:221222.
560. Toufan M, Kazemi B, Molazadeh N. The significance of the left atrial volume
index in prediction of atrial fibrillation recurrence after electrical cardioversion.
J Cardiovasc Thorac Res 2017;9:5459.
561. Voskoboinik A, Kalman E, Plunkett G, Knott J, Moskovitch J, Sanders P, Kistler
PM, Kalman JM. A comparison of early versus delayed elective electrical cardio-
version for recurrent episodes of persistent atrial fibrillation: a multi-center
study. Int J Cardiol 2019;284:3337.
562. Furniss SS, Sneyd JR. Safe sedation in modern cardiological practice. Heart
2015;101:15261530.
563. Mittal S, Ayati S, Stein KM, Schwartzman D, Cavlovich D, Tchou PJ, Markowitz
SM, Slotwiner DJ, Scheiner MA, Lerman BB. Transthoracic cardioversion of
atrial fibrillation: comparison of rectilinear biphasic versus damped sine wave
monophasic shocks. Circulation 2000;101:12821287.
564. Inacio JF, da Rosa Mdos S, Shah J, Rosario J, Vissoci JR, Manica AL, Rodrigues
CG. Monophasic and biphasic shock for transthoracic conversion of atrial fibril-
lation: systematic review and network meta-analysis. Resuscitation
2016;100
:6675.
565. Kirkland S, Stiell I, AlShawabkeh T, Campbell S, Dickinson G, Rowe BH. The
efficacy of pad placement for electrical cardioversion of atrial fibrillation/flutter:
a systematic review. Acad Emerg Med 2014;21:717726.
566. Boriani G, Diemberger I, Biffi M, Martignani C, Branzi A. Pharmacological cardi-
oversion of atrial fibrillation: current management and treatment options. Drugs
2004;64:27412762.
567. Danias PG, Caulfield TA, Weigner MJ, Silverman DI, Manning WJ. Likelihood of
spontaneous conversion of atrial fibrillation to sinus rhythm. J Am Coll Cardiol
1998;31:588592.
568. Dan GA, Martinez-Rubio A, Agewall S, Boriani G, Borggrefe M, Gaita F, van
Gelder I, Gorenek B, Kaski JC, Kjeldsen K, Lip GYH, Merkely B, Okumura K,
Piccini JP, Potpara T, Poulsen BK, Saba M, Savelieva I, Tamargo JL, Wolpert C,
ESC Scientific Document Group. Antiarrhythmic drugs-clinical use and clinical
decision making: a consensus document from the European Heart Rhythm
Association (EHRA) and European Society of Cardiology (ESC) Working
Group on Cardiovascular Pharmacology, endorsed by the Heart Rhythm
Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS) and International
Society of Cardiovascular Pharmacotherapy (ISCP). Europace
2018;20:731732.
569. Markey GC, Salter N, Ryan J. Intravenous flecainide for emergency department
management of acute atrial fibrillation. J Emerg Med 2018;54:320327.
570. Chevalier P, Durand-Dubief A, Burri H, Cucherat M, Kirkorian G, Touboul P.
Amiodarone versus placebo and class Ic drugs for cardioversion of recent-
onset atrial fibrillation: a meta-analysis. J Am Coll Cardiol 2003;41:255262.
571. Capucci A, Lenzi T, Boriani G, Trisolino G, Binetti N, Cavazza M, Fontana G,
Magnani B. Effectiveness of loading oral flecainide for converting recent-onset
atrial fibrillation to sinus rhythm in patients without organic heart disease or
with only systemic hypertension. Am J Cardiol 1992;70:6972.
572. Donovan KD, Dobb GJ, Coombs LJ, Lee KY, Weekes JN, Murdock CJ, Clarke
GM. Efficacy of flecainide for the reversion of acute onset atrial fibrillation. Am J
Cardiol 1992;70:50A-54A; discussion 54A-55A.
573. Reisinger J, Gatterer E, Lang W, Vanicek T, Eisserer G, Bachleitner T, Niemeth
C, Aicher F, Grander W, Heinze G, Kuhn P, Siostrzonek P. Flecainide versus
ibutilide for immediate cardioversion of atrial fibrillation of recent onset. Eur
Heart J 2004;25:13181324.
574. Khan IA. Oral loading single dose flecainide for pharmacological cardioversion
of recent-onset atrial fibrillation. Int J Cardiol 2003;87:121128.
575. Galve E, Rius T, Ballester R, Artaza MA, Arnau JM, Garcia-Dorado D, Soler-
Soler J. Intravenous amiodarone in treatment of recent-onset atrial fibrillation:
results of a randomized, controlled study. J Am Coll Cardiol
1996;27:10791082.
576. Vardas PE, Kochiadakis GE, Igoumenidis NE, Tsatsakis AM, Simantirakis EN,
Chlouverakis GI. Amiodarone as a first-choice drug for restoring sinus rhythm
in patients with atrial fibrillation: a randomized, controlled study. Chest
2000;117:15381545.
577. Letelier LM, Udol K, Ena J, Weaver B, Guyatt GH. Effectiveness of amiodarone
for conversion of atrial fibrillation to sinus rhythm: a meta-analysis. Arch Intern
Med 2003;163:777785.
578. Bash LD, Buono JL, Davies GM, Martin A, Fahrbach K, Phatak H, Avetisyan R,
Mwamburi M. Systematic review and meta-analysis of the efficacy of cardiover-
sion by vernakalant and comparators in patients with atrial fibrillation.
Cardiovasc Drugs Ther 2012;26:167179.
579. Camm AJ, Capucci A, Hohnloser SH, Torp-Pedersen C, Van Gelder IC, Mangal
B, Beatch G; AVRO Investigators. A randomized active-controlled study com-
paring the efficacy and safety of vernakalant to amiodarone in recent-onset
atrial fibrillation. J Am Coll Cardiol 2011;57:313321.
580. Akel T, Lafferty J. Efficacy and safety of intravenous vernakalant for the rapid
conversion of recent-onset atrial fibrillation: a meta-analysis. Ann Noninvasive
Electrocardiol 2018;23:e12508.
581. Beatch GN, Mangal B. Safety and efficacy of vernakalant for the conversion of
atrial fibrillation to sinus rhythm; a phase 3b randomized controlled trial. BMC
Cardiovasc Disord 2016;16:113.
582. Roy D, Pratt CM, Torp-Pedersen C, Wyse DG, Toft E, Juul-Moller S, Nielsen T,
Rasmussen SL, Stiell IG, Coutu B, Ip JH, Pritchett EL, Camm AJ; Atrial
Arrhythmia Conversion Trial Investigators. Vernakalant hydrochloride for rapid
conversion of atrial fibrillation: a phase 3, randomized, placebo-controlled trial.
Circulation 2008;117:15181525.
583. Kowey PR, Dorian P, Mitchell LB, Pratt CM, Roy D, Schwartz PJ, Sadowski J,
Sobczyk D, Bochenek A, Toft E; Atrial Arrhythmia Conversion Trial
Investigators. Vernakalant hydrochloride for the rapid conversion of atrial fibril-
lation after cardiac surgery: a randomized, double-blind, placebo-controlled
trial. Circ Arrhythm Electrophysiol 2009;2:652659.
584. Pohjantahti-Maaroos H, Hyppola H, Lekkala M, Sinisalo E, Heikkola A,
Hartikainen J. Intravenous vernakalant in comparison with intravenous flecainide
in the cardioversion of recent-onset atrial fibrillation. Eur Heart J Acute
Cardiovasc Care 2019;8:114120.
585. Vos MA, Golitsyn SR, Stangl K, Ruda MY, Van Wijk LV, Harry JD, Perry KT,
Touboul P, Steinbeck G, Wellens HJ. Superiority of ibutilide (a new class III
agent) over DL-sotalol in converting atrial flutter and atrial fibrillation. The
Ibutilide/Sotalol Comparator Study Group. Heart 1998;79:568575.
586. Alboni P, Botto GL, Baldi N, Luzi M, Russo V, Gianfranchi L, Marchi P, Calzolari
M, Solano A, Baroffio R, Gaggioli G. Outpatient treatment of recent-onset atrial
fibrillation with the ‘pill-in-the-pocket’ approach. N Engl J Med
2004;351:23842391.
587. Brembilla-Perrot B, Houriez P, Beurrier D, Claudon O, Terrier de la Chaise A,
Louis P. Predictors of atrial flutter with 1:1 conduction in patients treated with
class I antiarrhythmic drugs for atrial tachyarrhythmias. Int J Cardiol
2001;80:715.
588. Zhang N, Guo JH, Zhang H, Li XB, Zhang P, Xn Y. Comparison of intravenous
ibutilide vs. propafenone for rapid termination of recent onset atrial fibrillation.
Int J Clin Pract 2005;59
:13951400.
589. Conde D, Costabel JP, Caro M, Ferro A, Lambardi F, Corrales Barboza A,
Lavalle Cobo A, Trivi M. Flecainide versus vernakalant for conversion of recent-
onset atrial fibrillation. Int J Cardiol 2013;168:24232425.
590. Martinez-Marcos FJ, Garcia-Garmendia JL, Ortega-Carpio A, Fernandez-Gomez
JM, Santos JM, Camacho C. Comparison of intravenous flecainide, propafenone,
and amiodarone for conversion of acute atrial fibrillation to sinus rhythm. Am J
Cardiol 2000;86:950953.
591. Deedwania PC, Singh BN, Ellenbogen K, Fisher S, Fletcher R, Singh SN.
Spontaneous conversion and maintenance of sinus rhythm by amiodarone in
patients with heart failure and atrial fibrillation: observations from the veterans
100 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
affairs congestive heart failure survival trial of antiarrhythmic therapy (CHF-
STAT). The Department of Veterans Affairs CHF-STAT Investigators.
Circulation 1998;98:25742579.
592. Hofmann R, Steinwender C, Kammler J, Kypta A, Wimmer G, Leisch F.
Intravenous amiodarone bolus for treatment of atrial fibrillation in patients with
advanced congestive heart failure or cardiogenic shock. Wien Klin Wochenschr
2004;116:744749.
593. Crijns HJ, Weijs B, Fairley AM, Lewalter T, Maggioni AP, Martin A, Ponikowski
P, Rosenqvist M, Sanders P, Scanavacca M, Bash LD, Chazelle F, Bernhardt A,
Gitt AK, Lip GY, Le Heuzey JY. Contemporary real life cardioversion of atrial
fibrillation: results from the multinational RHYTHM-AF study. Int J Cardiol
2014;172:588594.
594. Kirchhof P, Andresen D, Bosch R, Borggrefe M, Meinertz T, Parade U, Ravens
U, Samol A, Steinbeck G, Treszl A, Wegscheider K, Breithardt G. Short-term
versus long-term antiarrhythmic drug treatment after cardioversion of atrial
fibrillation (Flec-SL): a prospective, randomised, open-label, blinded endpoint
assessment trial. Lancet 2012;380:238246.
595. Van Gelder IC, Tuinenburg AE, Schoonderwoerd BS, Tieleman RG, Crijns HJ.
Pharmacologic versus direct-current electrical cardioversion of atrial flutter and
fibrillation. Am J Cardiol 1999;84:147R151R.
596. Climent VE, Marin F, Mainar L, Gomez-Aldaravi R, Martinez JG, Chorro FJ,
Roman P, Sogorb F. Effects of pretreatment with intravenous flecainide on effi-
cacy of external cardioversion of persistent atrial fibrillation. Pacing Clin
Electrophysiol 2004;27:368372.
597. Mussigbrodt A, John S, Kosiuk J, Richter S, Hindricks G, Bollmann A.
Vernakalant-facilitated electrical cardioversion: comparison of intravenous ver-
nakalant and amiodarone for drug-enhanced electrical cardioversion of atrial
fibrillation after failed electrical cardioversion. Europace 2016;18:5156.
598. Singh SN, Tang XC, Reda D, Singh BN. Systematic electrocardioversion for
atrial fibrillation and role of antiarrhythmic drugs: a substudy of the SAFE-T trial.
Heart Rhythm 2009;6:152155.
599. Oral H, Souza JJ, Michaud GF, Knight BP, Goyal R, Strickberger SA, Morady F.
Facilitating transthoracic cardioversion of atrial fibrillation with ibutilide pre-
treatment. N Engl J Med 1999;340:18491854.
600. Khan IA. Single oral loading dose of propafenone for pharmacological cardi-
oversion of recent-onset atrial fibrillation. J Am Coll Cardiol
2001;37:542547.
601. Alboni P, Botto GL, Boriani G, Russo G, Pacchioni F, Iori M, Pasanisi G, Mancini
M, Mariconti B, Capucci A. Intravenous administration of flecainide or propafe-
none in patients with recent-onset atrial fibrillation does not predict adverse
effects during ‘pill-in-the-pocket’ treatment. Heart 2010;96:546549.
602. Arbelo E, Brugada J, Hindricks G, Maggioni A, Tavazzi L, Vardas P, Anselme F,
Inama G, Jais P, Kalarus Z, Kautzner J, Lewalter T, Mairesse G, Perez-Villacastin
J, Riahi S, Taborsky M, Theodorakis G, Trines S; Atrial Fibrillation Ablation Pilot
Study Investigators. ESC-EURObservational Research Programme: the Atrial
Fibrillation Ablation Pilot Study, conducted by the European Heart Rhythm
Association. Europace 2012;
14:10941103.
603. Arbelo E, Brugada J, Hindricks G, Maggioni AP, Tavazzi L, Vardas P, Laroche C,
Anselme F, Inama G, Jais P, Kalarus Z, Kautzner J, Lewalter T, Mairesse GH,
Perez-Villacastin J, Riahi S, Taborsky M, Theodorakis G, Trines SA; Atrial
Fibrillation Ablation Pilot Study Investigators. The atrial fibrillation ablation pilot
study: a European Survey on Methodology and results of catheter ablation for
atrial fibrillation conducted by the European Heart Rhythm Association. Eur
Heart J 2014;35:14661478.
604. Arbelo E, Brugada J, Blomstrom-Lundqvist C, Laroche C, Kautzner J,
Pokushalov E, Raatikainen P, Efremidis M, Hindricks G, Barrera A, Maggioni A,
Tavazzi L, Dagres N, on the behalf of the ESC EHRA Atrial Fibrillation Ablation
Long-term Registry Investigators. Contemporary management of patients
undergoing atrial fibrillation ablation: in-hospital and 1-year follow-up findings
from the ESC-EHRA atrial fibrillation ablation long-term registry. Eur Heart J
2017;38:13031316.
605. Krittayaphong R, Raungrattanaamporn O, Bhuripanyo K, Sriratanasathavorn C,
Pooranawattanakul S, Punlee K, Kangkagate C. A randomized clinical trial of
the efficacy of radiofrequency catheter ablation and amiodarone in the treat-
ment of symptomatic atrial fibrillation. J Med Assoc Thai 2003;86 Suppl
1:S816.
606. Stabile G, Bertaglia E, Senatore G, De Simone A, Zoppo F, Donnici G, Turco P,
Pascotto P, Fazzari M, Vitale DF. Catheter ablation treatment in patients with
drug-refractory atrial fibrillation: a prospective, multi-centre, randomized, con-
trolled study (Catheter Ablation For The Cure Of Atrial Fibrillation Study). Eur
Heart J 2006;27:216221.
607. Pappone C, Augello G, Sala S, Gugliotta F, Vicedomini G, Gulletta S, Paglino G,
Mazzone P, Sora N, Greiss I, Santagostino A, LiVolsi L, Pappone N, Radinovic
A, Manguso F, Santinelli V. A randomized trial of circumferential pulmonary
vein ablation versus antiarrhythmic drug therapy in paroxysmal atrial fibrillation:
the APAF Study. J Am Coll Cardiol 2006;48:23402347.
608. Calkins H, Reynolds MR, Spector P, Sondhi M, Xu Y, Martin A, Williams CJ,
Sledge I. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofre-
quency ablation: two systematic literature reviews and meta-analyses. Circ
Arrhythm Electrophysiol 2009;2:349361.
609. Packer DL, Kowal RC, Wheelan KR, Irwin JM, Champagne J, Guerra PG, Dubuc
M, Reddy V, Nelson L, Holcomb RG, Lehmann JW, Ruskin JN; STOP AF
Cryoablation Investigators. Cryoballoon ablation of pulmonary veins for parox-
ysmal atrial fibrillation: first results of the North American Arctic Front (STOP
AF) pivotal trial. J Am Coll Cardiol 2013;61:17131723.
610. Ganesan AN, Shipp NJ, Brooks AG, Kuklik P, Lau DH, Lim HS, Sullivan T,
Roberts-Thomson KC, Sanders P. Long-term outcomes of catheter ablation of
atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc
2013;2:e004549.
611. Di Biase L, Mohanty P, Mohanty S, Santangeli P, Trivedi C, Lakkireddy D, Reddy
M, Jais P, Themistoclakis S, Dello Russo A, Casella M, Pelargonio G, Narducci
ML, Schweikert R, Neuzil P, Sanchez J, Horton R, Beheiry S, Hongo R, Hao S,
Rossillo A, Forleo G, Tondo C, Burkhardt JD, Haissaguerre M, Natale A.
Ablation versus amiodarone for treatment of persistent atrial fibrillation in
patients with congestive heart failure and an implanted device: results from the
AATAC multicenter randomized trial. Circulation 2016;133:16371644.
612. Kuck KH, Brugada J, Furnkranz A, Metzner A, Ouyang F, Chun KR, Elvan A,
Arentz T, Bestehorn K, Pocock SJ, Albenque JP, Tondo C; FIRE AND ICE
Investigators. Cryoballoon or radiofrequency ablation for paroxysmal atrial
fibrillation. N Engl J Med 2016;374:22352245.
613. Sohara H, Ohe T, Okumura K, Naito S, Hirao K, Shoda M, Kobayashi Y,
Yamauchi Y, Yamaguchi Y, Kuwahara T, Hirayama H, YeongHwa C, Kusano K,
Kaitani K, Banba K, Fujii S, Kumagai K, Yoshida H, Matsushita M, Satake S,
Aonuma K. HotBalloon ablation of the pulmonary veins for paroxysmal AF: a
multicenter randomized trial in Japan. J Am Coll Cardiol 2016;68:27472757.
614. Hakalahti A, Biancari F, Nielsen JC, Raatikainen MJ. Radiofrequency ablation vs.
antiarrhythmic drug therapy as first line treatment of symptomatic atrial fibrilla-
tion: systematic review and meta-analysis. Europace 2015;17:370378.
615. Nielsen JC, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H, Pehrson
SM, Englund A, Hartikainen J, Mortensen LS, Hansen PS; MANTRA-PAF
Investigators. Long-term efficacy of catheter ablation as first-line therapy for
paroxysmal atrial fibrillation: 5-year outcome in a randomised clinical trial.
Heart 2017;103:368376.
616. Chen C, Zhou X, Zhu M, Chen S, Chen J, Cai H, Dai J, Xu X, Mao W. Catheter
ablation versus medical therapy for patients with persistent atrial fibrillation: a
systematic review and meta-analysis of evidence from randomized controlled
trials. J Interv Card Electrophysio l 2018;52:918.
617. Packer DL, Mark DB, Robb RA, Monahan KH, Bahnson TD, Poole JE,
Noseworthy PA, Rosenberg YD, Jeffries N, Mitchell LB, Flaker GC, Pokushalov
E, Romanov A, Bunch TJ, Noelker G, Ardashev A, Revishvili A, Wilber DJ,
Cappato R, Kuck KH, Hindricks G, Davies DW, Kowey PR, Naccarelli GV,
Reiffel JA, Piccini JP, Silverstein AP, Al-Khalidi HR, Lee KL; CABANA
Investigators. Effect of catheter ablation vs antiarrhythmic drug therapy on mor-
tality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation:
the CABANA randomized clinical trial. JAMA 2019;321:12611274.
618. Noseworthy PA, Gersh BJ, Kent DM, Piccini JP, Packer DL, Shah ND, Yao X.
Atrial fibrillation ablation in practice: assessing CABANA generalizability. Eur
Heart J 2019;40:12571264.
619. Teh AW, Kistler PM, Lee G, Medi C, Heck PM, Spence SJ, Sparks PB, Morton
JB, Kalman JM. Electroanatomic remodeling of the left atrium in paroxysmal and
persistent atrial fibrillation patients without structural heart disease. J Cardiovasc
Electrophysiol 2012;23:232238.
620. D’Ascenzo F, Corleto A, Biondi-Zoccai G, Anselmino M, Ferraris F, di Biase L,
Natale A, Hunter RJ, Schilling RJ, Miyazaki S, Tada H, Aonuma K, Yenn-Jiang L,
Tao H, Ma C, Packer D, Hammill S, Gaita F. Which are the most reliable predic-
tors of recurrence of atrial fibrillation after transcatheter ablation?: a meta-anal-
ysis. Int J Cardiol 2013;167:19841989.
621. Berruezo A, Tamborero D, Mont L, Benito B, Tolosana JM, Sitges M, Vidal B,
Arriagada G, Mendez F, Matiello M, Molina I, Brugada J. Pre-procedural predic-
tors of atrial fibrillation recurrence after circumferential pulmonary vein abla-
tion. Eur Heart J 2007;28:836841.
622. Nedios S, Kosiuk J, Koutalas E, Kornej J, Sommer P, Arya A, Richter S, Rolf S,
Husser D, Hindricks G, Bollmann A. Comparison of left atrial dimensions in CT
and echocardiography as predictors of long-term success after catheter ablation
of atrial fibrillation. J Interv Card Electrophysiol 2015;43:237244.
623. Njoku A, Kannabhiran M, Arora R, Reddy P, Gopinathannair R, Lakkireddy D,
Dominic P. Left atrial volume predicts atrial fibrillation recurrence after radio-
frequency ablation: a meta-analysis. Europace 2018;20:3342.
624. Costa FM, Ferreira AM, Oliveira S, Santos PG, Durazzo A, Carmo P, Santos KR,
Cavaco D, Parreira L, Morgado F, Adragao P. Left atrial volume is more impor-
tant than the type of atrial fibrillation in predicting the long-term success of
catheter ablation. Int J Cardiol 2015;
184:5661.
ESC Guidelines 101

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
625. Marrouche NF, Wilber D, Hindricks G, Jais P, Akoum N, Marchlinski F,
Kholmovski E, Burgon N, Hu N, Mont L, Deneke T, Duytschaever M, Neumann
T, Mansour M, Mahnkopf C, Herweg B, Daoud E, Wissner E, Bansmann P,
Brachmann J. Association of atrial tissue fibrosis identified by delayed enhance-
ment MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA
2014;311:498506.
626. Kosich F, Schumacher K, Potpara T, Lip GY, Hindricks G, Kornej J. Clinical
scores used for the prediction of negative events in patients undergoing cathe-
ter ablation for atrial fibrillation. Clin Cardiol 2019;42:320329.
627. Kornej J, Hindricks G, Shoemaker MB, Husser D, Arya A, Sommer P, Rolf S,
Saavedra P, Kanagasundram A, Patrick Whalen S, Montgomery J, Ellis CR,
Darbar D, Bollmann A. The APPLE score: a novel and simple score for the pre-
diction of rhythm outcomes after catheter ablation of atrial fibrillation. Clin Res
Cardiol 2015;104:871876.
628. Kornej J, Hindricks G, Arya A, Sommer P, Husser D, Bollmann A. The APPLE
score a novel score for the prediction of rhythm outcomes after repeat
catheter ablation of atrial fibrillation. PLoS One 2017;12:e0169933.
629. Kornej J, Schumacher K, Dinov B, Kosich F, Sommer P, Arya A, Husser D,
Bollmann A, Lip GYH, Hindricks G. Prediction of electro-anatomical substrate
and arrhythmia recurrences using APPLE, DR-FLASH and MB-LATER scores in
patients with atrial fibrillation undergoing catheter ablation. Sci Rep
2018;8:12686.
630. Kosiuk J, Dinov B, Kornej J, Acou WJ, Schonbauer R, Fiedler L, Buchta P, Myrda
K, Gasior M, Polonski L, Kircher S, Arya A, Sommer P, Bollmann A, Hindricks
G, Rolf S. Prospective, multicenter validation of a clinical risk score for left atrial
arrhythmogenic substrate based on voltage analysis: DR-FLASH score. Heart
Rhythm 2015;12:22072212.
631. Mujovic N, Marinkovic M, Markovic N, Shantsila A, Lip GY, Potpara TS.
Prediction of very late arrhythmia recurrence after radiofrequency catheter
ablation of atrial fibrillation: the MB-LATER clinical score. Sci Rep 2017;7:40828.
632. Mesquita J, Ferreira AM, Cavaco D, Moscoso Costa F, Carmo P, Marques H,
Morgado F, Mendes M, Adragao P. Development and validation of a risk score
for predicting atrial fibrillation recurrence after a first catheter ablation proce-
dure ATLAS score. Europace 2018;20:f428f435.
633. Winkle RA, Jarman JW, Mead RH, Engel G, Kong MH, Fleming W, Patrawala
RA. Predicting atrial fibrillation ablation outcome: the CAAP-AF score. Heart
Rhythm 2016;13:21192125.
634. Canpolat U, Aytemir K, Yorgun H, Sahiner L, Kaya EB, Oto A. A proposal for a
new scoring system in the prediction of catheter ablation outcomes: promising
results from the Turkish Cryoablation Registry. Int J Cardiol 2013;169:201206.
635. Wojcik M, Berkowitsch A, Greiss H, Zaltsberg S, Pajitnev D, Deubner N,
Hamm CW, Pitschner HF, Kuniss M, Neumann T. Repeated catheter ablation
of atrial fibrillation: how to predict outcome?Circ J 2013;77:22712279.
636. Pathak RK, Middeldorp ME, Lau DH, Mehta AB, Mahajan R, Twomey D,
Alasady M, Hanley L, Antic NA, McEvoy RD, Kalman JM, Abhayaratna WP,
Sanders P. Aggressive risk factor reduction study for atrial fibrillation and impli-
cations for the outcome of ablation: the ARREST-AF cohort study. J Am Coll
Cardiol
2014;64:22222231.
637. Trines SA, Stabile G, Arbelo E, Dagres N, Brugada J, Kautzner J, Pokushalov E,
Maggioni AP, Laroche C, Anselmino M, Beinart R, Traykov V, Blomstrom-
Lundqvist C. Influence of risk factors in the ESC-EHRA EORP atrial fibrillation
ablation long-term registry. Pacing Clin Electrophysiol 2019;42:13651373.
638. Wong CX, Sullivan T, Sun MT, Mahajan R, Pathak RK, Middeldorp M, Twomey
D, Ganesan AN, Rangnekar G, Roberts-Thomson KC, Lau DH, Sanders P.
Obesity and the risk of incident, post-operative, and post-ablation atrial fibrilla-
tion: a meta-analysis of 626,603 individuals in 51 studies. JACC Clin Electrophysiol
2015;1:139152.
639. Wokhlu A, Hodge DO, Monahan KH, Asirvatham SJ, Friedman PA, Munger TM,
Cha YM, Shen WK, Brady PA, Bluhm CM, Haroldson JM, Hammill SC, Packer
DL. Long-term outcome of atrial fibrillation ablation: impact and predictors of
very late recurrence. J Cardiovasc Electrophysiol 2010;21:10711078.
640. Arya A, Hindricks G, Sommer P, Huo Y, Bollmann A, Gaspar T, Bode K, Husser
D, Kottkamp H, Piorkowski C. Long-term results and the predictors of out-
come of catheter ablation of atrial fibrillation using steerable sheath catheter
navigation after single procedure in 674 patients. Europace 2010;12:173180.
641. Santoro F, Di Biase L, Trivedi C, Burkhardt JD, Paoletti Perini A, Sanchez J,
Horton R, Mohanty P, Mohanty S, Bai R, Santangeli P, Lakkireddy D, Reddy M,
Elayi CS, Hongo R, Beheiry S, Hao S, Schweikert RA, Viles-Gonzalez J, Fassini
G, Casella M, Dello Russo A, Tondo C, Natale A. Impact of uncontrolled
hypertension on atrial fibrillation ablation outcome. JACC Clin Electrophysiol
2015;1:164173.
642. Letsas KP, Weber R, Burkle G, Mihas CC, Minners J, Kalusche D, Arentz T. Pre-
ablative predictors of atrial fibrillation recurrence following pulmonary vein iso-
lation: the potential role of inflammation. Europace 2009;11:158163.
643. Jongnarangsin K, Chugh A, Good E, Mukerji S, Dey S, Crawford T, Sarrazin
JF, Kuhne M, Chalfoun N, Wells D, Boonyapisit W, Pelosi F, Jr., Bogun F,
Morady F, Oral H. Body mass index, obstructive sleep apnea, and outcomes
of catheter ablation of atrial fibrillation. JCardiovascElectrophysiol
2008;19:668672.
644. Patel D, Mohanty P, Di Biase L, Shaheen M, Lewis WR, Quan K, Cummings JE,
Wang P, Al-Ahmad A, Venkatraman P, Nashawati E, Lakkireddy D, Schweikert
R, Horton R, Sanchez J, Gallinghouse J, Hao S, Beheiry S, Cardinal DS,
Zagrodzky J, Canby R, Bailey S, Burkhardt JD, Natale A. Safety and efficacy of
pulmonary vein antral isolation in patients with obstructive sleep apnea: the
impact of continuous positive airway pressure. Circ Arrhythm Electrophysiol
2010;3:445451.
645. Matiello M, Nadal M, Tamborero D, Berruezo A, Montserrat J, Embid C, Rios J,
Villacastin J, Brugada J, Mont L. Low efficacy of atrial fibrillation ablation in
severe obstructive sleep apnoea patients. Europace 2010;12:10841089.
646. Chilukuri K, Dalal D, Gadrey S, Marine JE, Macpherson E, Henrikson CA,
ChengA,NazarianS,SinhaS,SpraggD,BergerR,CalkinsH.Aprospective
study evaluating the role of obesity and obstructive sleep apnea for outcomes
after catheter ablation of atrial fibrillation. J Cardiovasc Electrophysi ol
2010;21:521525.
647. Ng CY, Liu T, Shehata M, Stevens S, Chugh SS, Wang X. Meta-analysis of
obstructive sleep apnea as predictor of atrial fibrillation recurrence after cathe-
ter ablation. Am J Cardiol 2011;108:4751.
648. Naruse Y, Tada H, Satoh M, Yanagihara M, Tsuneoka H, Hirata Y, Ito Y, Kuroki
K, Machino T, Yamasaki H, Igarashi M, Sekiguchi Y, Sato A, Aonuma K.
Concomitant obstructive sleep apnea increases the recurrence of atrial fibrilla-
tion following radiofrequency catheter ablation of atrial fibrillation: clinical
impact of continuous positive airway pressure therapy. Heart Rhythm
2013;10:331337.
649. Li L, Wang ZW, Li J, Ge X, Guo LZ, Wang Y, Guo WH, Jiang CX, Ma CS.
Efficacy of catheter ablation of atrial fibrillation in patients with obstructive
sleep apnoea with and without continuous positive airway pressure treatment:
a meta-analysis of observational studies. Europace 2014;16:13091314.
650. Kawakami H, Nagai T, Fujii A, Uetani T, Nishimura K, Inoue K, Suzuki J, Oka Y,
Okura T, Higaki J, Ogimoto A, Ikeda S. Apnea-hypopnea index as a predictor of
atrial fibrillation recurrence following initial pulmonary vein isolation: usefulness
of type-3 portable monitor for sleep-disordered breathing. J Interv Card
Electrophysiol 2016;47:237244.
651. Congrete S, Bintvihok M, Thongprayoon C, Bathini T, Boonpheng B, Sharma K,
Chokesuwattanaskul R, Srivali N, Tanawuttiwat T, Cheungpasitporn W. Effect of
obstructive sleep apnea and its treatment of atrial fibrillation recurrence after radio-
frequency catheter ablation: a meta-analysis. JEvidBasedMed2018;11:145151.
652. Deng F, Raza A, Guo J. Treating obstructive sleep apnea with continuous posi-
tive airway pressure reduces risk of recurrent atrial fibrillation after catheter
ablation: a meta-analysis. Sleep Med 2018;46:511.
653. Wokhlu A, Monahan KH, Hodge DO, Asirvatham SJ, Friedman PA, Munger TM,
Bradley DJ, Bluhm CM, Haroldson JM, Packer DL. Long-term quality of life after
ablation of atrial fibrillation the impact of recurrence, symptom relief, and pla-
cebo effect. J Am Coll Cardiol 2010;55:2308 2316.
654. Reddy VY, Dukkipati SR, Neuzil P, Natale A, Albenque JP, Kautzner J, Shah D,
Michaud G, Wharton M, Harari D, Mahapatra S, Lambert H, Mansour M.
Randomized, controlled trial of the safety and effectiveness of a contact force-
sensing irrigated catheter for ablation of paroxysmal atrial fibrillation: results of
the TactiCath Contact Force Ablation Catheter Study for Atrial Fibrillation
(TOCCASTAR) Study. Circulation 2015;132:907915.
655. Mark DB, Anstrom KJ, Sheng S, Piccini JP, Baloch KN, Monahan KH, Daniels
MR, Bahnson TD, Poole JE, Rosenberg Y, Lee KL, Packer DL. Effect of catheter
ablation vs medical therapy on quality of life among patients with atrial fibrilla-
tion: the CABANA randomized clinical trial. JAMA 2019;321:12751285.
656. Kirchhof P, Breithardt G, Camm AJ, Crijns HJ, Kuck KH, Vardas P, Wegscheider
K. Improving outcomes in patients with atrial fibrillation: rationale and design of
the Early treatment of Atrial fibrillation for Stroke prevention Trial. Am Heart J
2013;166:442448.
657. Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L,
Merkely B, Pokushalov E, Sanders P, Proff J, Schunkert H, Christ H, Vogt J,
Bansch D; CASTLE-AF Investigators. Catheter ablation for atrial fibrillation with
heart failure. N Engl J Med 2018;378:417427.
658. Noseworthy PA, Van Houten HK, Gersh BJ, Packer DL, Friedman PA, Shah
ND, Dunlay SM, Siontis KC, Piccini JP, Yao X. Generalizability of the CASTLE-
AF trial: catheter ablation for patients with atrial fibrillation and heart failure in
routine practice. Heart Rhythm 2020;17:10571065.
659. Kuck KH, Merkely B, Zahn R, Arentz T, Seidl K, Schluter M, Tilz RR, Piorkowski
C, Geller L, Kleemann T, Hindricks G. Catheter ablation versus best medical
therapy in patients with persistent atrial fibrillation and congestive heart failure:
the randomized AMICA trial. Circ Arrhythm Electrophysiol 2019;12:e007731.
660. Packer DL, Monahan KH, Al-KhalidiHR, Silverstein AP, Poole JP, Bahnson TD,
Mark DB, Lee KL. Ablation of Atrial Fibrillation in Heart Failure Patients:
Additional outcomes of the CABANATrial. Heart Rhythm 2019;16(suppl):S35.
102 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
661. Khan MN, Jais P, Cummings J, Di Biase L, Sanders P, Martin DO, Kautzner J,
Hao S, Themistoclakis S, Fanelli R, Potenza D, Massaro R, Wazni O, Schweikert
R, Saliba W, Wang P, Al-Ahmad A, Beheiry S, Santarelli P, Starling RC, Dello
Russo A, Pelargonio G, Brachmann J, Schibgilla V, Bonso A, Casella M, Raviele
A, Haissaguerre M, Natale A; PABA-CHF Investigators. Pulmonary-vein isola-
tion for atrial fibrillation in patients with heart failure. N Engl J Med
2008;359:17781785.
662. MacDonald MR, Connelly DT, Hawkins NM, Steedman T, Payne J, Shaw M,
Denvir M, Bhagra S, Small S, Martin W, McMurray JJ, Petrie MC.
Radiofrequency ablation for persistent atrial fibrillation in patients with
advanced heart failure and severe left ventricular systolic dysfunction: a rando-
mised controlled trial. Heart 2011;97:740747.
663. Jones DG, Haldar SK, Hussain W, Sharma R, Francis DP, Rahman-Haley SL,
McDonagh TA, Underwood SR, Markides V, Wong T. A randomized trial to
assess catheter ablation versus rate control in the management of persistent
atrial fibrillation in heart failure. J Am Coll Cardiol 2013;61:18941903.
664. Hunter RJ, Berriman TJ, Diab I, Kamdar R, Richmond L, Baker V, Goromonzi F,
Sawhney V, Duncan E, Page SP, Ullah W, Unsworth B, Mayet J, Dhinoja M,
Earley MJ, Sporton S, Schilling RJ. A randomized controlled trial of catheter
ablation versus medical treatment of atrial fibrillation in heart failure (the
CAMTAF trial). Circ Arrhythm Electrophysiol 2014;7:3138.
665. Al Halabi S, Qintar M, Hussein A, Alraies MC, Jones DG, Wong T, MacDonald
MR, Petrie MC, Cantillon D, Tarakji KG, Kanj M, Bhargava M, Varma N,
Baranowski B, Wilkoff BL, Wazni O, Callahan T, Saliba W, Chung MK. Catheter
ablation for atrial fibrillation in heart failure patients: a meta-analysis of random-
ized controlled trials. JACC Clin Electrophysiol 2015;1:200209.
666. Prabhu S, Taylor AJ, Costello BT, Kaye DM, McLellan AJA, Voskoboinik A,
Sugumar H, Lockwood SM, Stokes MB, Pathik B, Nalliah CJ, Wong GR,
Azzopardi SM, Gutman SJ, Lee G, Layland J, Mariani JA, Ling LH, Kalman JM,
Kistler PM. Catheter ablation versus medical rate control in atrial fibrillation
and systolic dysfunction: the CAMERA-MRI study. J Am Coll Cardiol
2017;70:19491961.
667. Elgendy AY, Mahmoud AN, Khan MS, Sheikh MR, Mojadidi MK, Omer M,
Elgendy IY, Bavry AA, Ellenbogen KA, Miles WM, McKillop M. Meta-analysis
comparing catheter-guided ablation versus conventional medical therapy for
patients with atrial fibrillation and heart failure with reduced ejection fraction.
Am J Cardiol 2018;122:806813.
668. Briceno DF, Markman TM, Lupercio F, Romero J, Liang JJ, Villablanca PA, Birati
EY, Garcia FC, Di Biase L, Natale A, Marchlinski FE, Santangeli P. Catheter abla-
tion versus conventional treatment of atrial fibrillation in patients with heart
failure with reduced ejection fraction: a systematic review and meta-analysis of
randomized controlled trials. J Interv Card Electrophysiol 2018;53:1929.
669. Ma Y, Bai F, Qin F, Li Y, Tu T, Sun C, Zhou S, Liu Q. Catheter ablation for
treatment of patients with atrial fibrillation and heart failure: a meta-analysis of
randomized controlled trials. BMC Cardiovasc Disord 2018;18:165.
670. Kheiri B, Osman M, Abdalla A, Haykal T, Ahmed S, Bachuwa G, Hassan M,
Bhatt DL. Catheter ablation of atrial fibrillation with heart failure: an updated
meta-analysis of randomized trials. Int J Cardiol 2018;269:170173.
671. Khan SU, Rahman H, Talluri S, Kaluski E. The clinical benefits and mortality
reduction associated with catheter ablation in subjects with atrial fibrillation: a
systematic review and meta-analysis. JACC Clin Electrophysiol 2018;4:626635.
672. Martin CA, Lambiase PD. Pathophysiology, diagnosis and treatment of tachycar-
diomyopathy. Heart 2017;
103:15431552.
673. Raymond-Paquin A, Nattel S, Wakili R, Tadros R. Mechanisms and clinical signif-
icance of arrhythmia-induced cardiomyopathy. Can J Cardiol
2018;34:14491460.
674. Brembilla-Perrot B, Ferreira JP, Manenti V, Sellal JM, Olivier A, Villemin T,
Beurrier D, De Chillou C, Louis P, Brembilla A, Juilliere Y, Girerd N. Predictors
and prognostic significance of tachycardiomyopathy: insights from a cohort of
1269 patients undergoing atrial flutter ablation. Eur J Heart Fail
2016;18:394401.
675. Dagres N, Varounis C, Gaspar T, Piorkowski C, Eitel C, Iliodromitis EK, Lekakis
JP, Flevari P, Simeonidou E, Rallidis LS, Tsougos E, Hindricks G, Sommer P,
Anastasiou-Nana M. Catheter ablation for atrial fibrillation in patients with left
ventricular systolic dysfunction. A systematic review and meta-analysis. J Card
Fail 2011;17:964970.
676. Prabhu S, Costello BT, Taylor AJ, Gutman SJ, Voskoboinik A, McLellan AJA,
Peck KY, Sugumar H, Iles L, Pathik B, Nalliah CJ, Wong GR, Azzopardi SM, Lee
G, Mariani J, Kaye DM, Ling LH, Kalman JM, Kistler PM. Regression of diffuse
ventricular fibrosis following restoration of sinus rhythm with catheter ablation
in patients with atrial fibrillation and systolic dysfunction: a substudy of the
CAMERA MRI trial. JACC Clin Electrophysiol 2018;4:9991007.
677. Tamborero D, Mont L, Berruezo A, Matiello M, Benito B, Sitges M, Vidal B, de
Caralt TM, Perea RJ, Vatasescu R, Brugada J. Left atrial posterior wall isolation
does not improve the outcome of circumferential pulmonary vein ablation for
atrial fibrillation: a prospective randomized study. Circ Arrhythm Electrophysiol
2009;2:3540.
678. Natale A, Reddy VY, Monir G, Wilber DJ, Lindsay BD, McElderry HT, Kantipudi
C, Mansour MC, Melby DP, Packer DL, Nakagawa H, Zhang B, Stagg RB, Boo
LM, Marchlinski FE. Paroxysmal AF catheter ablation with a contact force sens-
ing catheter: results of the prospective, multicenter SMART-AF trial. J Am Coll
Cardiol 2014;64:647656.
679. McLellan AJ, Ling LH, Azzopardi S, Lee GA, Lee G, Kumar S, Wong MC,
Walters TE, Lee JM, Looi KL, Halloran K, Stiles MK, Lever NA, Fynn SP, Heck
PM, Sanders P, Morton JB, Kalman JM, Kistler PM. A minimal or maximal abla-
tion strategy to achieve pulmonary vein isolation for paroxysmal atrial fibrilla-
tion: a prospective multi-centre randomized controlled trial (the Minimax
study). Eur Heart J 2015;36:18121821.
680. Verma A, Jiang CY, Betts TR, Chen J, Deisenhofer I, Mantovan R, Macle L,
Morillo CA, Haverkamp W, Weerasooriya R, Albenque JP, Nardi S, Menardi E,
Novak P, Sanders P; STAR AF II Investigators. Approaches to catheter ablation
for persistent atrial fibrillation. N Engl J Med 2015;372:18121822.
681. Luik A, Radzewitz A, Kieser M, Walter M, Bramlage P, Hormann P, Schmidt K,
Horn N, Brinkmeier-Theofanopoulou M, Kunzmann K, Riexinger T, Schymik
G, Merkel M, Schmitt C. Cryoballoon versus open irrigated radiofrequency
ablation in patients with paroxysmal atrial fibrillation: the prospective,
randomized, controlled, noninferiority FreezeAF study. Circulation
2015;132:13111319.
682. Dukkipati SR, Cuoco F, Kutinsky I, Aryana A, Bahnson TD, Lakkireddy D,
Woollett I, Issa ZF, Natale A, Reddy VY; HeartLight Study Investigators.
Pulmonary vein isolation using the visually guided laser balloon: a prospective,
multicenter, and randomized comparison to standard radiofrequency ablation. J
Am Coll Cardiol 2015;66:13501360.
683. Kuck KH, Hoffmann BA, Ernst S, Wegscheider K, Treszl A, Metzner A, Eckardt
L, Lewalter T, Breithardt G, Willems S; Gap-AF
AFNET 1 Investigators.
Impact of complete versus incomplete circumferential lines around the pulmo-
nary veins during catheter ablation of paroxysmal atrial fibrillation: results from
the Gap-Atrial Fibrillation-German Atrial Fibrillation Competence Network 1
trial. Circ Arrhythm Electrophysiol 2016;9:e003337.
684. Nery PB, Belliveau D, Nair GM, Bernick J, Redpath CJ, Szczotka A, Sadek MM,
Green MS, Wells G, Birnie DH. Relationship between pulmonary vein recon-
nection and atrial fibrillation recurrence: a systematic review and meta-analysis.
JACC Clin Electrophysiol 2016;2:474483.
685. Bassiouny M, Saliba W, Hussein A, Rickard J, Diab M, Aman W, Dresing T, Tt
Callahan, Bhargava M, Martin DO, Shao M, Baranowski B, Tarakji K, Tchou PJ,
Hakim A, Kanj M, Lindsay B, Wazni O. Randomized study of persistent atrial
fibrillation ablation: ablate in sinus rhythm versus ablate complex-fractionated
atrial electrograms in atrial fibrillation. Circ Arrhythm Electrophysiol
2016;9:e003596.
686. Hindricks G, Sepehri Shamloo A, Lenarczyk R, Kalarus Z, Arya A, Kircher S,
Darma A, Dagres N. Catheter ablation of atrial fibrillation: current status, tech-
niques, outcomes and challenges. Kardiol Pol 2018;76:16801686.
687. Nanthakumar K, Plumb VJ, Epstein AE, Veenhuyzen GD, Link D, Kay GN.
Resumption of electrical conduction in previously isolated pulmonary veins:
rationale for a different strategy?Circulation 2004;109:12261229.
688. Verma A, Kilicaslan F, Pisano E, Marrouche NF, Fanelli R, Brachmann J,
Geunther J, Potenza D, Martin DO, Cummings J, Burkhardt JD, Saliba W,
Schweikert RA, Natale A. Response of atrial fibrillation to pulmonary vein
antrum isolation is directly related to resumption and delay of pulmonary vein
conduction. Circulation 2005;112:627635.
689. Ouyang F, Antz M, Ernst S, Hachiya H, Mavrakis H, Deger FT, Schaumann A,
Chun J, Falk P, Hennig D, Liu X, Bansch D, Kuck KH. Recovered pulmonary
vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after
complete circular isolation of the pulmonary veins: lessons from double Lasso
technique. Circulation 2005;111:127135.
690. Cheema A, Dong J, Dalal D, Marine JE, Henrikson CA, Spragg D, Cheng A,
Nazarian S, Bilchick K, Sinha S, Scherr D, Almasry I, Halperin H, Berger R,
Calkins H. Incidence and time course of early recovery of pulmonary vein con-
duction after catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol
2007;18:387391.
691. Pratola C, Baldo E, Notarstefano P, Toselli T, Ferrari R. Radiofrequency ablation
of atrial fibrillation: is the persistence of all intraprocedural targets necessary
for long-term maintenance of sinus rhythm?Circulation 2008;117:136143.
692. Rajappan K, Kistler PM, Earley MJ, Thomas G, Izquierdo M, Sporton SC,
Schilling RJ. Acute and chronic pulmonary vein reconnection after atrial fibrilla-
tion ablation: a prospective characterization of anatomical sites. Pacing Clin
Electrophysiol 2008;31:15981605.
693. Bansch D, Bittkau J, Schneider R, Schneider C, Wendig I, Akin I, Nienaber CA.
Circumferential pulmonary vein isolation: wait or stop early after initial success-
ful pulmonary vein isolation?Europace 2013;15:183188.
ESC Guidelines 103

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
694. Nakamura K, Naito S, Kaseno K, Tsukada N, Sasaki T, Hayano M, Nishiuchi S,
Fuke E, Miki Y, Sakamoto T, Nakamura K, Kumagai K, Kataoka A, Takaoka H,
Kobayashi Y, Funabashi N, Oshima S. Optimal observation time after comple-
tion of circumferential pulmonary vein isolation for atrial fibrillation to prevent
chronic pulmonary vein reconnections. Int J Cardiol 2013;168:53005310.
695. Neuzil P, Reddy VY, Kautzner J, Petru J, Wichterle D, Shah D, Lambert H,
Yulzari A, Wissner E, Kuck KH. Electrical reconnection after pulmonary vein
isolation is contingent on contact force during initial treatment: results from the
EFFICAS I study. Circ Arrhythm Electrophysiol 2013;6:327333.
696. Jiang RH, Po SS, Tung R, Liu Q, Sheng X, Zhang ZW, Sun YX, Yu L, Zhang P, Fu
GS, Jiang CY. Incidence of pulmonary vein conduction recovery in patients
without clinical recurrence after ablation of paroxysmal atrial fibrillation: mech-
anistic implications. Heart Rhythm 2014;11:969976.
697. Kim TH, Park J, Uhm JS, Joung B, Lee MH, Pak HN. Pulmonary vein reconnec-
tion predicts good clinical outcome after second catheter ablation for atrial
fibrillation. Europace 2017;19:961967.
698. Bordignon S, Furnkranz A, Perrotta L, Dugo D, Konstantinou A, Nowak B,
Schulte-Hahn B, Schmidt B, Chun KR. High rate of durable pulmonary vein iso-
lation after second-generation cryoballoon ablation: analysis of repeat proce-
dures. Europace 2015;17:725731.
699. Ullah W, McLean A, Tayebjee MH, Gupta D, Ginks MR, Haywood GA, O’Neill
M, Lambiase PD, Earley MJ, Schilling RJ, Group UKMT. Randomized trial com-
paring pulmonary vein isolation using the SmartTouch catheter with or without
real-time contact force data. Heart Rhythm 2016;13:17611767.
700. Phlips T, Taghji P, El Haddad M, Wolf M, Knecht S, Vandekerckhove Y,
Tavernier R, Duytschaever M. Improving procedural and one-year outcome
after contact force-guided pulmonary vein isolation: the role of interlesion dis-
tance, ablation index, and contact force variability in the ‘CLOSE’-protocol.
Europace 2018;20:f419f427.
701. Shah D, Haissaguerre M, Jais P, Hocini M. Nonpulmonary vein foci: do they
exist?Pacing Clin Electrophysiol 2003;26:16311635.
702. Nademanee K, McKenzie J, Kosar E, Schwab M, Sunsaneewitayakul B, Vasavakul
T, Khunnawat C, Ngarmukos T. A new approach for catheter ablation of atrial
fibrillation: mapping of the electrophysiologic substrate. J Am Coll Cardiol
2004;43:20442053.
703. Haissaguerre M, Sanders P, Hocini M, Takahashi Y, Rotter M, Sacher F, Rostock
T, Hsu LF, Bordachar P, Reuter S, Roudaut R, Clementy J, Jais P. Catheter abla-
tion of long-lasting persistent atrial fibrillation: critical structures for termina-
tion. J Cardiovasc Electrophysiol 2005;16:11251137.
704. Haissaguerre M, Hocini M, Sanders P, Sacher F, Rotter M, Takahashi Y, Rostock
T, Hsu LF, Bordachar P, Reuter S, Roudaut R, Clementy J, Jais P. Catheter abla-
tion of long-lasting persistent atrial fibrillation: clinical outcome and mechanisms
of subsequent arrhythmias. J Cardiovasc Electrophysiol 2005;16:11381147.
705. Jaı¨s P, O’Neill MD, Takahashi Y, Jo¨nsson A, Hocini M, Sacher F, Sanders P,
Kodali S, Rostock T, Rotter M, Cle´menty J, Haı¨ssaguerre M. Stepwise catheter
ablation of chronic atrial fibrillation:importance of discrete anatomic sites for
termination. J Cardiovasc Electrophysiol 2006;17:S28S36.
706. Atienza F, Almendral J, Jalife J, Zlochiver S, Ploutz-Snyder R, Torrecilla EG,
Arenal A, Kalifa J, Fernandez-Aviles F, Berenfeld O. Real-time dominant fre-
quency mapping and ablation of dominant frequency sites in atrial fibrillation
with left-to-right frequency gradients predicts long-term maintenance of sinus
rhythm. Heart Rhythm 2009;6:3340.
707. Stavrakis S, Nakagawa H, Po SS, Scherlag BJ, Lazzara R, Jackman WM. The role
of the autonomic ganglia in atrial fibrillation. JACC Clin Electrophysiol
2015;1:113.
708. Di Biase L, Burkhardt JD, Mohanty P, Mohanty S, Sanchez JE, Trivedi C, Gunes
M, Gokoglan Y, Gianni C, Horton RP, Themistoclakis S, Gallinghouse GJ, Bailey
S, Zagrodzky JD, Hongo RH, Beheiry S, Santangeli P, Casella M, Dello Russo A,
Al-Ahmad A, Hranitzky P, Lakkireddy D, Tondo C, Natale A. Left atrial append-
age isolation in patients with longstanding persistent af undergoing catheter
ablation: BELIEF trial. J Am Coll Cardiol 2016;68:19291940.
709. Gianni C, Mohanty S, Di Biase L, Metz T, Trivedi C, Gokoglan Y, Gunes MF, Bai
R, Al-Ahmad A, Burkhardt JD, Gallinghouse GJ, Horton RP, Hranitzky PM,
Sanchez JE, Halbfass P, Muller P, Schade A, Deneke T, Tomassoni GF, Natale A.
Acute and early outcomes of focal impulse and rotor modulation (FIRM)-guided
rotors-only ablation in patients with nonparoxysmal atrial fibrillation. Heart
Rhythm 2016;13:830835.
710. Santangeli P, Zado ES, Hutchinson MD, Riley MP, Lin D, Frankel DS, Supple GE,
Garcia FC, Dixit S, Callans DJ, Marchlinski FE. Prevalence and distribution of
focal triggers in persistent and long-standing persistent atrial fibrillation. Heart
Rhythm 2016;13:374382.
711. Katritsis DG, Pokushalov E, Romanov A, Giazitzoglou E, Siontis GC, Po SS,
Camm AJ, Ioannidis JP. Autonomic denervation added to pulmonary vein isola-
tion for paroxysmal atrial fibrillation: a randomized clinical trial. J Am Coll Cardiol
2013;62:23182325.
712. Arbelo E, Guiu E, Ramos P, Bisbal F, Borras R, Andreu D, Tolosana JM,
Berruezo A, Brugada J, Mont L. Benefit of left atrial roof linear ablation in par-
oxysmal atrial fibrillation: a prospective, randomized study. J Am Heart Assoc
2014;3:e000877.
713. Da Costa A, Levallois M, Romeyer-Bouchard C, Bisch L, Gate-Martinet A, Isaaz
K. Remote-controlled magnetic pulmonary vein isolation combined with supe-
rior vena cava isolation for paroxysmal atrial fibrillation: a prospective random-
ized study. Arch Cardiovasc Dis 2015;108:163171.
714. Wong KC, Paisey JR, Sopher M, Balasubramaniam R, Jones M, Qureshi N,
Hayes CR, Ginks MR, Rajappan K, Bashir Y, Betts TR. No benefit of complex
fractionated atrial electrogram ablation in addition to circumferential pulmonary
vein ablation and linear ablation: Benefit of Complex Ablation Study. Circ
Arrhythm Electrophysiol 2015;8:13161324.
715. Vogler J, Willems S, Sultan A, Schreiber D, Luker J, Servatius H, Schaffer B,
Moser J, Hoffmann BA, Steven D. Pulmonary vein isolation versus defragmenta-
tion: the CHASE-AF clinical trial. J Am Coll Cardiol 2015;66:27432752.
716. Faustino M, Pizzi C, Agricola T, Xhyheri B, Costa GM, Flacco ME, Capasso L,
Cicolini G, Di Girolamo E, Leonzio L, Manzoli L. Stepwise ablation approach
versus pulmonary vein isolation in patients with paroxysmal atrial fibrillation:
randomized controlled trial. Heart Rhythm 2015;12:19071915.
717. Scott PA, Silberbauer J, Murgatroyd FD. The impact of adjunctive complex frac-
tionated atrial electrogram ablation and linear lesions on outcomes in persistent
atrial fibrillation: a meta-analysis. Europace 2016;18:359367.
718. Driessen AHG, Berger WR, Krul SPJ, van den Berg NWE, Neefs J, Piersma FR,
Chan Pin Yin D, de Jong J, van Boven WP, de Groot JR. Ganglion plexus abla-
tion in advanced atrial fibrillation: the AFACT study. J Am Coll Cardiol
2016;68:11551165.
719. Qin M, Liu X, Wu SH, Zhang XD. Atrial substrate modification in atrial fibrilla-
tion: targeting GP or CFAE? Evidence from meta-analysis of clinical trials. PLoS
One 2016;11:e0164989.
720. Hu X, Jiang J, Ma Y, Tang A. Is there still a role for additional linear ablation in
addition to pulmonary vein isolation in patients with paroxysmal atrial fibrilla-
tion? An updated meta-analysis of randomized controlled trials. Int J Cardiol
2016;209:266274.
721. Wynn GJ, Panikker S, Morgan M, Hall M, Waktare J, Markides V, Hussain W,
Salukhe T, Modi S, Jarman J, Jones DG, Snowdon R, Todd D, Wong T, Gupta
D. Biatrial linear ablation in sustained nonpermanent AF: results of the substrate
modification with ablation and antiarrhythmic drugs in nonpermanent atrial
fibrillation (SMAN-PAF) trial. Heart Rhythm 2016;13:399406.
722. Zhang Z, Letsas KP, Zhang N, Efremidis M, Xu G, Li G, Liu T. Linear ablation
following pulmonary vein isolation in patients with atrial fibrillation: a meta-anal-
ysis. Pacing Clin Electrophysiol 2016;39:623630.
723. Fink T, Schluter M, Heeger CH, Lemes C, Maurer T, Reissmann B, Riedl J,
Rottner L, Santoro F, Schmidt B, Wohlmuth P, Mathew S, Sohns C, Ouyang F,
Metzner A, Kuck KH. Stand-alone pulmonary vein isolation versus pulmonary
vein isolation with additional substrate modification as index ablation proce-
dures in patients with persistent and long-standing persistent atrial fibrillation:
the randomized Alster-Lost-AF trial (Ablation at St. Georg Hospital for long-
standing persistent atrial fibrillation). Circ Arrhythm Electrophysiol 2017;10.
724. Kim TH, Uhm JS, Kim JY, Joung B, Lee MH, Pak HN. Does additional
electrogram-guided ablation after linear ablation reduce recurrence after cathe-
ter ablation for longstanding persistent atrial fibrillation? A prospective random-
ized study. J Am Heart Assoc 2017;6:e004811.
725. Kircher S, Arya A, Altmann D, Rolf S, Bollmann A, Sommer P, Dagres N,
Richter S, Breithardt OA, Dinov B, Husser D, Eitel C, Gaspar T, Piorkowski C,
Hindricks G. Individually tailored vs. standardized substrate modification during
radiofrequency catheter ablation for atrial fibrillation: a randomized study.
Europace 2018;20:17661775.
726. Ammar-Busch S, Bourier F, Reents T, Semmler V, Telishevska M, Kathan S,
Hofmann M, Hessling G, Deisenhofer I. Ablation of complex fractionated elec-
trograms with or without ADditional LINEar Lesions for Persistent Atrial
Fibrillation (the ADLINE trial). J Cardiovasc Electrophysiol 2017;28:636641.
727. Blandino A, Bianchi F, Grossi S, Biondi-Zoccai G, Conte MR, Gaido L, Gaita F,
Scaglione M, Rametta F. Left atrial substrate modification targeting low-voltage
areas for catheter ablation of atrial fibrillation: a systematic review and meta-
analysis. Pacing Clin Electrophysiol 2017;40:199
212.
728. Yang B, Jiang C, Lin Y, Yang G, Chu H, Cai H, Lu F, Zhan X, Xu J, Wang X,
Ching CK, Singh B, Kim YH, Chen M; STABLE-SR Investigators. STABLE-SR
(Electrophysiological Substrate Ablation in the Left Atrium During Sinus
Rhythm) for the treatment of nonparoxysmal atrial fibrillation: a prospective,
multicenter randomized clinical trial. Circ Arrhythm Electrophysiol 2017;10:pii:
e005405.
729. Yu HT, Shim J, Park J, Kim IS, Kim TH, Uhm JS, Joung B, Lee MH, Kim YH, Pak
HN. Pulmonary vein isolation alone versus additional linear ablation in patients
with persistent atrial fibrillation converted to paroxysmal type with
104 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
antiarrhythmic drug therapy: a multicenter, prospective, randomized study. Circ
Arrhythm Electrophysiol 2017;10:pii: e004915.
730. Wang YL, Liu X, Zhang Y, Jiang WF, Zhou L, Qin M, Zhang DL, Zhang XD, Wu
SH, Xu K. Optimal endpoint for catheter ablation of longstanding persistent
atrial fibrillation: a randomized clinical trial. Pacing Clin Electrophysiol
2018;41:172178.
731. Perez FJ, Schubert CM, Parvez B, Pathak V, Ellenbogen KA, Wood MA. Long-
term outcomes after catheter ablation of cavo-tricuspid isthmus dependent
atrial flutter: a meta-analysis. Circ Arrhythm Electrophysiol 2009;2:393401.
732. Natale A, Newby KH, Pisano E, Leonelli F, Fanelli R, Potenza D, Beheiry S,
Tomassoni G. Prospective randomized comparison of antiarrhythmic therapy
versus first-line radiofrequency ablation in patients with atrial flutter. J Am Coll
Cardiol 2000;35:18981904.
733. Wazni O, Marrouche NF, Martin DO, Gillinov AM, Saliba W, Saad E, Klein A,
Bhargava M, Bash D, Schweikert R, Erciyes D, Abdul-Karim A, Brachman J,
Gunther J, Pisano E, Potenza D, Fanelli R, Natale A. Randomized study compar-
ing combined pulmonary vein-left atrial junction disconnection and cavotricus-
pid isthmus ablation versus pulmonary vein-left atrial junction disconnection
alone in patients presenting with typical atrial flutter and atrial fibrillation.
Circulation 2003;108:24792483.
734. Shah DC, Sunthorn H, Burri H, Gentil-Baron P. Evaluation of an individualized
strategy of cavotricuspid isthmus ablation as an adjunct to atrial fibrillation abla-
tion. J Cardiovasc Electrophysiol 2007;18:926930.
735. Neumann T, Kuniss M, Conradi G, Janin S, Berkowitsch A, Wojcik M, Rixe J,
Erkapic D, Zaltsberg S, Rolf A, Bachmann G, Dill T, Hamm CW, Pitschner HF.
MEDAFI-Trial (Micro-embolization during ablation of atrial fibrillation): compar-
ison of pulmonary vein isolation using cryoballoon technique vs. radiofrequency
energy. Europace 2011;13:3744.
736. Herrera Siklody C, Deneke T, Hocini M, Lehrmann H, Shin DI, Miyazaki S,
Henschke S, Fluegel P, Schiebeling-Romer J, Bansmann PM, Bourdias T, Dousset
V, Haissaguerre M, Arentz T. Incidence of asymptomatic intracranial
embolic events after pulmonary vein isolation: comparison of different atrial
fibrillation ablation technologies in a multicenter study. J Am Coll Cardiol
2011;58:681688.
737. Herrera Siklody C, Arentz T, Minners J, Jesel L, Stratz C, Valina CM, Weber R,
Kalusche D, Toti F, Morel O, Trenk D. Cellular damage, platelet activation, and
inflammatory response after pulmonary vein isolation: a randomized study com-
paring radiofrequency ablation with cryoablation. Heart Rhythm
2012;9:189196.
738. Pokushalov E, Romanov A, Artyomenko S, Baranova V, Losik D, Bairamova S,
Karaskov A, Mittal S, Steinberg JS. Cryoballoon versus radiofrequency for pul-
monary vein re-isolation after a failed initial ablation procedure in patients with
paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol 2013;24:274279.
739. Schmidt M, Dorwarth U, Andresen D, Brachmann J, Kuck KH, Kuniss M,
Lewalter T, Spitzer S, Willems S, Senges J, Junger C, Hoffmann E. Cryoballoon
versus RF ablation in paroxysmal atrial fibrillation: results from the German
Ablation Registry. J Cardiovasc Electrophysiol 2014;25:17.
740. Perez-Castellano N, Fernandez-Cavazos R, Moreno J, Canadas V, Conde A,
Gonzalez-Ferrer JJ, Macaya C, Perez-Villacastin J. The COR trial: a randomized
study with continuous rhythm monitoring to compare the efficacy of cryoe-
nergy and radiofrequency for pulmonary vein isolation.
Heart Rhythm
2014;11:814.
741. Hunter RJ, Baker V, Finlay MC, Duncan ER, Lovell MJ, Tayebjee MH, Ullah W,
Siddiqui MS, Mc LA, Richmond L, Kirkby C, Ginks MR, Dhinoja M, Sporton S,
Earley MJ, Schilling RJ. Point-by-point radiofrequency ablation versus the cryo-
balloon or a novel combined approach: a randomized trial comparing 3 meth-
ods of pulmonary vein isolation for paroxysmal atrial fibrillation (the Cryo
Versus RF trial). J Cardiovasc Electrophysiol 2015;26:13071314.
742. Squara F, Zhao A, Marijon E, Latcu DG, Providencia R, Di Giovanni G, Jauvert
G, Jourda F, Chierchia GB, De Asmundis C, Ciconte G, Alonso C, Grimard C,
Boveda S, Cauchemez B, Saoudi N, Brugada P, Albenque JP, Thomas O.
Comparison between radiofrequency with contact force-sensing and second-
generation cryoballoon for paroxysmal atrial fibrillation catheter ablation: a
multicentre European evaluation. Europace 2015;17:718724.
743. Straube F, Dorwarth U, Ammar-Busch S, Peter T, Noelker G, Massa T, Kuniss
M, Ewertsen NC, Chun KR, Tebbenjohanns J, Tilz R, Kuck KH, Ouarrak T,
Senges J, Hoffmann E; Freeze Cohort Investigators. First-line catheter ablation
of paroxysmal atrial fibrillation: outcome of radiofrequency vs. cryoballoon pul-
monary vein isolation. Europace 2016;18:368375.
744. Schmidt M, Dorwarth U, Andresen D, Brachmann J, Kuck K, Kuniss M, Willems
S, Deneke T, Tebbenjohanns J, Gerds-Li JH, Spitzer S, Senges J, Hochadel M,
Hoffmann E. German ablation registry: cryoballoon vs. radiofrequency ablation
in paroxysmal atrial fibrillation one-year outcome data. Heart Rhythm
2016;13:836844.
745. Boveda S, Providencia R, Defaye P, Pavin D, Cebron JP, Anselme F, Halimi F,
Khoueiry Z, Combes N, Combes S, Jacob S, Albenque JP, Sousa P. Outcomes
after cryoballoon or radiofrequency ablation for persistent atrial fibrillation: a
multicentric propensity-score matched study. J Interv Card Electrophysiol
2016;47:133142.
746. Kuck KH, Furnkranz A, Chun KR, Metzner A, Ouyang F, Schluter M, Elvan A,
Lim HW, Kueffer FJ, Arentz T, Albenque JP, Tondo C, Kuhne M, Sticherling C,
Brugada J; FIRE AND ICE Investigators. Cryoballoon or radiofrequency ablation
for symptomatic paroxysmal atrial fibrillation: reintervention, rehospitalization,
and quality-of-life outcomes in the FIRE AND ICE trial. Eur Heart J
2016;37:28582865.
747. Buist TJ, Adiyaman A, Smit JJJ, Ramdat Misier AR, Elvan A. Arrhythmia-free sur-
vival and pulmonary vein reconnection patterns after second-generation cryo-
balloon and contact-force radiofrequency pulmonary vein isolation. Clin Res
Cardiol 2018;107:498506.
748. Gunawardene MA, Hoffmann BA, Schaeffer B, Chung DU, Moser J, Akbulak
RO, Jularic M, Eickholt C, Nuehrich J, Meyer C, Willems S. Influence of energy
source on early atrial fibrillation recurrences: a comparison of cryoballoon vs.
radiofrequency current energy ablation with the endpoint of unexcitability in
pulmonary vein isolation. Europace 2018;20:4349.
749. Mortsell D, Arbelo E, Dagres N, Brugada J, Laroche C, Trines SA, Malmborg H,
Hoglund N, Tavazzi L, Pokushalov E, Stabile G, Blomstrom-Lundqvist C; ESC-
EHRA Atrial Fibrillation Ablation Long-Term Registry Investigators.
Cryoballoon vs. radiofrequency ablation for atrial fibrillation: a study of out-
come and safety based on the ESC-EHRA atrial fibrillation ablation long-term
registry and the Swedish catheter ablation registry. Europace 2019;21:581589.
750. Akkaya E, Berkowitsch A, Zaltsberg S, Greiss H, Hamm CW, Sperzel J,
Neumann T, Kuniss M. Ice or fire? Comparison of second-generation cryobal-
loon ablation and radiofrequency ablation in patients with symptomatic persis-
tent atrial fibrillation and an enlarged left atrium. J Cardiovasc Electrophysiol
2018;29:375384.
751. Murray MI, Arnold A, Younis M, Varghese S, Zeiher AM. Cryoballoon versus
radiofrequency ablation for paroxysmal atrial fibrillation: a meta-analysis of
randomized controlled trials. Clin Res Cardiol 2018;107:658669.
752. Chen CF, Gao XF, Duan X, Chen B, Liu XH, Xu YZ. Comparison of catheter
ablation for paroxysmal atrial fibrillation between cryoballoon and radiofre-
quency: a meta-analysis. J Interv Card Electrophysiol 2017;48:351366.
753. Buiatti A, von Olshausen G, Barthel P, Schneider S, Luik A, Kaess B, Laugwitz
KL, Hoppmann P. Cryoballoon vs. radiofrequency ablation for paroxysmal atrial
fibrillation: an updated meta-analysis of randomized and observational studies.
Europace 2017;19:378384.
754. Cardoso R, Mendirichaga R, Fernandes G, Healy C, Lambrakos LK, Viles-
Gonzalez JF, Goldberger JJ, Mitrani RD. Cryoballoon versus radiofrequency
catheter ablation in atrial fibrillation: a meta-analysis. J Cardiovasc Electrophysiol
2016;27:11511159.
755. Kabunga P, Phan K, Ha H, Sy RW. Meta-analysis of contemporary atrial fibrilla-
tion ablation strategies: irrigated radiofrequency versus duty-cycled phased
radiofrequency versus cryoballoon ablation. JACC Clin Electrophysiol
2016;2:377390.
756. Bollmann A, Ueberham L, Schuler E, Wiedemann M, Reithmann C, Sause A,
Tebbenjohanns J, Schade A, Shin DI, Staudt A, Zacharzowsky U, Ulbrich M,
Wetzel U, Neuser H, Bode K, Kuhlen R, Hindricks G. Cardiac tamponade in
catheter ablation of atrial fibrillation: German-wide analysis of 21 141 proce-
dures in the Helios atrial fibrillation ablation registry (SAFER). Europace
2018;20:19441951.
757. Ueberham L, Schuler E, Hindricks G, Kuhlen R, Bollmann A. SAFER. Eur Heart J
2018;39:20232024.
758. Hummel J, Michaud G, Hoyt R, DeLurgio D, Rasekh A, Kusumoto F, Giudici M,
Dan D, Tschopp D, Calkins H, Boersma L; TTOP-AF Investigators. Phased RF
ablation in persistent atrial fibrillation. Heart Rhythm 2014;11:202209.
759. Boersma LV, van der Voort P, Debruyne P, Dekker L, Simmers T,
Rossenbacker T, Balt J, Wijffels M, Degreef Y. Multielectrode pulmonary vein
isolation versus single tip wide area catheter ablation for paroxysmal atrial fibril-
lation: a multinational multicenter randomized clinical trial. Circ Arrhythm
Electrophysiol 2016;9:e003151.
760. Nagashima K, Okumura Y, Watanabe I, Nakahara S, Hori Y, Iso K, Watanabe R,
Arai M, Wakamatsu Y, Kurokawa S, Mano H, Nakai T, Ohkubo K, Hirayama A.
Hot balloon versus cryoballoon ablation for atrial fibrillation: lesion characteris-
tics and middle-term outcomes. Circ Arrhythm Electro physiol 2018;11:e005861.
761. Ucer E, Janeczko Y, Seegers J, Fredersdorf S, Friemel S, Poschenrieder F, Maier
LS, Jungbauer CG. A RAndomized Trial to compare the acute reconnection
after pulmonary vein ISolation with Laser-BalloON versus radiofrequency
Ablation: RATISBONA trial. J Cardiovasc Electrophysiol 2018;29:733739.
762. De Greef Y, Stroker E, Schwagten B, Kupics K, De Cocker J, Chierchia GB, de
Asmundis C, Stockman D, Buysschaert I. Complications of pulmonary vein iso-
lation in atrial fibrillation: predictors and comparison between four different
ablation techniques: results from the Middelheim PVI-registry. Europace
2018;20:12791286.
ESC Guidelines 105

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
763. Steinbeck G, Sinner MF, Lutz M, Muller-Nurasyid M, Kaab S, Reinecke H.
Incidence of complications related to catheter ablation of atrial fibrillation and
atrial flutter: a nationwide in-hospital analysis of administrative data for
Germany in 2014. Eur Heart J 2018;39:40204029.
764. Fink T, Metzner A, Willems S, Eckardt L, Ince H, Brachmann J, Spitzer SG,
Deneke T, Schmitt C, Hochadel M, Senges J, Rillig A. Procedural success, safety
and patients satisfaction after second ablation of atrial fibrillation in the elderly:
results from the German ablation registry. Clin Res Cardiol
2019;108:13541363.
765. Szegedi N, Szeplaki G, Herczeg S, Tahin T, Sallo Z, Nagy VK, Osztheimer I,
Ozcan EE, Merkely B, Geller L. Repeat procedure is a new independent predic-
tor of complications of atrial fibrillation ablation. Europace 2019;21:732737.
766. Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, Kim YH, Klein
G, Natale A, Packer D, Skanes A, Ambrogi F, Biganzoli E. Updated worldwide
survey on the methods, efficacy, and safety of catheter ablation for human atrial
fibrillation. Circ Arrhythm Electrophysiol 2010;3:3238.
767. Lee G, Sparks PB, Morton JB, Kistler PM, Vohra JK, Medi C, Rosso R, Teh A,
Halloran K, Kalman JM. Low risk of major complications associated with pulmo-
nary vein antral isolation for atrial fibrillation: results of 500 consecutive abla-
tion procedures in patients with low prevalence of structural heart disease
from a single center. J Cardiovasc Electrophysiol 2011;22:163168.
768. Deshmukh A, Patel NJ, Pant S, Shah N, Chothani A, Mehta K, Grover P, Singh
V, Vallurupalli S, Savani GT, Badheka A, Tuliani T, Dabhadkar K, Dibu G, Reddy
YM, Sewani A, Kowalski M, Mitrani R, Paydak H, Viles-Gonzalez JF. In-hospital
complications associated with catheter ablation of atrial fibrillation in the
United States between 2000 and 2010: analysis of 93 801 procedures.
Circulation 2013;128:21042112.
769. Tripathi B, Arora S, Kumar V, Abdelrahman M, Lahewala S, Dave M, Shah M,
Tan B, Savani S, Badheka A, Gopalan R, Shantha GPS, Viles-Gonzalez J,
Deshmukh A. Temporal trends of in-hospital complications associated with
catheter ablation of atrial fibrillation in the United States: an update from
Nationwide Inpatient Sample database (20112014). J Cardiovasc Electrophysiol
2018;29:715724.
770. Voskoboinik A, Sparks PB, Morton JB, Lee G, Joseph SA, Hawson JJ, Kistler PM,
Kalman JM. Low rates of major complications for radiofrequency ablation of
atrial fibrillation maintained over 14 years: a single centre experience of 2750
consecutive cases. Heart Lung Circ 2018;27:976983.
771. Berger WR, Meulendijks ER, Limpens J, van den Berg NWE, Neefs J, Driessen
AHG, Krul SPJ, van Boven WJP, de Groot JR. Persistent atrial fibrillation: a sys-
tematic review and meta-analysis of invasive strategies. Int J Cardiol
2019;278:137143.
772. Shah AN, Mittal S, Sichrovsky TC, Cotiga D, Arshad A, Maleki K, Pierce WJ,
Steinberg JS. Long-term outcome following successful pulmonary vein isolation:
pattern and prediction of very late recurrence. J Cardiovasc Electrophysiol
2008;19:661667.
773. Sawhney N, Anousheh R, Chen WC, Narayan S, Feld GK. Five-year outcomes
after segmental pulmonary vein isolation for paroxysmal atrial fibrillation. Am J
Cardiol 2009;104:366372.
774. Ouyang F, Tilz R, Chun J, Schmidt B, Wissner E, Zerm T, Neven K, Kokturk B,
Konstantinidou M, Metzner A, Fuernkranz A, Kuck KH. Long-term results of
catheter ablation in paroxysmal atrial fibrillation: lessons from a 5-year follow-
up. Circulation 2010;
122:23682377.
775. Bertaglia E, Tondo C, De Simone A, Zoppo F, Mantica M, Turco P, Iuliano A,
Forleo G, La Rocca V, Stabile G. Does catheter ablation cure atrial fibrillation?
Single-procedure outcome of drug-refractory atrial fibrillation ablation: a 6-year
multicentre experience. Europace 2010;12:181187.
776. Weerasooriya R, Khairy P, Litalien J, Macle L, Hocini M, Sacher F, Lellouche N,
Knecht S, Wright M, Nault I, Miyazaki S, Scavee C, Clementy J, Haissaguerre M,
Jais P. Catheter ablation for atrial fibrillation: are results maintained at 5 years of
follow-up?J Am Coll Cardiol 2011;57:160166.
777. Medi C, Sparks PB, Morton JB, Kistler PM, Halloran K, Rosso R, Vohra JK,
Kumar S, Kalman JM. Pulmonary vein antral isolation for paroxysmal atrial fibril-
lation: results from long-term follow-up. J Cardiovasc Electrophysiol
2011;22:137141.
778. Schreiber D, Rostock T, Frohlich M, Sultan A, Servatius H, Hoffmann BA, Luker
J, Berner I, Schaffer B, Wegscheider K, Lezius S, Willems S, Steven D. Five-year
follow-up after catheter ablation of persistent atrial fibrillation using the step-
wise approach and prognostic factors for success. Circ Arrhythm Electrophysiol
2015;8:308317.
779. Scherr D, Khairy P, Miyazaki S, Aurillac-Lavignolle V, Pascale P, Wilton SB,
Ramoul K, Komatsu Y, Roten L, Jadidi A, Linton N, Pedersen M, Daly M,
O’Neill M, Knecht S, Weerasooriya R, Rostock T, Manninger M, Cochet H,
Shah AJ, Yeim S, Denis A, Derval N, Hocini M, Sacher F, Haissaguerre M, Jais P.
Five-year outcome of catheter ablation of persistent atrial fibrillation using ter-
mination of atrial fibrillation as a procedural endpoint. Circ Arrhythm
Electrophysiol 2015;8:1824.
780. Bertaglia E, Senatore G, De Michieli L, De Simone A, Amellone C, Ferretto S,
La Rocca V, Giuggia M, Corrado D, Zoppo F, Stabile G. Twelve-year follow-up
of catheter ablation for atrial fibrillation: a prospective, multicenter, randomized
study. Heart Rhythm 2017;14:486492.
781. Skelly A, Hashimoto R, Al-Khatib S, et alet alCatheter Ablation for Treatment of
Atrial Fibrillation [Internet]. Rockville, MD: Agency for Healthcare Research and
Quality (US). Available from https://www.ncbi.nlm.nih.gov/books/NBK305763/
(accessed 20 April 2015).
782. Zheng YR, Chen ZY, Ye LF, Wang LH. Long-term stroke rates after catheter
ablation or antiarrhythmic drug therapy for atrial fibrillation: a meta-analysis of
randomized trials. J Geriatr Cardiol 2015;12:507514.
783. Reynolds MR, Walczak J, White SA, Cohen DJ, Wilber DJ. Improvements in
symptoms and quality of life in patients with paroxysmal atrial fibrillation
treated with radiofrequency catheter ablation versus antiarrhythmic drugs. Circ
Cardiovasc Qual Outcomes 2010;3:615623.
784. Walfridsson H, Walfridsson U, Nielsen JC, Johannessen A, Raatikainen P, Janzon
M, Levin LA, Aronsson M, Hindricks G, Kongstad O, Pehrson S, Englund A,
Hartikainen J, Mortensen LS, Hansen PS. Radiofrequency ablation as initial ther-
apy in paroxysmal atrial fibrillation: results on health-related quality of life and
symptom burden. The MANTRA-PAF trial. Europace 2015;17:215221.
785. De Greef Y, Schwagten B, Chierchia GB, de Asmundis C, Stockman D,
Buysschaert I. Diagnosis-to-ablation time as a predictor of success: early choice
for pulmonary vein isolation and long-term outcome in atrial fibrillation: results
from the Middelheim-PVI registry. Europace 2018;20
:589595.
786. Wong CX, Abed HS, Molaee P, Nelson AJ, Brooks AG, Sharma G, Leong
DP, Lau DH, Middeldorp ME, Roberts-Thomson KC, Wittert GA,
Abhayaratna WP, Worthley SG, Sanders P. Pericardial fat is associated with
atrial fibrillation severity and ablation outcome. J Am Coll Cardiol
2011;57:17451751.
787. Kang JH, Lee DI, Kim S, Kim MN, Park YM, Ban JE, Choi JI, Lim HE, Park SW,
Kim YH. Prediction of long-term outcomes of catheter ablation of persistent
atrial fibrillation by parameters of preablation DC cardioversion. J Cardiovasc
Electrophysiol 2012;23:11651170.
788. Mahajan R, Lau DH, Brooks AG, Shipp NJ, Manavis J, Wood JPM, Finnie JW,
Samuel CS, Royce SG, Twomey DJ, Thanigaimani S, Kalman JM, Sanders P.
Electrophysiological, electroanatomical, and structural remodeling of the atria
as consequences of sustained obesity. J Am Coll Cardiol 2015;66:111.
789. Winkle RA, Mead RH, Engel G, Kong MH, Fleming W, Salcedo J, Patrawala RA.
Impact of obesity on atrial fibrillation ablation: patient characteristics, long-term
outcomes, and complications. Heart Rhythm 2017;14:819827.
790. De Maat GE, Mulder B, Berretty WL, Al-Jazairi MIH, Tan YES, Wiesfeld ACP,
Mariani MA, Van Gelder IC, Rienstra M, Blaauw Y. Obesity is associated with
impaired long-term success of pulmonary vein isolation: a plea for risk factor
management before ablation. Open Heart 2018;5:e000771.
791. Glover BM, Hong KL, Dagres N, Arbelo E, Laroche C, Riahi S, Bertini M,
Mikhaylov EN, Galvin J, Kiliszek M, Pokushalov E, Kautzner J, Calvo N,
Blomstrom-Lundqvist C, Brugada J; ESC-EHRA Atrial Fibrillation Ablation Long-
Term Registry Investigators. Impact of body mass index on the outcome of
catheter ablation of atrial fibrillation. Heart 2019;105:244250.
792. Chang SL, Tuan TC, Tai CT, Lin YJ, Lo LW, Hu YF, Tsao HM, Chang CJ, Tsai
WC, Chen SA. Comparison of outcome in catheter ablation of atrial fibrillation
in patients with versus without the metabolic syndrome. Am J Cardiol
2009;103:6772.
793. Tang RB, Dong JZ, Liu XP, Long DY, Yu RH, Kalifa J, Ma CS. Metabolic syn-
drome and risk of recurrence of atrial fibrillation after catheter ablation. Circ J
2009;73:438443.
794. Mohanty S, Mohanty P, Di Biase L, Bai R, Pump A, Santangeli P, Burkhardt D,
Gallinghouse JG, Horton R, Sanchez JE, Bailey S, Zagrodzky J, Natale A. Impact
of metabolic syndrome on procedural outcomes in patients with atrial fibrilla-
tion undergoing catheter ablation. J Am Coll Cardiol 2012;59:12951301.
795. Mulder AA, Wijffels MC, Wever EF, Kelder JC, Boersma LV. Arrhythmia detec-
tion after atrial fibrillation ablation: value of incremental monitoring time. Pacing
Clin Electrophysiol 2012;35:164169.
796. Steven D, Rostock T, Lutomsky B, Klemm H, Servatius H, Drewitz I, Friedrichs
K, Ventura R, Meinertz T, Willems S. What is the real atrial fibrillation burden
after catheter ablation of atrial fibrillation? A prospective rhythm analysis in
pacemaker patients with continuous atrial monitoring. Eur Heart J
2008;29:10371042.
797. Kaitani K, Inoue K, Kobori A, Nakazawa Y, Ozawa T, Kurotobi T, Morishima I,
Miura F, Watanabe T, Masuda M, Naito M, Fujimoto H, Nishida T, Furukawa Y,
Shirayama T, Tanaka M, Okajima K, Yao T, Egami Y, Satomi K, Noda T,
Miyamoto K, Haruna T, Kawaji T, Yoshizawa T, Toyota T, Yahata M, Nakai K,
Sugiyama H, Higashi Y, Ito M, Horie M, Kusano KF, Shimizu W, Kamakura S,
Morimoto T, Kimura T, Shizuta S; EAST-AF Trial Investigators. Efficacy of
Antiarrhythmic Drugs Short-Term Use After Catheter Ablation for Atrial
Fibrillation (EAST-AF) trial. Eur Heart J 2016;37:610618.
106 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
798. Willems S, Khairy P, Andrade JG, Hoffmann BA, Levesque S, Verma A,
Weerasooriya R, Novak P, Arentz T, Deisenhofer I, Rostock T, Steven D,
Rivard L, Guerra PG, Dyrda K, Mondesert B, Dubuc M, Thibault B, Talajic M,
Roy D, Nattel S, Macle L, ADVICE Trial Investigators. Redefining the
blanking period after catheter ablation for paroxysmal atrial fibrillation: insights
from the ADVICE (Adenosine Following Pulmonary Vein Isolation to Target
Dormant Conduction Elimination) trial. Circ Arrhythm Electrophysiol 2016;9:
e003909.
799. Klemm HU, Ventura R, Rostock T, Brandstrup B, Risius T, Meinertz T, Willems
S. Correlation of symptoms to ECG diagnosis following atrial fibrillation abla-
tion. J Cardiovasc Electrophysiol 2006;17:146150.
800. Vasamreddy CR, Dalal D, Dong J, Cheng A, Spragg D, Lamiy SZ, Meininger G,
Henrikson CA, Marine JE, Berger R, Calkins H. Symptomatic and asymptomatic
atrial fibrillation in patients undergoing radiofrequency catheter ablation. J
Cardiovasc Electrophysiol 2006;17:134139.
801. Oral H, Veerareddy S, Good E, Hall B, Cheung P, Tamirisa K, Han J, Fortino J,
Chugh A, Bogun F, Pelosi F Jr, Morady F. Prevalence of asymptomatic recur-
rences of atrial fibrillation after successful radiofrequency catheter ablation. J
Cardiovasc Electrophysiol 2004;15:920924.
802. Hindricks G, Piorkowski C, Tanner H, Kobza R, Gerds-Li JH, Carbucicchio C,
Kottkamp H. Perception of atrial fibrillation before and after radiofrequency
catheter ablation: relevance of asymptomatic arrhythmia recurrence. Circulation
2005;112:307313.
803. Senatore G, Stabile G, Bertaglia E, Donnici G, De Simone A, Zoppo F, Turco P,
Pascotto P, Fazzari M. Role of transtelephonic electrocardiographic monitoring
in detecting short-term arrhythmia recurrences after radiofrequency ablation in
patients with atrial fibrillation. J Am Coll Cardiol 2005;45:873876.
804. Roux JF, Zado E, Callans DJ, Garcia F, Lin D, Marchlinski FE, Bala R, Dixit S,
Riley M, Russo AM, Hutchinson MD, Cooper J, Verdino R, Patel V, Joy PS,
Gerstenfeld EP. Antiarrhythmics After Ablation of Atrial Fibrillation (5A Study).
Circulation 2009;120:10361040.
805. Duytschaever M, Demolder A, Phlips T, Sarkozy A, El Haddad M, Taghji P,
Knecht S, Tavernier R, Vandekerckhove Y, De Potter T. PulmOnary vein isola-
tion With vs. without continued antiarrhythmic Drug trEatment in subjects
with Recurrent Atrial Fibrillation (POWDER AF): results from a multicentre
randomized trial. Eur Heart J 2018;39:14291437.
806. Mardigyan V, Verma A, Birnie D, Guerra P, Redfearn D, Becker G, Champagne
J, Sapp J, Gula L, Parkash R, Macle L, Crystal E, O’Hara G, Khaykin Y, Sturmer
M, Veenhuyzen GD, Greiss I, Sarrazin JF, Mangat I, Novak P, Skanes A, Roux JF,
Chauhan V, Hadjis T, Morillo CA, Essebag V. Anticoagulation management pre-
and post atrial fibrillation ablation: a survey of Canadian centres. Can J Cardiol
2013;29:219223.
807. Nakahara S, Hori Y, Kobayashi S, Sakai Y, Taguchi I, Takayanagi K, Nagashima K,
Sonoda K, Kogawa R, Sasaki N, Watanabe I, Okumura Y. Epicardial adipose
tissue-based defragmentation approach to persistent atrial fibrillation: its impact
on complex fractionated electrograms and ablation outcome. Heart Rhythm
2014;11:13431351.
808. Chao TF, Hung CL, Tsao HM, Lin YJ, Yun CH, Lai YH, Chang SL, Lo LW, Hu
YF, Tuan TC, Chang HY, Kuo JY, Yeh HI, Wu TJ, Hsieh MH, Yu WC, Chen SA.
Epicardial adipose tissue thickness and ablation outcome of atrial fibrillation.
PLoS One 2013;8:e74926.
809. Masuda M, Mizuno H, Enchi Y, Minamiguchi H, Konishi S, Ohtani T, Yamaguchi
O, Okuyama Y, Nanto S, Sakata Y. Abundant epicardial adipose tissue sur-
rounding the left atrium predicts early rather than late recurrence of atrial fibril-
lation after catheter ablation. J Interv Card Electrophysiol 2015;44:3137.
810. Sepehri Shamloo A, Dagres N, Dinov B, Sommer P, Husser-Bollmann D,
Bollmann A, Hindricks G, Arya A. Is epicardial fat tissue associated with atrial
fibrillation recurrence after ablation? A systematic review and meta-analysis. Int
J Cardiol Heart Vasc 2019;22:132138.
811. Blanche C, Tran N, Rigamonti F, Burri H, Zimmermann M. Value of P-wave sig-
nal averaging to predict atrial fibrillation recurrences after pulmonary vein isola-
tion. Europace 2013;15:198204.
812. Bhargava M, Di Biase L, Mohanty P, Prasad S, Martin DO, Williams-Andrews M,
Wazni OM, Burkhardt JD, Cummings JE, Khaykin Y, Verma A, Hao S, Beheiry S,
Hongo R, Rossillo A, Raviele A, Bonso A, Themistoclakis S, Stewart K, Saliba
WI, Schweikert RA, Natale A. Impact of type of atrial fibrillation and repeat
catheter ablation on long-term freedom from atrial fibrillation: results from a
multicenter study. Heart Rhythm 2009;6:14031412.
813. Winkle RA, Mead RH, Engel G, Patrawala RA. Long-term results of atrial fibrilla-
tion ablation: the importance of all initial ablation failures undergoing a repeat
ablation. Am Heart J 2011;162:193200.
814. Mohanty S, Mohanty P, DIB L, Bai R, Trivedi C, Santangeli P, Santoro F, Hongo
R, Hao S, Beheiry S, Burkhardt D, Gallinghouse JG, Horton R, Sanchez JE, Bailey
S, Hranitzky PM, Zagrodzky J, Natale A. Long-term outcome of catheter abla-
tion in atrial fibrillation patients with coexistent metabolic syndrome and
obstructive sleep apnea: impact of repeat procedures versus lifestyle changes. J
Cardiovasc Electrophysiol 2014;25:930938.
815. Ejima K, Shoda M, Arai K, Suzuki A, Yagishita D, Yagishita Y, Yashiro B, Sato T,
Manaka T, Ashihara K, Hagiwara N. Impact of diastolic dysfunction on the out-
come of catheter ablation in patients with atrial fibrillation. Int J Cardiol
2013;164:8893.
816. Hocini M, Sanders P, Deisenhofer I, Jais P, Hsu LF, Scavee C, Weerasoriya R,
Raybaud F, Macle L, Shah DC, Garrigue S, Le Metayer P, Clementy J,
Haissaguerre M. Reverse remodeling of sinus node function after catheter abla-
tion of atrial fibrillation in patients with prolonged sinus pauses. Circulation
2003;108:11721175.
817. Chen YW, Bai R, Lin T, Salim M, Sang CH, Long DY, Yu RH, Tang RB, Guo XY,
Yan XL, Nie JG, Du X, Dong JZ, Ma CS. Pacing or ablation: which is better for
paroxysmal atrial fibrillation-related tachycardia-bradycardia syndrome?Pacing
Clin Electrophysiol 2014;37:403411.
818. Inada K, Yamane T, Tokutake K, Yokoyama K, Mishima T, Hioki M, Narui R, Ito
K, Tanigawa S, Yamashita S, Tokuda M, Matsuo S, Shibayama K, Miyanaga S,
Date T, Sugimoto K, Yoshimura M. The role of successful catheter ablation in
patients with paroxysmal atrial fibrillation and prolonged sinus pauses: outcome
during a 5-year follow-up. Europace 2014;16:208213.
819. Cummings JE, Schweikert R, Saliba W, Hao S, Martin DO, Marrouche NF,
Burkhardt JD, Kilicaslan F, Verma A, Beheiry S, Belden W, Natale A. Left atrial
flutter following pulmonary vein antrum isolation with radiofrequency energy:
linear lesions or repeat isolation. J Cardiovasc Electrophysiol 2005;16:293297.
820. Schneider R, Lauschke J, Tischer T, Schneider C, Voss W, Moehlenkamp F,
Glass A, Diedrich D, Bansch D. Pulmonary vein triggers play an important role
in the initiation of atrial flutter: initial results from the prospective randomized
Atrial Fibrillation Ablation in Atrial Flutter (Triple A) trial. Heart Rhythm
2015;12:865
871.
821. Patel NJ, Deshmukh A, Pau D, Goyal V, Patel SV, Patel N, Agnihotri K,
Asirvatham S, Noseworthy P, Di Biase L, Natale A, Viles-Gonzalez JF.
Contemporary utilization and safety outcomes of catheter ablation of atrial flut-
ter in the United States: analysis of 89,638 procedures. Heart Rhythm
2016;13:13171325.
822. Cox JL, Schuessler RB, Boineau JP. The development of the maze procedure for
the treatment of atrial fibrillation. Semin Thorac Cardiovasc Surg 2000;12:214.
823. Melby SJ, Zierer A, Bailey MS, Cox JL, Lawton JS, Munfakh N, Crabtree TD,
Moazami N, Huddleston CB, Moon MR, Damiano RJ Jr. A new era in the surgi-
cal treatment of atrial fibrillation: the impact of ablation technology and lesion
set on procedural efficacy. Ann Surg 2006;244:583592.
824. Badhwar V, Rankin JS, Damiano RJ, Jr., Gillinov AM, Bakaeen FG, Edgerton JR,
Philpott JM, McCarthy PM, Bolling SF, Roberts HG, Thourani VH, Suri RM,
Shemin RJ, Firestone S, Ad N. The Society of Thoracic Surgeons 2017 Clinical
Practice Guidelines for the surgical treatment of atrial fibrillation. Ann Thorac
Surg 2017;103:329341.
825. Belley-Cote EP, Singal RK, McClure G, Devereaux K, Brady K, An K, Healey JS,
Connolly SJ, Whitlock RP. Perspective and practice of surgical atrial fibrillation
ablation: an international survey of cardiac surgeons. Europace
2019;21:445450.
826. Barnett SD, Ad N. Surgical ablation as treatment for the elimination of atrial
fibrillation: a meta-analysis. J Thorac Cardiovasc Surg 2006;131:10291035.
827. McClure GR, Belley-Cote EP, Jaffer IH, Dvirnik N, An KR, Fortin G, Spence J,
Healey J, Singal RK, Whitlock RP. Surgical ablation of atrial fibrillation: a system-
atic review and meta-analysis of randomized controlled trials. Europace
2018;20:14421450.
828. Osmancik P, Budera P, Talavera D, Hlavicka J, Herman D, Holy J, Cervinka P,
Smid J, Hanak P, Hatala R, Widimsky P. Five-year outcomes in cardiac surgery
patients with atrial fibrillation undergoing concomitant surgical ablation versus
no ablation. The long-term follow-up of the PRAGUE-12 study. Heart Rhythm
201916:13341340.
829. Sharples L, Everett C, Singh J, Mills C, Spyt T, Abu-Omar Y, Fynn S, Thorpe B,
Stoneman V, Goddard H, Fox-Rushby J, Nashef S. Amaze: a double-blind, multi-
centre randomised controlled trial to investigate the clinical effectiveness and
cost-effectiveness of adding an ablation device-based maze procedure as an
adjunct to routine cardiac surgery for patients with pre-existing atrial fibrilla-
tion. Health Technol Assess 2018;22:1132.
830. Bagge L, Probst J, Jensen SM, Blomstrom P, Thelin S, Holmgren A, Blomstrom-
Lundqvist C. Quality of life is not improved after mitral valve surgery combined
with epicardial left atrial cryoablation as compared with mitral valve surgery
alone: a substudy of the double blind randomized SWEDish Multicentre Atrial
Fibrillation study (SWEDMAF). Europace 2018;20:f343f350.
831. Suwalski P, Kowalewski M, Jasinski M, Staromlynski J, Zembala M, Widenka K,
Brykczynski M, Skiba J, Zembala MO, Bartus K, Hirnle T, Dziembowska I, Deja
M, Tobota Z, Maruszewski BJ. Surgical ablation for atrial fibrillation during iso-
lated coronary artery bypass surgery. Eur J Cardiothorac Surg 2019.
ESC Guidelines 107

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
832. Suwalski P, Kowalewski M, Jasinski M, Staromlynski J, Zembala M, Widenka K,
Brykczynski M, Skiba J, Zembala MO, Bartus K, Hirnle T, Dziembowska I,
Tobota Z, Maruszewski BJ; KROK Investigators. Survival after surgical ablation
for atrial fibrillation in mitral valve surgery: analysis from the Polish National
Registry of Cardiac Surgery Procedures (KROK). J Thorac Cardiovasc Surg 2018;
doi: 10.1016/j.jtcvs.2018.07.099.
833. Gillinov AM, Bakaeen F, McCarthy PM, Blackstone EH, Rajeswaran J, Pettersson
G, Sabik JF 3rd, Najam F, Hill KM, Svensson LG, Cosgrove DM, Marrouche N,
Natale A. Surgery for paroxysmal atrial fibrillation in the setting of mitral valve
disease: a role for pulmonary vein isolation? Ann Thorac Surg 2006;81:1926;
discussion 2728.
834. Basu S, Nagendran M, Maruthappu M. How effective is bipolar radiofrequency
ablation for atrial fibrillation during concomitant cardiac surgery?Interact
Cardiovasc Thorac Surg 2012;15:741748.
835. Gillinov AM, Bhavani S, Blackstone EH, Rajeswaran J, Svensson LG, Navia JL,
Pettersson BG, Sabik JF, 3rd, Smedira NG, Mihaljevic T, McCarthy PM,
Shewchik J, Natale A. Surgery for permanent atrial fibrillation: impact of patient
factors and lesion set. Ann Thorac Surg 2006;82:502513; discussion 513514.
836. Beukema WP, Sie HT, Misier AR, Delnoy PP, Wellens HJ, Elvan A. Predictive
factors of sustained sinus rhythm and recurrent atrial fibrillation after a radiofre-
quency modified maze procedure. Eur J Cardiothorac Surg 2008;34:771775.
837. Lee SH, Kim JB, Cho WC, Chung CH, Jung SH, Choo SJ, Lee JW. The influence
of age on atrial fibrillation recurrence after the maze procedure in patients with
giant left atrium. J Thorac Cardiovasc Surg 2011;141:1015 1019.
838. Damiano RJ Jr, Schwartz FH, Bailey MS, Maniar HS, Munfakh NA, Moon MR,
Schuessler RB. The Cox maze IV procedure: predictors of late recurrence. J
Thorac Cardiovasc Surg 2011;141:113121.
839. Sunderland N, Maruthappu M, Nagendran M. What size of left atrium signifi-
cantly impairs the success of maze surgery for atrial fibrillation?Interact
Cardiovasc Thorac Surg 2011;13:332338.
840. Bakker RC, Akin S, Rizopoulos D, Kik C, Takkenberg JJ, Bogers AJ. Results of
clinical application of the modified maze procedure as concomitant surgery.
Interact Cardiovasc Thorac Surg 2013;16:151156.
841. Ad N, Holmes SD. Prediction of sinus rhythm in patients undergoing concomi-
tant Cox maze procedure through a median sternotomy. J Thorac Cardiovasc
Surg 2014;148:881886.
842. Blomstrom-Lundqvist C, Johansson B, Berglin E, Nilsson L, Jensen SM, Thelin S,
Holmgren A, Edvardsson N, Kallner G, Blomstrom P. A randomized double-
blind study of epicardial left atrial cryoablation for permanent atrial fibrillation
in patients undergoing mitral valve surgery: the SWEDish Multicentre Atrial
Fibrillation study (SWEDMAF). Eur Heart J 2007;28:29022908.
843. Huffman MD, Karmali KN, Berendsen MA, Andrei AC, Kruse J, McCarthy PM,
Malaisrie SC. Concomitant atrial fibrillation surgery for people undergoing car-
diac surgery. Cochrane Database Syst Rev 2016:CD011814.
844. Budera P, Straka Z, Osmancik P, Vanek T, Jelinek S, Hlavicka J, Fojt R, Cervinka
P, Hulman M, Smid M, Maly M, Widimsky P. Comparison of cardiac surgery
with left atrial surgical ablation vs. cardiac surgery without atrial ablation in
patients with coronary and/or valvular heart disease plus atrial fibrillation: final
results of the PRAGUE-12 randomized multicentre study. Eur Heart J
2012;33:26442652.
845. Wang JG, Xin M, Han J, Li Y, Luo TG, Wang J, Meng F, Meng X. Ablation in
selective patients with long-standing persistent atrial fibrillation: medium-term
results of the Dallas lesion set. Eur J Cardiothorac Surg 2014;46:213220.
846. Badhwar V, Rankin JS, Ad N, Grau-Sepulveda M, Damiano RJ, Gillinov AM,
McCarthy PM, Thourani VH, Suri RM, Jacobs JP, Cox JL. Surgical ablation of
atrial fibrillation in the United States: trends and propensity matched outcomes.
Ann Thorac Surg 2017;104:493500.
847. Joshibayev S, Bolatbekov B. Early and long-term outcomes and quality of life
after concomitant mitral valve surgery, left atrial size reduction, and radiofre-
quency surgical ablation of atrial fibrillation. Anatol J Cardiol 2016;16:797803.
848. Driessen AHG, Berger WR, Bierhuizen MFA, Piersma FR, van den Berg NWE,
Neefs J, Krul SPJ, van Boven WP, de Groot JR. Quality of life improves after
thoracoscopic surgical ablation of advanced atrial fibrillation: results of the
Atrial Fibrillation Ablation and Autonomic Modulation via Thoracoscopic
Surgery (AFACT) study. J Thorac Cardiovasc Surg 2018;155:972980.
849. Castella M, Kotecha D, van Laar C, Wintgens L, Castillo Y, Kelder J, Aragon D,
Nunez M, Sandoval E, Casellas A, Mont L, van Boven WJ, Boersma LVA, van
Putte BP. Thoracoscopic vs. catheter ablation for atrial fibrillation: long-term
follow-up of the FAST randomized trial. Europace 2019;21:746753.
850. Osmancik P, Budera P, Talavera D, Herman D, Vesela J, Prochazkova R, Rizov
V, Kacer P. Improvement in the quality of life of patients with persistent or
long-standing persistent atrial fibrillation after hybrid ablation. J Interv Card
Electrophysiol 2020;57:435442.
851. Kim HJ, Kim JS, Kim TS. Epicardial thoracoscopic ablation versus endocardial
catheter ablation for management of atrial fibrillation: a systematic review and
meta-analysis. Interact Cardiovasc Thorac Surg 2016;22:729 737.
852. Gammie JS, Haddad M, Milford-Beland S, Welke KF, Ferguson TB Jr, O’Brien
SM, Griffith BP, Peterson ED. Atrial fibrillation correction surgery: lessons from
the Society of Thoracic Surgeons National Cardiac Database. Ann Thorac Surg
2008;85:909914.
853. Calkins H, Kuck KH, Cappato R, Brugada J, Camm AJ, Chen SA, Crijns HJ,
Damiano RJ, Jr, Davies DW, DiMarco J, Edgerton J, Ellenbogen K, Ezekowitz
MD, Haines DE, Haissaguerre M, Hindricks G, Iesaka Y, Jackman W, Jalife J, Jais
P, Kalman J, Keane D, Kim YH, Kirchhof P, Klein G, Kottkamp H, Kumagai K,
Lindsay BD, Mansour M, Marchlinski FE, McCarthy PM, Mont JL, Morady F,
Nademanee K, Nakagawa H, Natale A, Nattel S, Packer DL, Pappone C,
Prystowsky E, Raviele A, Reddy V, Ruskin JN, Shemin RJ, Tsao HM, Wilber D.
2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical
ablation of atrial fibrillation: recommendations for patient selection, procedural
techniques, patient management and follow-up, definitions, endpoints, and
research trial design. Europace 2012;14:528606.
854. van der Heijden CAJ, Vroomen M, Luermans JG, Vos R, Crijns H, Gelsomino S,
La Meir M, Pison L, Maesen B. Hybrid versus catheter ablation in patients with
persistent and longstanding persistent atrial fibrillation: a systematic review and
meta-analysis. Eur J Cardiothorac Surg 2019;56:433443.
855. Velagic V, DEA C, Mugnai G, Irfan G, Hunuk B, Stroker E, Hacioglu E, Umbrain
V, Beckers S, Czapla J, Wellens F, Nijs J, Brugada P, M LAM, Chierchia GB.
Repeat procedures after hybrid thoracoscopic ablation in the setting of long-
standing persistent atrial fibrillation: electrophysiological findings and 2-year
clinical outcome. J Cardiovasc Electrophysiol 2016;27:4150.
856. Osmancik P, Budera P, Zdarska J, Herman D, Petr R, Straka Z.
Electrophysiological findings after surgical thoracoscopic atrial fibrillation abla-
tion. Heart Rhythm 2016;13:12461252.
857. Wang H, Han J, Wang Z, Yin Z, Liu Z, Jin Y, Han H. A prospective
randomized trial of the cut-and-sew maze procedure in patients undergoing
surgery for rheumatic mitral valve disease. J Thorac Cardiovasc Surg 2018;155:
608617.
858. Lawrance CP, Henn MC, Miller JR, Sinn LA, Schuessler RB, Maniar HS,
Damiano RJ Jr. A minimally invasive Cox maze IV procedure is as effective as
sternotomy while decreasing major morbidity and hospital stay. J Thorac
Cardiovasc Surg 2014;148:955961.
859. Weimar T, Schena S, Bailey MS, Maniar HS, Schuessler RB, Cox JL, Damiano RJ
Jr. The Cox-maze procedure for lone atrial fibrillation: a single-center experi-
ence over 2 decades. Circ Arrhythm Electrophysiol 2012;5:814.
860. Nuotio I, Hartikainen JE, Gronberg T, Biancari F, Airaksinen KE. Time to cardio-
version for acute atrial fibrillation and thromboembolic complications. JAMA
2014;312:647649.
861. Airaksinen KE, Gronberg T, Nuotio I, Nikkinen M, Ylitalo A, Biancari F,
Hartikainen JE. Thromboembolic complications after cardioversion of acute
atrial fibrillation: the FinCV (Finnish CardioVersion) study. J Am Coll Cardiol
2013;62:11871192.
862. Hansen ML, Jepsen RM, Olesen JB, Ruwald MH, Karasoy D, Gislason GH,
Hansen J, Kober L, Husted S, Torp-Pedersen C. Thromboembolic risk in 16
274 atrial fibrillation patients undergoing direct current cardioversion with and
without oral anticoagulant therapy. Europace 2015;17:1823.
863. Lip GY. Cardioversion of atrial fibrillation. Postgrad Med J 1995;71:457465.
864. Garg A, Khunger M, Seicean S, Chung MK, Tchou PJ. Incidence of throm-
boembolic complications within 30 days of electrical cardioversion per-
formed within 48 hours of atrial fibrillation onset. JACC Clin Electrophysiol
2016;2:487494.
865. Tampieri A, Cipriano V, Mucci F, Rusconi AM, Lenzi T, Cenni P. Safety of cardi-
oversion in atrial fibrillation lasting less than 48 h without post-procedural anti-
coagulation in patients at low cardioembolic risk. Intern Emerg Med
2018;13:8793.
866. Klein AL, Grimm RA, Murray RD, Apperson-Hansen C, Asinger RW, Black IW,
Davidoff R, Erbel R, Halperin JL, Orsinelli DA, Porter TR, Stoddard MF;
Assessment of Cardioversion Using Transesophageal Echocardiography
Investigators. Use of transesophageal echocardiography to guide cardioversion
in patients with atrial fibrillation. N Engl J Med 2001;344:14111420.
867. Stellbrink C, Nixdorff U, Hofmann T, Lehmacher W, Daniel WG, Hanrath P,
Geller C, Mugge A, Sehnert W, Schmidt-Lucke C, Schmidt-Lucke JA, Group
ACES. Safety and efficacy of enoxaparin compared with unfractionated heparin
and oral anticoagulants for prevention of thromboembolic complications in car-
dioversion of nonvalvular atrial fibrillation: the Anticoagulation in Cardioversion
using Enoxaparin (ACE) trial. Circulation 2004;109:9971003.
868. Cappato R, Ezekowitz MD, Klein AL, Camm AJ, Ma CS, Le Heuzey JY, Talajic
M, Scanavacca M, Vardas PE, Kirchhof P, Hemmrich M, Lanius V, Meng IL,
Wildgoose P, van Eickels M, Hohnloser SH; X-VERT Investigators. Rivaroxaban
vs. vitamin K antagonists for cardioversion in atrial fibrillation. Eur Heart J
2014;35:33463355.
869. Ezekowitz MD, Pollack CV Jr, Halperin JL, England RD, VanPelt Nguyen S,
Spahr J, Sudworth M, Cater NB, Breazna A, Oldgren J, Kirchhof P. Apixaban
108 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
compared to heparin/vitamin K antagonist in patients with atrial fibrillation
scheduled for cardioversion: the EMANATE trial. Eur Heart J
2018;39:29592971.
870. Goette A, Merino JL, Ezekowitz MD, Zamoryakhin D, Melino M, Jin J, Mercuri
MF, Grosso MA, Fernandez V, Al-Saady N, Pelekh N, Merkely B, Zenin S,
Kushnir M, Spinar J, Batushkin V, de Groot JR, Lip GY; ENSURE-AF investiga-
tors. Edoxaban versus enoxaparin-warfarin in patients undergoing cardioversion
of atrial fibrillation (ENSURE-AF): a randomised, open-label, phase 3b trial.
Lancet 2016;388:19952003.
871. Telles-Garcia N, Dahal K, Kocherla C, Lip GYH, Reddy P, Dominic P. Non-vita-
min K antagonists oral anticoagulants are as safe and effective as warfarin for
cardioversion of atrial fibrillation: a systematic review and meta-analysis. Int J
Cardiol 2018;268:143148.
872. Brunetti ND, Tarantino N, De Gennaro L, Correale M, Santoro F, Di Biase M.
Direct oral anti-coagulants compared to vitamin-K antagonists in cardioversion
of atrial fibrillation: an updated meta-analysis. J Thromb Thrombolysis
2018;45:550556.
873. Kotecha D, Pollack CV Jr, De Caterina R, Renda G, Kirchhof P. Direct oral anti-
coagulants halve thromboembolic events after cardioversion of AF compared
with warfarin. J Am Coll Cardiol 2018;72:19841986.
874. Itainen S, Lehto M, Vasankari T, Mustonen P, Kotamaki M, Numminen A,
Lahtela H, Bah A, Hartikainen J, Hekkala AM, Airaksinen JKE. Non-vitamin K
antagonist oral anticoagulants in atrial fibrillation patients undergoing elective
cardioversion. Europace 2018;20:565568.
875. Lip GY, Hammerstingl C, Marin F, Cappato R, Meng IL, Kirsch B, van Eickels M,
Cohen A; X-TRA study and CLOT-AF Registry Investigators. Left atrial throm-
bus resolution in atrial fibrillation or flutter: results of a prospective study with
rivaroxaban (X-TRA) and a retrospective observational registry providing base-
line data (CLOT-AF). Am Heart J 2016;178:126134.
876. Steinberg JS, Sadaniantz A, Kron J, Krahn A, Denny DM, Daubert J, Campbell
WB, Havranek E, Murray K, Olshansky B, O’Neill G, Sami M, Schmidt S, Storm
R, Zabalgoitia M, Miller J, Chandler M, Nasco EM, Greene HL. Analysis of
cause-specific mortality in the Atrial Fibrillation Follow-up Investigation of
Rhythm Management (AFFIRM) study. Circulation 2004;109:19731980.
877. Cardoso R, Knijnik L, Bhonsale A, Miller J, Nasi G, Rivera M, Blumer V, Calkins
H. An updated meta-analysis of novel oral anticoagulants versus vitamin K
antagonists for uninterrupted anticoagulation in atrial fibrillation catheter abla-
tion. Heart Rhythm 2018;15:107115.
878. Calkins H, Willems S, Gerstenfeld EP, Verma A, Schilling R, Hohnloser SH,
Okumura K, Serota H, Nordaby M, Guiver K, Biss B, Brouwer MA, Grimaldi M;
RE-CIRCUIT Investigators. Uninterrupted dabigatran versus warfarin for abla-
tion in atrial fibrillation. N Engl J Med 2017;376:16271636.
879. Cappato R, Marchlinski FE, Hohnloser SH, Naccarelli GV, Xiang J, Wilber DJ,
Ma CS, Hess S, Wells DS, Juang G, Vijgen J, Hugl BJ, Balasubramaniam R, De
Chillou C, Davies DW, Fields LE, Natale A; VENTURE-AF Investigators.
Uninterrupted rivaroxaban vs. uninterrupted vitamin K antagonists for catheter
ablation in non-valvular atrial fibrillation. Eur Heart J 2015;36:18051811.
880. Kirchhof P, Haeusler KG, Blank B, De Bono J, Callans D, Elvan A, Fetsch T, Van
Gelder IC, Gentlesk P, Grimaldi M, Hansen J, Hindricks G, Al-Khalidi HR,
Massaro T, Mont L, Nielsen JC, Nolker G, Piccini JP, De Potter T, Scherr D,
Schotten U, Themistoclakis S, Todd D, Vijgen J, Di Biase L. Apixaban in patients
at risk of stroke undergoing atrial fibrillation ablation. Eur Heart J
2018;39:29422955.
881. Hohnloser SH, Camm J, Cappato R, Diener HC, Heidbuchel H, Mont L, Morillo
CA, Abozguia K, Grimaldi M, Rauer H, Reimitz PE, Smolnik R, Monninghoff C,
Kautzner J. Uninterrupted edoxaban vs. vitamin K antagonists for ablation of
atrial fibrillation: the ELIMINATE-AF trial. Eur Heart J 2019;40:30133021.
882. European Heart Rhythm Association, European Association for Cardio-
Thoracic Surgery, Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst
S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B, Heidbuchel H, Alfieri
O, Angelini A, Atar D, Colonna P, De Caterina R, De Sutter J, Goette A,
Gorenek B, Heldal M, Hohloser SH, Kolh P, Le Heuzey JY, Ponikowski P,
Rutten FH. Guidelines for the management of atrial fibrillation: the Task Force
for the management of atrial fibrillation of the European Society of Cardiology
(ESC). Eur Heart J 2010;31:23692429.
883. Lafuente-Lafuente C, Longas-Tejero MA, Bergmann JF, Belmin J.
Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibril-
lation. Cochrane Database Syst Rev 2012:CD005049.
884. Valembois L, Audureau E, Takeda A, Jarzebowski W, Belmin J, Lafuente-
Lafuente C. Antiarrhythmics for maintaining sinus rhythm after cardioversion of
atrial fibrillation. Cochrane Database Syst Rev 2019;9:CD005049.
885. Nabauer M, Gerth A, Limbourg T, Schneider S, Oeff M, Kirchhof P, Goette A,
Lewalter T, Ravens U, Meinertz T, Breithardt G, Steinbeck G. The registry of
the German Competence NETwork on Atrial Fibrillation: patient characteristics
and initial management. Europace 2009;11:423434.
886. Darkner S, Chen X, Hansen J, Pehrson S, Johannessen A, Nielsen JB, Svendsen
JH. Recurrence of arrhythmia following short-term oral AMIOdarone after
CATheter ablation for atrial fibrillation: a double-blind, randomized, placebo-
controlled study (AMIO-CAT trial). Eur Heart J 2014;35:33563364.
887. Leong-Sit P, Roux JF, Zado E, Callans DJ, Garcia F, Lin D, Marchlinski FE, Bala R,
Dixit S, Riley M, Hutchinson MD, Cooper J, Russo AM, Verdino R, Gerstenfeld
EP. Antiarrhythmics After Ablation of Atrial Fibrillation (5A Study): six-month
follow-up study. Circ Arrhythm Electrophysiol 2011;4:1114.
888. Abed HS, Wittert GA, Leong DP, Shirazi MG, Bahrami B, Middeldorp ME,
Lorimer MF, Lau DH, Antic NA, Brooks AG, Abhayaratna WP, Kalman JM,
Sanders P. Effect of weight reduction and cardiometabolic risk factor manage-
ment on symptom burden and severity in patients with atrial fibrillation: a
randomized clinical trial. JAMA 2013;310:20502060.
889. Pathak RK, Middeldorp ME, Meredith M, Mehta AB, Mahajan R, Wong CX,
Twomey D, Elliott AD, Kalman JM, Abhayaratna WP, Lau DH, Sanders P. Long-
term effect of goal-directed weight management in an atrial fibrillation cohort: a
long-term follow-up study (LEGACY). J Am Coll Cardiol 2015;65:21592169.
890. Lafuente-Lafuente C, Valembois L, Bergmann JF, Belmin J. Antiarrhythmics for
maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane
Database Syst Rev 2015;3:CD005049.
891. Kochiadakis GE, Igoumenidis NE, Marketou ME, Kaleboubas MD, Simantirakis
EN, Vardas PE. Low dose amiodarone and sotalol in the treatment of recurrent,
symptomatic atrial fibrillation: a comparative, placebo controlled study. Heart
2000;84:251257.
892. Galperin J, Elizari MV, Chiale PA, Molina RT, Ledesma R, Scapin AO, Vazquez
Blanco M; GEFCA Investigators-GEMA Group. Efficacy of amiodarone for the
termination of chronic atrial fibrillation and maintenance of normal sinus
rhythm: a prospective, multicenter, randomized, controlled, double blind trial. J
Cardiovasc Pharmacol Ther 2001;6:341350.
893. Channer KS, Birchall A, Steeds RP, Walters SJ, Yeo WW, West JN, Muthusamy
R, Rhoden WE, Saeed BT, Batin P, Brooksby WP, Wilson I, Grant S. A random-
ized placebo-controlled trial of pre-treatment and short- or long-term mainte-
nance therapy with amiodarone supporting DC cardioversion for persistent
atrial fibrillation. Eur Heart J 2004;25:144150.
894. Singh SN, Singh BN, Reda DJ, Fye CL, Ezekowitz MD, Fletcher RD, Sharma SC,
Atwood JE, Jacobson AK, Lewis HD Jr, Antman EM, Falk RH, Lopez B, Tang
XC. Comparison of sotalol versus amiodarone in maintaining stability of sinus
rhythm in patients with atrial fibrillation (Sotalol-Amiodarone Fibrillation
Efficacy Trial [Safe-T]). Am J Cardiol 2003;92:468472.
895. Kochiadakis GE, Igoumenidis NE, Hamilos ME, Tzerakis PG, Klapsinos NC,
Chlouverakis GI, Vardas PE. Sotalol versus propafenone for long-term mainte-
nance of normal sinus rhythm in patients with recurrent symptomatic atrial
fibrillation. Am J Cardiol 2004;94:15631566.
896. Gulizia M, Mangiameli S, Orazi S, Chiaranda G, Piccione G, Di Giovanni N,
Colletti A, Pensabene O, Lisi F, Vasquez L, Grammatico A, Boriani G;
PITAGORA Study Investigators. A randomized comparison of amiodarone and
class IC antiarrhythmic drugs to treat atrial fibrillation in patients paced for sinus
node disease: the Prevention Investigation and Treatment: A Group for
Observation and Research on Atrial arrhythmias (PITAGORA) trial. Am Heart J
2008;155:100107.e1.
897. Freemantle N, Lafuente-Lafuente C, Mitchell S, Eckert L, Reynolds M. Mixed
treatment comparison of dronedarone, amiodarone, sotalol, flecainide, and
propafenone, for the management of atrial fibrillation. Europace
2011;13:329345.
898. Cadrin-Tourigny J, Wyse DG, Roy D, Blondeau L, Levesque S, Talajic M,
Andrade JG, Dubuc M, Thibault B, Guerra PG, Macle L, Rivard L, Khairy P.
Efficacy of amiodarone in patients with atrial fibrillation with and without left
ventricular dysfunction: a pooled analysis of AFFIRM and AF-CHF trials. J
Cardiovasc Electrophysiol 2014;25:13061313.
899. Massie BM, Fisher SG, Radford M, Deedwania PC, Singh BN, Fletcher RD, Singh
SN. Effect of amiodarone on clinical status and left ventricular function in
patients with congestive heart failure. CHF-STAT Investigators. Circulation
1996;93:21282134.
900. Singh SN, Fletcher RD, Fisher SG, Singh BN, Lewis HD, Deedwania PC, Massie
BM, Colling C, Lazzeri D. Amiodarone in patients with congestive heart failure
and asymptomatic ventricular arrhythmia. Survival trial of antiarrhythmic ther-
apy in congestive heart failure. N Engl J Med 1995;333:7782.
901. Zimetbaum P. Antiarrhythmic drug therapy for atrial fibrillation. Circulation
2012;125:381389.
902. Kirchhof P, Franz MR, Bardai A, Wilde AM. Giant T-U waves precede torsades
de pointes in long QT syndrome: a systematic electrocardiographic analysis in
patients with acquired and congenital QT prolongation. J Am Coll Card iol
2009;54:143149.
903. Orr CF, Ahlskog JE. Frequency, characteristics, and risk factors for amiodarone
neurotoxicity. Arch Neurol 2009;
66:865869.
ESC Guidelines 109

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
904. Lai SW, Lin CL, Liao KF, Lin CY. Amiodarone use and risk of acute pancreatitis:
a population-based case-control study. Heart Rhythm 2015;12:163166.
905. Epstein AE, Olshansky B, Naccarelli GV, Kennedy JI Jr, Murphy EJ, Goldschlager
N. Practical management guide for clinicians who treat patients with amiodar-
one. Am J Med 2016;129:468 475.
906. Basaria S, Cooper DS. Amiodarone and the thyroid. Am J Med
2005;118:706714.
907. Colby R, Geyer H. Amiodarone-induced pulmonary toxicity. JAAPA
2017;30:2326.
908. Van Gelder IC, Crijns HJ, Van Gilst WH, Van Wijk LM, Hamer HP, Lie KI.
Efficacy and safety of flecainide acetate in the maintenance of sinus rhythm after
electrical cardioversion of chronic atrial fibrillation or atrial flutter. Am J Cardiol
1989;64:13171321.
909. Anderson JL, Gilbert EM, Alpert BL, Henthorn RW, Waldo AL, Bhandari AK,
Hawkinson RW, Pritchett EL. Prevention of symptomatic recurrences of parox-
ysmal atrial fibrillation in patients initially tolerating antiarrhythmic therapy. A
multicenter, double-blind, crossover study of flecainide and placebo with trans-
telephonic monitoring. Flecainide Supraventricular Tachycardia Study Group.
Circulation 1989;80:15571570.
910. Stroobandt R, Stiels B, Hoebrechts R. Propafenone for conversion and prophy-
laxis of atrial fibrillation. Propafenone Atrial Fibrillation Trial Investigators. Am J
Cardiol 1997;79:418423.
911. Echt DS, Liebson PR, Mitchell LB, Peters RW, Obias-Manno D, Barker AH,
Arensberg D, Baker A, Friedman L, Greene HL, et alet alMortality and morbid-
ity in patients receiving encainide, flecainide, or placebo. The Cardiac
Arrhythmia Suppression Trial. N Engl J Med 1991;324:781788.
912. Flaker GC, Blackshear JL, McBride R, Kronmal RA, Halperin JL, Hart RG.
Antiarrhythmic drug therapy and cardiac mortality in atrial fibrillation. The
Stroke Prevention in Atrial Fibrillation Investigators. J Am Coll Cardiol
1992;20:527532.
913. Podrid PJ, Anderson JL. Safety and tolerability of long-term propafenone ther-
apy for supraventricular tachyarrhythmias. The Propafenone Multicenter Study
Group. Am J Cardiol 1996;78:430434.
914. Brembilla-Perrot B, Laporte F, Sellal JM, Schwartz J, Olivier A, Zinzius PY,
Manenti V, Beurrier D, Andronache M, Louis P, Selton O, de la Chaise AT, De
Chillou C. 1: 1 atrial-flutter. Prevalence and clinical characteristics. Int J Cardiol
2013;168:32873290.
915. Gao X, Guha A, Buck B, Patel D, Snider MJ, Boyd M, Afzal M, Badin A, Godara
H, Liu Z, Tyler J, Weiss R, Kalbfleisch S, Hummel J, Augostini R, Houmsse M,
Daoud EG. Initiation and outcomes with Class Ic antiarrhythmic drug therapy.
Indian Pacing Electrophysiol J 2018;18:6872.
916. Richiardi E, Gaita F, Greco C, Gaschino G, Comba Costa G, Rosettani E,
Brusca A. [Propafenone versus hydroquinidine in long-term pharmacological
prophylaxis of atrial fibrillation]. Cardiologia 1992;
37:123127.
917. Chimienti M, Cullen MT, Jr., Casadei G. Safety of long-term flecainide and prop-
afenone in the management of patients with symptomatic paroxysmal atrial
fibrillation: report from theFlecainide and Propafenone Italian Study
Investigators. Am J Cardiol 1996;77:60A75A.
918. Reimold SC, Cantillon CO, Friedman PL, Antman EM. Propafenone versus sota-
lol for suppression of recurrent symptomatic atrial fibrillation. Am J Cardiol
1993;71:558563.
919. Aliot E, Denjoy I. Comparison of the safety and efficacy of flecainide versus
propafenone in hospital out-patients with symptomatic paroxysmal atrial fibril-
lation/flutter. The Flecainide AF French Study Group. Am J Cardiol
1996;77:66A71A.
920. Bellandi F, Simonetti I, Leoncini M, Frascarelli F, Giovannini T, Maioli M, Dabizzi
RP. Long-term efficacy and safety of propafenone and sotalol for the mainte-
nance of sinus rhythm after conversion of recurrent symptomatic atrial fibrilla-
tion. Am J Cardiol 2001;88:640645.
921. Meinertz T, Lip GY, Lombardi F, Sadowski ZP, Kalsch B, Camez A, Hewkin A,
Eberle S; ERAFT Investigators. Efficacy and safety of propafenone sustained
release in the prophylaxis of symptomatic paroxysmal atrial fibrillation (The
European Rythmol/Rytmonorm Atrial Fibrillation Trial [ERAFT] Study). Am J
Cardiol 2002;90:13001306.
922. Pritchett EL, Page RL, Carlson M, Undesser K, Fava G; Rythmol Atrial
Fibrillation Trial (RAFT) Investigators. Efficacy and safety of sustained-release
propafenone (propafenone SR) for patients with atrial fibrillation. Am J Cardiol
2003;92:941946.
923. Hohnloser SH, Crijns HJ, van Eickels M, Gaudin C, Page RL, Torp-Pedersen C,
Connolly SJ; Athena Investigators. Effect of dronedarone on cardiovascular
events in atrial fibrillation. N Engl J Med 2009;360:668678.
924. Le Heuzey JY, De Ferrari GM, Radzik D, Santini M, Zhu J, Davy JM. A short-
term, randomized, double-blind, parallel-group study to evaluate the efficacy
and safety of dronedarone versus amiodarone in patients with persistent
atrial fibrillation: the DIONYSOS study. J Cardiovasc Electrophysiol
2010;21:597605.
925. Singh BN, Connolly SJ, Crijns HJ, Roy D, Kowey PR, Capucci A, Radzik D, Aliot
EM, Hohnloser SH, for the EURIDIS and ADONIS Investigators. Dronedarone
for maintenance of sinus rhythm in atrial fibrillation or flutter. N Engl J Med
2007;357:987999.
926. Touboul P, Brugada J, Capucci A, Crijns HJ, Edvardsson N, Hohnloser SH.
Dronedarone for prevention of atrial fibrillation: a dose-ranging study. Eur
Heart J 2003;24:14811487.
927. Kober L, Torp-Pedersen C, McMurray JJ, Gotzsche O, Levy S, Crijns H, Amlie J,
Carlsen J, Dronedarone Study G. Increased mortality after dronedarone ther-
apy for severe heart failure. N Engl J Med 2008;358:26782687.
928. Wu C, Tcherny-Lessenot S, Dai W, Wang Y, Kechemir H, Gandhi S, Lin S,
Juhaeri J. Assessing the risk for peripheral neuropathy in patients treated with
dronedarone compared with that in other antiarrhythmics. Clin Ther
2018;
40:450455.e1.
929. Piccini JP, Hasselblad V, Peterson ED, Washam JB, Califf RM, Kong DF.
Comparative efficacy of dronedarone and amiodarone for the maintenance of
sinus rhythm in patients with atrial fibrillation. J Am Coll Cardiol
2009;54:10891095.
930. Gao S, Dai W, Zhang L, Juhaeri J, Wang Y, Caubel P. Risk of cardiovascular
events, stroke, congestive heart failure, interstitial lung disease, and acute liver
injury: dronedarone versus amiodarone and other antiarrhythmics. J Atr
Fibrillation 2013;6:890.
931. Pisters R, Hohnloser SH, Connolly SJ, Torp-Pedersen C, Naditch-Brule L, Page
RL, Crijns HJ; ATHENA Investigators. Effect of dronedarone on clinical end
points in patients with atrial fibrillation and coronary heart disease: insights
from the ATHENA trial. Europace 2014;16:174181.
932. Connolly SJ, Camm AJ, Halperin JL, Joyner C, Alings M, Amerena J, Atar D,
Avezum A, Blomstrom P, Borggrefe M, Budaj A, Chen SA, Ching CK,
Commerford P, Dans A, Davy JM, Delacretaz E, Di Pasquale G, Diaz R, Dorian
P, Flaker G, Golitsyn S, Gonzalez-Hermosillo A, Granger CB, Heidbuchel H,
Kautzner J, Kim JS, Lanas F, Lewis BS, Merino JL, Morillo C, Murin J, Narasimhan
C, Paolasso E, Parkhomenko A, Peters NS, Sim KH, Stiles MK, Tanomsup S,
Toivonen L, Tomcsanyi J, Torp-Pedersen C, Tse HF, Vardas P, Vinereanu D,
Xavier D, Zhu J, Zhu JR, Baret-Cormel L, Weinling E, Staiger C, Yusuf S,
Chrolavicius S, Afzal R, Hohnloser SH;PALLAS Investigators. Dronedarone in
high-risk permanent atrial fibrillation. N Engl J Med 2011;365:22682276.
933. Friberg L. Safety of dronedarone in routine clinical care. J Am Coll Cardiol
2014;63:23762384.
934. Friberg L. Ventricular arrhythmia and death among atrial fibrillation patients
using anti-arrhythmic drugs. Am Heart J 2018;205:118127.
935. Khan MH, Rochlani Y, Aronow WS. Efficacy and safety of dronedarone in the
treatment of patients with atrial fibrillation. Expert Opin Drug Saf
2017;16:14071412.
936. Vamos M, Hohnloser SH. Amiodarone and dronedarone: an update. Trends
Cardiovasc Med 2016;26:597602.
937. Tschuppert Y, Buclin T, Rothuizen LE, Decosterd LA, Galleyrand J, Gaud C,
Biollaz J. Effect of dronedarone on renal function in healthy subjects. Br J Clin
Pharmacol 2007;64:785791.
938. Vijayalakshmi K, Whittaker VJ, Sutton A, Campbell P, Wright RA, Hall JA,
Harcombe AA, Linker NJ, Stewart MJ, Davies A, de Belder MA. A randomized
trial of prophylactic antiarrhythmic agents (amiodarone and sotalol) in patients
with atrial fibrillation for whom direct current cardioversion is planned. Am
Heart J 2006;151:863.e1-6.
939. Capucci A, Botto G, Molon G, Spampinato A, Favale S, Proclemer A, Porfilio A,
Marotta T, Vimercati M, Boriani G; DAPHNE Study Investigators. The Drug
And Pace Health cliNical Evaluation (DAPHNE) study: a randomized trial com-
paring sotalol versus beta-blockers to treat symptomatic atrial fibrillation in
patients with brady-tachycardia syndrome implanted with an antitachycardia
pacemaker. Am Heart J 2008;156:373.e1-8.
940. Juul-Moller S, Edvardsson N, Rehnqvist-Ahlberg N. Sotalol versus quinidine for
the maintenance of sinus rhythm after direct current conversion of atrial fibrilla-
tion. Circulation 1990;82:1932
199.
941. MacNeil DJ, Davies RO, Deitchman D. Clinical safety profile of sotalol in the
treatment of arrhythmias. Am J Cardiol 1993;72:44A50A.
942. Roy D, Talajic M, Dorian P, Connolly S, Eisenberg MJ, Green M, Kus T, Lambert
J, Dubuc M, Gagne P, Nattel S, Thibault B. Amiodarone to prevent recurrence
of atrial fibrillation. Canadian Trial of Atrial Fibrillation Investigators. N Engl J
Med 2000;342:913920.
943. Andersen SS, Hansen ML, Gislason GH, Schramm TK, Folke F, Fosbol E,
Abildstrom SZ, Madsen M, Kober L, Torp-Pedersen C. Antiarrhythmic therapy
and risk of death in patients with atrial fibrillation: a nationwide study. Europace
2009;11:886891.
944. Crijns HJ, Gosselink AT, Lie KI. Propafenone versus disopyramide for mainte-
nance of sinus rhythm after electrical cardioversion of chronic atrial fibrillation:
a randomized, double-blind study. PRODIS Study Group. Cardiovasc Drugs Ther
1996;10:145152.
110 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
945. Lloyd EA, Gersh BJ, Forman R. The efficacy of quinidine and disopyramide in
the maintenance of sinus rhythm after electroconversion from atrial fibrillation.
A double-blind study comparing quinidine, disopyramide and placebo. S Afr Med
J 1984;65:367369.
946. Karlson BW, Torstensson I, Abjorn C, Jansson SO, Peterson LE. Disopyramide
in the maintenance of sinus rhythm after electroconversion of atrial fibrillation.
A placebo-controlled one-year follow-up study. Eur Heart J 1988;9:284290.
947. Coplen SE, Antman EM, Berlin JA, Hewitt P, Chalmers TC. Efficacy and safety
of quinidine therapy for maintenance of sinus rhythm after cardioversion. A
meta-analysis of randomized control trials. Circulation 1990;82:11061116.
948. Lip GY, Laroche C, Dan GA, Santini M, Kalarus Z, Rasmussen LH, Oliveira MM,
Mairesse G, Crijns HJ, Simantirakis E, Atar D, Kirchhof P, Vardas P, Tavazzi L,
Maggioni AP. A prospective survey in European Society of Cardiology member
countries of atrial fibrillation management: baseline results of
EURObservational Research Programme Atrial Fibrillation (EORP-AF) pilot
general registry. Europace 2014;16:308319.
949. Dagres N, Lewalter T, Lip GY, Pison L, Proclemer A, Blomstrom-Lundqvist C,
Scientific Initiatives Committee EHRA. Current practice of antiarrhythmic drug
therapy for prevention of atrial fibrillation in Europe: the European Heart
Rhythm Association survey. Europace 2013;15:478481.
950. Sherrid MV, Barac I, McKenna WJ, Elliott PM, Dickie S, Chojnowska L, Casey S,
Maron BJ. Multicenter study of the efficacy and safety of disopyramide in
obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol
2005;45:12511258.
951. Goette A, Staack T, Rocken C, Arndt M, Geller JC, Huth C, Ansorge S, Klein
HU, Lendeckel U. Increased expression of extracellular signal-regulated kinase
and angiotensin-converting enzyme in human atria during atrial fibrillation. JAm
Coll Cardiol 2000;35:16691677.
952. Thanigaimani S, Lau DH, Agbaedeng T, Elliott AD, Mahajan R, Sanders P.
Molecular mechanisms of atrial fibrosis: implications for the clinic. Expert Rev
Cardiovasc Ther 2017;15:247256.
953. Kumagai K, Nakashima H, Urata H, Gondo N, Arakawa K, Saku K. Effects of
angiotensin II type 1 receptor antagonist on electrical and structural remodeling
in atrial fibrillation. J Am Coll Cardiol 2003;41:21972204.
954. Schneider MP, Hua TA, Bohm M, Wachtell K, Kjeldsen SE, Schmieder RE.
Prevention of atrial fibrillation by renin-angiotensin system inhibition a meta-
analysis. J Am Coll Cardiol 2010;55:22992307.
955. Healey JS, Baranchuk A, Crystal E, Morillo CA, Garfinkle M, Yusuf S, Connolly
SJ. Prevention of atrial fibrillation with angiotensin-converting enzyme inhibitors
and angiotensin receptor blockers: a meta-analysis. J Am Coll Cardiol
2005;45:18321839.
956. Ducharme A, Swedberg K, Pfeffer MA, Cohen-Solal A, Granger CB, Maggioni
AP, Michelson EL, McMurray JJ, Olsson L, Rouleau JL, Young JB, Yusuf S.
Prevention of atrial fibrillation in patients with symptomatic chronic heart fail-
ure by candesartan in the Candesartan in Heart failure: Assessment of
Reduction in Mortality and morbidity (CHARM) program. Am Heart J
2006;152:8692.
957. McMurray JJ, Young JB, Dunlap ME, Granger CB, Hainer J, Michelson EL, Earle
S, Olofsson B, Ostergren J, Yusuf S, Swedberg K, Pfeffer MA, CHARM
Investigators. Relationship of dose of background angiotensin-converting
enzyme inhibitor to the benefits of candesartan in the Candesartan in Heart fail-
ure: Assessment of Reduction in Mortality and morbidity (CHARM)-Added
trial. Am Heart J 2006;151:985991.
958. Wachtell K, Lehto M, Gerdts E, Olsen MH, Hornestam B, Dahlof B, Ibsen H,
Julius S, Kjeldsen SE, Lindholm LH, Nieminen MS, Devereux RB. Angiotensin II
receptor blockade reduces new-onset atrial fibrillation and subsequent stroke
compared to atenolol: the Losartan Intervention For End Point Reduction in
Hypertension (LIFE) study. J Am Coll Cardiol 2005;45:712719.
959. Anand K, Mooss AN, Hee TT, Mohiuddin SM. Meta-analysis: inhibition of renin-
angiotensin system prevents new-onset atrial fibrillation. Am Heart J
2006;152:217222.
960. Okin PM, Wachtell K, Devereux RB, Harris KE, Jern S, Kjeldsen SE, Julius S,
Lindholm LH, Nieminen MS, Edelman JM, Hille DA, Dahlof B. Regression of
electrocardiographic left ventricular hypertrophy and decreased incidence of
new-onset atrial fibrillation in patients with hypertension. JAMA
2006;296:12421248.
961. Olsson LG, Swedberg K, Ducharme A, Granger CB, Michelson EL, McMurray JJ,
Puu M, Yusuf S, Pfeffer MA; CHARM Investigators. Atrial fibrillation and risk of
clinical events in chronic heart failure with and without left ventricular systolic
dysfunction: results from the Candesartan in Heart failure: Assessment of
Reduction in Mortality and morbidity (CHARM) program. J Am Coll Cardiol
2006;47:19972004.
962. Marott SC, Nielsen SF, Benn M, Nordestgaard BG. Antihypertensive treatment
and risk of atrial fibrillation: a nationwide study. Eur Heart J
2014;35:12051214.
963. Goette A, Schon N, Kirchhof P, Breithardt G, Fetsch T, Hausler KG, Klein HU,
Steinbeck G, Wegscheider K, Meinertz T. Angiotensin II-antagonist in paroxys-
mal atrial fibrillation (ANTIPAF) trial. Circ Arrhythm Electrophysiol 2012;5:4351.
964. Savelieva I, Kakouros N, Kourliouros A, Camm AJ. Upstream therapies for man-
agement of atrial fibrillation: review of clinical evidence and implications for
European Society of Cardiology guidelines. Part II: secondary prevention.
Europace 2011;13:610625.
965. Reil JC, Hohl M, Selejan S, Lipp P, Drautz F, Kazakow A, Munz BM, Muller P,
Steendijk P, Reil GH, Allessie MA, Bohm M, Neuberger HR. Aldosterone pro-
motes atrial fibrillation. Eur Heart J 2012;33:20982108.
966. Reil JC, Tauchnitz M, Tian Q, Hohl M, Linz D, Oberhofer M, Kaestner L, Reil
GH, Thiele H, Steendijk P, Bohm M, Neuberger HR, Lipp P.
Hyperaldosteronism induces left atrial systolic and diastolic dysfunction. Am J
Physiol Heart Circ Physiol 2016;311:H1014H1023.
967. Tsai CT, Chiang FT, Tseng CD, Hwang JJ, Kuo KT, Wu CK, Yu CC, Wang YC,
Lai LP, Lin JL. Increased expression of mineralocorticoid receptor in human
atrial fibrillation and a cellular model of atrial fibrillation. J Am Coll Cardiol
2010;
55:758770.
968. Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, Bittman R,
Hurley S, Kleiman J, Gatlin M; Eplerenone Post-Acute Myocardial Infarction
Heart Failure Efficacy Survival Study Investigators. Eplerenone, a selective aldos-
terone blocker, in patients with left ventricular dysfunction after myocardial
infarction. N Engl J Med 2003;348:13091321.
969. Swedberg K, Zannad F, McMurray JJ, Krum H, van Veldhuisen DJ, Shi H, Vincent
J, Pitt B; EMPHASIS-HF Study Investigators. Eplerenone and atrial fibrillation in
mild systolic heart failure: results from the EMPHASIS-HF (Eplerenone in Mild
Patients Hospitalization And SurvIval Study in Heart Failure) study. J Am Coll
Cardiol 2012;59:15981603.
970. Cikes M, Claggett B, Shah AM, Desai AS, Lewis EF, Shah SJ, Anand IS, O’Meara
E, Rouleau JL, Sweitzer NK, Fang JC, Saksena S, Pitt B, Pfeffer MA, Solomon SD.
Atrial fibrillation in heart failure with preserved ejection fraction: the TOPCAT
trial. JACC Heart Fail 2018;6:689697.
971. Neefs J, van den Berg NW, Limpens J, Berger WR, Boekholdt SM, Sanders P, de
Groot JR. Aldosterone pathway blockade to prevent atrial fibrillation: a system-
atic review and meta-analysis. Int J Cardiol 2017;231:155161.
972. Kuhlkamp V, Schirdewan A, Stangl K, Homberg M, Ploch M, Beck OA. Use of
metoprolol CR/XL to maintain sinus rhythm after conversion from persistent
atrial fibrillation: a randomized, double-blind, placebo-controlled study. JAm
Coll Cardiol 2000;36:139146.
973. Nergardh AK, Rosenqvist M, Nordlander R, Frick M. Maintenance of sinus
rhythm with metoprolol CR initiated before cardioversion and repeated cardio-
version of atrial fibrillation: a randomized double-blind placebo-controlled
study. Eur Heart J 2007;28:13511357.
974. Zheng Z, Jayaram R, Jiang L, Emberson J, Zhao Y, Li Q, Du J, Guarguagli S, Hill
M, Chen Z, Collins R, Casadei B. Perioperative rosuvastatin in cardiac surgery.
N Engl J Med 2016;374:17441753.
975. Rahimi K, Emberson J, McGale P, Majoni W, Merhi A, Asselbergs FW, Krane V,
Macfarlane PW, PROSPER Executive. Effect of statins on atrial fibrillation: col-
laborative meta-analysis of published and unpublished evidence from rando-
mised controlled trials. BMJ 2011;342:d1250.
976. Pinho-Gomes AC, Reilly S, Brandes RP, Casadei B. Targeting inflammation and
oxidative stress in atrial fibrillation: role of 3-hydroxy-3-methylglutaryl-coenzyme
a reductase inhibition with statins. Antioxid Redox Signal 2014;20:12681285.
977. Humphries KH, Lee M, Sheldon R, Ramanathan K, Dorian P, Green M, Kerr CR;
CARAF Investigators. Statin use and recurrence of atrial fibrillation after suc-
cessful cardioversion. Am Heart J 2007;154:908913.
978. Bianconi L, Calo L, Mennuni M, Santini L, Morosetti P, Azzolini P, Barbato G,
Biscione F, Romano P, Santini M. n-3 polyunsaturated fatty acids for the preven-
tion of arrhythmia recurrence after electrical cardioversion of chronic persis-
tent atrial fibrillation: a randomized, double-blind, multicentre study. Europace
2011;13:174181.
979. Mozaffarian D, Marchioli R, Macchia A, Silletta MG, Ferrazzi P, Gardner TJ,
Latini R, Libby P, Lombardi F, O’Gara PT, Page RL, Tavazzi L, Tognoni G;
OPERA Investigators. Fish oil and postoperative atrial fibrillation: the Omega-3
Fatty Acids for Prevention of Post-operative Atrial Fibrillation (OPERA)
randomized trial. JAMA 2012;308:20012011.
980. Yamashita T, Inoue H, Okumura K, Kodama I, Aizawa Y, Atarashi H, Ohe T,
Ohtsu H, Kato T, Kamakura S, Kumagai K, Kurachi Y, Koretsune Y, Saikawa T,
Sakurai M, Sato T, Sugi K, Nakaya H, Hirai M, Hirayama A, Fukatani M,
Mitamura H, Yamazaki T, Watanabe E, Ogawa S; J-RHYTHM II Investigators.
Randomized trial of angiotensin II-receptor blocker vs. dihydropiridine calcium
channel blocker in the treatment of paroxysmal atrial fibrillation with hyperten-
sion (J-RHYTHM II study). Europace 2011;13:473479.
981. Macchia A, Grancelli H, Varini S, Nul D, Laffaye N, Mariani J, Ferrante D, Badra
R, Figal J, Ramos S, Tognoni G, Doval HC; GESICA Investigators. Omega-3 fatty
ESC Guidelines 111

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
acids for the prevention of recurrent symptomatic atrial fibrillation: results of
the FORWARD (Randomized Trial to Assess Efficacy of PUFA for the
Maintenance of Sinus Rhythm in Persistent Atrial Fibrillation) trial. J Am Coll
Cardiol 2013;61:463468.
982. Kowey PR, Reiffel JA, Ellenbogen KA, Naccarelli GV, Pratt CM. Efficacy and
safety of prescription omega-3 fatty acids for the prevention of recurrent symp-
tomatic atrial fibrillation: a randomized controlled trial. JAMA
2010;304:23632372.
983. Kochiadakis GE, Marketou ME, Igoumenidis NE, Chrysostomakis SI, Mavrakis
HE, Kaleboubas MD, Vardas PE. Amiodarone, sotalol, or propafenone in atrial
fibrillation: which is preferred to maintain normal sinus rhythm?Pacing Clin
Electrophysiol 2000;23:18831887.
984. Boriani G, Biffi M, Capucci A, Botto GL, Broffoni T, Rubino I, Della Casa S,
Sanguinetti M, Magnani B. Oral propafenone to convert recent-onset atrial
fibrillation in patients with and without underlying heart disease. A randomized,
controlled trial. Ann Intern Med 1997;126:621625.
985. Ehrlich JR, Look C, Kostev K, Israel CW, Goette A. Impact of dronedarone on
the risk of myocardial infarction and stroke in atrial fibrillation patients followed
in general practices in Germany. Int J Cardiol 2019;278:126132.
986. Camm AJ. Hopes and disappointments with antiarrhythmic drugs. Int J Cardiol
2017;237:7174.
987. De Vecchis R. Long-term antiarrhythmic drug treatment after atrial fibrillation
ablation: does a too obstinate rhythm control strategy bring serious risk of
proarrhythmia to ablated patients?Eur Heart J Cardiovasc Pharmacother
2019;5:117118.
988. Fabritz L, Kirchhof P. Predictable and less predictable unwanted cardiac drugs
effects: individual pre-disposition and transient precipitating factors. Basic Clin
Pharmacol Toxicol 2010;106:263268.
989. Reimold FR, Reynolds MR. Proarrhythmia and death with antiarrhythmic drugs
for atrial fibrillation, and the unfulfilled promise of comparative effectiveness
research. Am Heart J 2018;205:128130.
990. Coughtrie AL, Behr ER, Layton D, Marshall V, Camm AJ, Shakir SAW. Drugs
and life-threatening ventricular arrhythmia risk: results from the DARE study
cohort. BMJ Open 2017;7:e016627.
991. Haverkamp W, Breithardt G, Camm AJ, Janse MJ, Rosen MR, Antzelevitch C,
Escande D, Franz M, Malik M, Moss A, Shah R. The potential for QT prolonga-
tion and proarrhythmia by non-antiarrhythmic drugs: clinical and regulatory
implications. Report on a policy conference of the European Society of
Cardiology. Eur Heart J 2000;21:12161231.
992. Milan DJ, Saul JP, Somberg JC, Molnar J. Efficacy of intravenous and oral sotalol
in pharmacologic conversion of atrial fibrillation: a systematic review and meta-
analysis. Cardiology 2017;136
:5260.
993. Agusala K, Oesterle A, Kulkarni C, Caprio T, Subacius H, Passman R. Risk
prediction for adverse events during initiation of sotalol and dofetilide
for the treatment of atrial fibrillation. Pacing Clin Electrophy siol
2015;38:490498.
994. Lin CY, Lin YJ, Lo LW, Chen YY, Chong E, Chang SL, Chung FP, Chao TF, Hu
YF, Tuan TC, Liao JN, Chang Y, Chien KL, Chiou CW, Chen SA. Factors predis-
posing to ventricular proarrhythmia during antiarrhythmic drug therapy for
atrial fibrillation in patients with structurally normal heart. Heart Rhythm
2015;12:14901500.
995. Kaab S, Hinterseer M, Nabauer M, Steinbeck G. Sotalol testing unmasks altered
repolarization in patients with suspected acquired long-QT-syndrome a
case-control pilot study using i.v. sotalol. Eur Heart J 2003;24:649657.
996. Lehtonen A, Fodstad H, Laitinen-Forsblom P, Toivonen L, Kontula K, Swan H.
Further evidence of inherited long QT syndrome gene mutations in antiarrhyth-
mic drug-associated torsades de pointes. Heart Rhythm 2007;4:603607.
997. Patten M, Maas R, Bauer P, Luderitz B, Sonntag F, Dluzniewski M, Hatala R,
Opolski G, Muller HW, Meinertz T; SOPAT Investigators. Suppression of par-
oxysmal atrial tachyarrhythmias results of the SOPAT trial. Eur Heart J
2004;25:13951404.
998. Fetsch T, Bauer P, Engberding R, Koch HP, Lukl J, Meinertz T, Oeff M, Seipel L,
Trappe HJ, Treese N, Breithardt G; Prevention of Atrial Fibrillation after
Cardioversion Investigators. Prevention of atrial fibrillation after cardioversion:
results of the PAFAC trial. Eur Heart J 2004;25:13851394.
999. Vallurupalli S, Pothineni NV, Deshmukh A, Paydak H. Utility of routine exercise
testing to detect rate-related QRS widening in patients without structural heart
disease on class Ic antiarrhythmic agents (flecainide and propafenone). Am J
Cardiol 2015;116:730732.
1000. Parkash R, Wells GA, Sapp JL, Healey JS, Tardif J-C, Greiss I, Rivard L, Roux J-
F, Gula L, Nault I. Effect of aggressive blood pressure control on the recur-
rence of atrial fibrillation after catheter ablation: a randomized, open-label clin-
ical trial (SMAC-AF [Substrate Modification With Aggressive Blood Pressure
Control]). Circulation 2017;135:17881798.
1001. Huxley RR, Misialek JR, Agarwal SK, Loehr LR, Soliman EZ, Chen LY, Alonso
A. Physical activity, obesity, weight change, and risk of atrial fibrillation: the
Atherosclerosis Risk in Communities study. Circ Arrhythm Electrophysiol
2014;7:620625.
1002. Murphy NF, MacIntyre K, Stewart S, Hart CL, Hole D, McMurray JJ. Long-
term cardiovascular consequences of obesity: 20-year follow-up of more than
15 000 middle-aged men and women (the Renfrew-Paisley study). Eur Heart J
2006;27:96106.
1003. Wanahita N, Messerli FH, Bangalore S, Gami AS, Somers VK, Steinberg JS.
Atrial fibrillation and obesity results of a meta-analysis. Am Heart J
2008;155:310315.
1004. Wang TJ, Parise H, Levy D, D’Agostino RB Sr, Wolf PA, Vasan RS, Benjamin EJ.
Obesity and the risk of new-onset atrial fibrillation. JAMA 2004;292:24712477.
1005. Baek YS, Yang PS, Kim TH, Uhm JS, Park J, Pak HN, Lee MH, Joung B.
Associations of abdominal obesity and new-onset atrial fibrillation in the gen-
eral population. J Am Heart Assoc 2017;6.
1006. Proietti M, Guiducci E, Cheli P, Lip GY. Is there an obesity paradox for out-
comes in atrial fibrillation? A systematic review and meta-analysis of non-
vitamin K antagonist oral anticoagulant trials. Stroke 2017;48:857 866.
1007. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney
MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Lochen
ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar
N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM,
Binno S, ESC Scientific Document Group. 2016 European Guidelines on cardi-
ovascular disease prevention in clinical practice: the Sixth Joint Task Force of
the European Society of Cardiology and other societies on cardiovascular dis-
ease prevention in clinical practice (constituted by representatives of 10 soci-
eties and by invited experts). Developed with the special contribution of the
European Association for Cardiovascular Prevention & Rehabilitation
(EACPR). Eur Heart J 2016;37:23152381.
1008. Cha YM, Friedman PA, Asirvatham SJ, Shen WK, Munger TM, Rea RF, Brady
PA, Jahangir A, Monahan KH, Hodge DO, Meverden RA, Gersh BJ, Hammill
SC, Packer DL. Catheter ablation for atrial fibrillation in patients with obesity.
Circulation 2008;117:25832590.
1009. Ector J, Dragusin O, Adriaenssens B, Huybrechts W, Willems R, Ector H,
Heidbuchel H. Obesity is a major determinant of radiation dose in patients
undergoing pulmonary vein isolation for atrial fibrillation. J Am Coll Cardiol
2007;50:234242.
1010. Shoemaker MB, Muhammad R, Farrell M, Parvez B, White BW, Streur M,
Stubblefield T, Rytlewski J, Parvathaneni S, Nagarakanti R, Roden DM,
Saavedra P, Ellis C, Whalen SP, Darbar D. Relation of morbid obesity and
female gender to risk of procedural complications in patients undergoing atrial
fibrillation ablation. Am J Cardiol 2013;111:368373.
1011. Ettinger PO, Wu CF, De La Cruz C Jr, Weisse AB, Ahmed SS, Regan TJ.
Arrhythmias and the ‘holiday heart’: alcohol-associated cardiac rhythm disor-
ders. Am Heart J 1978;95:555562.
1012. Conen D, Albert CM. Alcohol consumption and risk of atrial fibrillation: how
much is too much?J Am Coll Cardiol 2014;64:290292.
1013. Liang Y, Mente A, Yusuf S, Gao P, Sleight P, Zhu J, Fagard R, Lonn E, Teo KK;
ONTARGET and TRANSCEND Investigators. Alcohol consumption and the
risk of incident atrial fibrillation among people with cardiovascular disease.
CMAJ 2012;184:E857866.
1014. Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrilla-
tion: a prospective study and dose-response meta-analysis. J Am Coll Cardiol
2014;64:281289.
1015. Overvad TF, Rasmussen LH, Skjoth F, Overvad K, Albertsen IE, Lane DA, Lip
GY, Larsen TB. Alcohol intake and prognosis of atrial fibrillation. Heart
2013;99:1093
1099.
1016. Voskoboinik A, Kalman JM, De Silva A, Nicholls T, Costello B, Nanayakkara S,
Prabhu S, Stub D, Azzopardi S, Vizi D, Wong G, Nalliah C, Sugumar H, Wong
M, Kotschet E, Kaye D, Taylor AJ, Kistler PM. Alcohol abstinence in drinkers
with atrial fibrillation. N Engl J Med 2020;382:2028.
1017. Lavie CJ, Thomas RJ, Squires RW, Allison TG, Milani RV. Exercise training and
cardiac rehabilitation in primary and secondary prevention of coronary heart
disease. Mayo Clin Proc 2009;84:373383.
1018. Mont L. Arrhythmias and sport practice. Heart 2010;96:398405.
1019. Menezes AR, Lavie CJ, De Schutter A, Milani RV, O’Keefe J, DiNicolantonio JJ,
Morin DP, Abi-Samra FM. Lifestyle modification in the prevention and treat-
ment of atrial fibrillation. Prog Cardiovasc Dis 2015;58:117125.
1020. Karjalainen J, Kujala UM, Kaprio J, Sarna S, Viitasalo M. Lone atrial fibrillation in vigo-
rously exercising middle aged men: case-control study. BMJ 1998;316:17841785.
1021. Baldesberger S, Bauersfeld U, Candinas R, Seifert B, Zuber M, Ritter M, Jenni
R, Oechslin E, Luthi P, Scharf C, Marti B, Attenhofer Jost CH. Sinus node dis-
ease and arrhythmias in the long-term follow-up of former professional
cyclists. Eur Heart J 2008;29:7178.
1022. Molina L, Mont L, Marrugat J, Berruezo A, Brugada J, Bruguera J, Rebato C,
Elosua R. Long-term endurance sport practice increases the incidence of lone
atrial fibrillation in men: a follow-up study. Europace 2008;10:618623.
112 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1023. Nielsen JR, Wachtell K, Abdulla J. The relationship between physical activity
and risk of atrial fibrillation a systematic review and meta-analysis. J Atr
Fibrillation 2013;5:789.
1024. Risom SS, Zwisler AD, Johansen PP, Sibilitz KL, Lindschou J, Gluud C, Taylor
RS, Svendsen JH, Berg SK. Exercise-based cardiac rehabilitation for adults with
atrial fibrillation. Cochrane Database Syst Rev 2017;2:CD011197.
1025. Dzeshka MS, Shantsila A, Shantsila E, Lip GYH. Atrial fibrillation and hyperten-
sion. Hypertension 2017;70:854861.
1026. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M,
Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F,
Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S,
Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E,
Tsioufis C, Aboyans V, Desormais I, ESC Scientific Document Group. 2018
ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J
2018;39:30213104.
1027. Kim TH, Yang PS, Yu HT, Jang E, Shin H, Kim HY, Uhm JS, Kim JY, Sung JH,
Pak HN, Lee MH, Joung B, Lip GYH. Effect of hypertension duration and
blood pressure level on ischaemic stroke risk in atrial fibrillation: nationwide
data covering the entire Korean population. Eur Heart J 2019;40:809819.
1028. Lip GY, Frison L, Grind M. Effect of hypertension on anticoagulated patients
with atrial fibrillation. Eur Heart J 2007;28:752759.
1029. Steinberg JS, Shabanov V, Ponomarev D, Losik D, Ivanickiy E, Kropotkin E,
Polyakov K, Ptaszynski P, Keweloh B, Yao CJ, Pokushalov EA, Romanov AB.
Effect of renal denervation and catheter ablation vs catheter ablation alone on
atrial fibrillation recurrence among patients with paroxysmal atrial fibrillation
and hypertension: the ERADICATE-AF randomized clinical trial. JAMA
2020;323:248255.
1030. Du X, Ninomiya T, de Galan B, Abadir E, Chalmers J, Pillai A, Woodward M,
Cooper M, Harrap S, Hamet P, Poulter N, Lip GY, Patel A, Group AC. Risks
of cardiovascular events and effects of routine blood pressure lowering among
patients with type 2 diabetes and atrial fibrillation: results of the ADVANCE
study. Eur Heart J 2009;30:11281135.
1031. Pallisgaard JL, Schjerning AM, Lindhardt TB, Procida K, Hansen ML, Torp-
Pedersen C, Gislason GH. Risk of atrial fibrillation in diabetes mellitus: a
nationwide cohort study. Eur J Prev Cardiol 2016;23:621627.
1032. Rizzo MR, Sasso FC, Marfella R, Siniscalchi M, Paolisso P, Carbonara O,
Capoluongo MC, Lascar N, Pace C, Sardu C, Passavanti B, Barbieri M, Mauro
C, Paolisso G. Autonomic dysfunction is associated with brief episodes of
atrial fibrillation in type 2 diabetes. J Diabetes Complications 2015;29:8892.
1033. Movahed MR, Hashemzadeh M, Jamal MM. Diabetes mellitus is a strong, inde-
pendent risk for atrial fibrillation and flutter in addition to other cardiovascular
disease. Int J Cardiol 2005;105:315318.
1034. Lee SR, Choi EK, Rhee TM, Lee HJ, Lim WH, Kang SH, Han KD, Cha MJ, Cho
Y, Oh IY, Oh S. Evaluation of the association between diabetic retinopathy
and the incidence of atrial fibrillation: a nationwide population-based study. Int
J Cardiol 2016;223:953
957.
1035. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de
Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela
BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB,
McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K,
Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ,
Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh
RW, Turner MB, American Heart Association Statistics Committee and
Stroke Statistics Subcommittee. Heart disease and stroke statistics 2015
update: a report from the American Heart Association. Circulation
2015;131:e29322.
1036. Fatemi O, Yuriditsky E, Tsioufis C, Tsachris D, Morgan T, Basile J, Bigger T,
Cushman W, Goff D, Soliman EZ, Thomas A, Papademetriou V. Impact of
intensive glycemic control on the incidence of atrial fibrillation and associated
cardiovascular outcomes in patients with type 2 diabetes mellitus (from the
Action to Control Cardiovascular Risk in Diabetes study). Am J Cardiol
2014;114:12171222.
1037. Chang SH, Wu LS, Chiou MJ, Liu JR, Yu KH, Kuo CF, Wen MS, Chen WJ, Yeh
YH, See LC. Association of metformin with lower atrial fibrillation risk among
patients with type 2 diabetes mellitus: a population-based dynamic cohort and
in vitro studies. Cardiovasc Diabetol 2014;13:123.
1038. Zhang Z, Zhang X, Korantzopoulos P, Letsas KP, Tse G, Gong M, Meng L, Li
G, Liu T. Thiazolidinedione use and atrial fibrillation in diabetic patients: a
meta-analysis. BMC Cardiovasc Disord 2017;17:96.
1039. Bell DSH, Goncalves E. Atrial fibrillation and type 2 diabetes: prevalence, etiol-
ogy, pathophysiology and effect of anti-diabetic therapies. Diabetes Obes Metab
2019;21:210217.
1040. Patti G, Di Gioia G, Cavallari I, Nenna A. Safety and efficacy of nonvitamin K
antagonist oral anticoagulants versus warfarin in diabetic patients with atrial
fibrillation: a study-level meta-analysis of phase III randomized trials. Diabetes
Metab Res Rev 2017;33.
1041. Hylek EM, Held C, Alexander JH, Lopes RD, De Caterina R, Wojdyla DM,
Huber K, Jansky P, Steg PG, Hanna M, Thomas L, Wallentin L, Granger CB.
Major bleeding in patients with atrial fibrillation receiving apixaban or warfarin:
the ARISTOTLE trial (Apixaban for Reduction in Stroke and Other
Thromboembolic Events in Atrial Fibrillation): predictors, characteristics, and
clinical outcomes. J Am Coll Cardiol 2014;63:21412147.
1042. Donnellan E, Aagaard P, Kanj M, Jaber W, Elshazly M, Hoosien M, Baranowski
B, Hussein A, Saliba W, Wazni O. Association between pre-ablation glycemic
control and outcomes among patients with diabetes undergoing atrial fibrilla-
tion ablation. JACC Clin Electrophysiol 2019;5:897903.
1043. Linz D, Baumert M, Catcheside P, Floras J, Sanders P, Levy P, Cowie MR,
Doug McEvoy R. Assessment and interpretation of sleep disordered breathing
severity in cardiology: clinical implications and perspectives. Int J Cardiol
2018;271:281288.
1044. Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE, Malouf JF,
Ammash NM, Friedman PA, Somers VK. Association of atrial fibrillation and
obstructive sleep apnea. Circulation 2004;110:364367.
1045. Goudis CA, Ketikoglou DG. Obstructive sleep and atrial fibrillation: pathophy-
siological mechanisms and therapeutic implications. Int J Cardiol
2017;230:293300.
1046. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, Ramar K,
Rogers R, Schwab RJ, Weaver EM, Weinstein MD, Adult Obstructive Sleep
Apnea Task Force of the American Academy of Sleep Medicine. Clinical guide-
line for the evaluation, management and long-term care of obstructive sleep
apnea in adults. J Clin Sleep Med 2009;5:263276.
1047. Linz D, McEvoy RD, Cowie MR, Somers VK, Nattel S, Levy P, Kalman JM, Sanders
P. Associations of obstructive sleep apnea with atrial fibrillation and continuous
positive airway pressure treatment: a review. JAMA Cardiol 2018;3:532540.
1048. Fein AS, Shvilkin A, Shah D, Haffajee CI, Das S, Kumar K, Kramer DB,
Zimetbaum PJ, Buxton AE, Josephson ME, Anter E. Treatment of obstructive
sleep apnea reduces the risk of atrial fibrillation recurrence after catheter abla-
tion. J Am Coll Cardiol 2013;62:300305.
1049. Neilan TG, Farhad H, Dodson JA, Shah RV, Abbasi SA, Bakker JP, Michaud GF,
van der Geest R, Blankstein R, Steigner M, John RM, Jerosch-Herold M,
Malhotra A, Kwong RY. Effect of sleep apnea and continuous positive airway
pressure on cardiac structure and recurrence of atrial fibrillation. J Am Heart
Assoc 2013;2:e000421.
1050. Qureshi WT, Nasir UB, Alqalyoobi S, O’Neal WT, Mawri S, Sabbagh S,
Soliman EZ, Al-Mallah MH. Meta-analysis of continuous positive airway pres-
sure as a therapy of atrial fibrillation in obstructive sleep apnea. Am J Cardiol
2015;116:17671773.
1051. Shukla A, Aizer A, Holmes D, Fowler S, Park DS, Bernstein S, Bernstein N,
Chinitz L. Effect of obstructive sleep apnea treatment on atrial fibrillation
recurrence: a meta-analysis. JACC Clin Electrophysiol 2015;1:4151.
1052. Pathak RK, Elliott A, Middeldorp ME, Meredith M, Mehta AB, Mahajan R,
Hendriks JM, Twomey D, Kalman JM, Abhayaratna WP, Lau DH, Sanders P.
Impact of CARDIOrespiratory FITness on Arrhythmia Recurrence in Obese
Individuals With Atrial Fibrillation: the CARDIO-FIT study. J Am Coll Cardiol
2015;66:985996.
1053. Bonfanti L, Annovi A, Sanchis-Gomar F, Saccenti C, Meschi T, Ticinesi A,
Cervellin G. Effectiveness and safety of electrical cardioversion for acute-onset
atrial fibrillation in the emergency department: a real-world 10-year single cen-
ter experience. Clin Exp Emerg Med 2019;6:6469.
1054. Scheuermeyer FX, Grafstein E, Stenstrom R, Innes G, Heslop C, MacPhee J,
Pourvali R, Heilbron B, McGrath L, Christenson J. Thirty-day and 1-year out-
comes of emergency department patients with atrial fibrillation and no acute
underlying medical cause. Ann Emerg Med 2012;60:755765.e2.
1055. Boriani G, Proietti M, Laroche C, Diemberger I, Popescu MI, Riahi S, Shantsila
A, Dan GA, Tavazzi L, Maggioni AP, Lip GYH; EORP-A Pilot General Registry
Investigators. Changes to oral anticoagulant therapy and risk of death over a
3-year follow-up of a contemporary cohort of European patients with atrial
fibrillation final report of the EURObservational Research Programme on
Atrial Fibrillation (EORP-AF) pilot general registry. Int J Cardiol
2018;271:6874.
1056. Boriani G, Laroche C, Diemberger I, Fantecchi E, Popescu MI, Rasmussen LH,
Dan GA, Kalarus Z, Tavazzi L, Maggioni AP, Lip GY. ‘Real-world’ management
and outcomes of patients with paroxysmal vs. non-paroxysmal atrial fibrillation
in Europe: the EURObservational Research Programme-Atrial Fibrillation
(EORP-AF) general pilot registry. Europace 2016;18:648657.
1057. Gulizia MM, Cemin R, Colivicchi F, De Luca L, Di Lenarda A, Boriani G, Di
Pasquale G, Nardi F, Scherillo M, Lucci D, Fabbri G, Maggioni AP; BLITZ-AF
Investigators. Management of atrial fibrillation in the emergency room and in
the cardiology ward: the BLITZ AF study. Europace 2019;21:230
238.
1058. Gonzalez-Pacheco H, Marquez MF, Arias-Mendoza A, Alvarez-Sangabriel A,
Eid-Lidt G, Gonzalez-Hermosillo A, Azar-Manzur F, Altamirano-Castillo A,
Briseno-Cruz JL, Garcia-Martinez A, Mendoza-Garcia S, Martinez-Sanchez C.
ESC Guidelines 113

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Clinical features and in-hospital mortality associated with different types of
atrial fibrillation in patients with acute coronary syndrome with and without
ST elevation. J Cardiol 2015;66:148154.
1059. Krijthe BP, Leening MJ, Heeringa J, Kors JA, Hofman A, Franco OH, Witteman
JC, Stricker BH. Unrecognized myocardial infarction and risk of atrial fibrilla-
tion: the Rotterdam Study. Int J Cardiol 2013;168:14531457.
1060. Chao TF, Huang YC, Liu CJ, Chen SJ, Wang KL, Lin YJ, Chang SL, Lo LW, Hu
YF, Tuan TC, Chen TJ, Hsieh MH, Lip GY, Chen SA. Acute myocardial infarc-
tion in patients with atrial fibrillation with a CHA2DS2-VASc score of 0 or 1:
a nationwide cohort study. Heart Rhythm 2014;11:19411947.
1061. Sanclemente C, Yeste M, Suarez C, Coll R, Aguilar E, Sahuquillo JC, Lerma R,
Monreal M; FRENA Investigators. Predictors of outcome in stable outpatients
with peripheral artery disease. Intern Emerg Med 2014;9:6977.
1062. Soliman EZ, Lopez F, O’Neal WT, Chen LY, Bengtson L, Zhang ZM, Loehr L,
Cushman M, Alonso A. Atrial fibrillation and risk of ST-segment-elevation ver-
sus non-ST-segment-elevation myocardial infarction: the Atherosclerosis Risk
in Communities (ARIC) study. Circulation 2015;131:18431850.
1063. Soliman EZ, Safford MM, Muntner P, Khodneva Y, Dawood FZ, Zakai NA,
Thacker EL, Judd S, Howard VJ, Howard G, Herrington DM, Cushman M.
Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med
2014;174:107114.
1064. Kralev S, Schneider K, Lang S, Suselbeck T, Borggrefe M. Incidence and
severity of coronary artery disease in patients with atrial fibrillation undergoing
first-time coronary angiography. PLoS One 2011;6:e24964.
1065. Guimaraes PO, Zakroysky P, Goyal A, Lopes RD, Kaltenbach LA, Wang TY.
Usefulness of antithrombotic therapy in patients with atrial fibrillation and
acute myocardial infarction. Am J Cardiol 2019;123:12 18.
1066. Erez A, Goldenberg I, Sabbag A, Nof E, Zahger D, Atar S, Pollak A, Dobrecky-
Merye I, Beigel R, Matetzky S, Glikson M, Beinart R. Temporal trends and out-
comes associated with atrial fibrillation observed during acute coronary syn-
drome: real-world data from the Acute Coronary Syndrome Israeli Survey
(ACSIS), 20002013. Clin Cardiol 2017;40:275280.
1067. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U,
Byrne RA, Collet JP, Falk V, Head SJ, Juni P, Kastrati A, Koller A, Kristensen
SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker
S, Yadav R, Zembala MO, ESC Scientific Document Group. 2018 ESC/EACTS
Guidelines on myocardial revascularization. Eur Heart J 2019;40:87165.
1068. Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C,
Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen
T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip
J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ, ESC Scientific Document
Group. 2019 ESC Guidelines for the diagnosis and management of chronic
coronary syndromes. Eur Heart J 2020;41:407477.
1069. Lip GYH, Collet JP, Haude M, Byrne R, Chung EH, Fauchier L, Halvorsen S,
Lau D, Lopez-Cabanillas N, Lettino M, Marin F, Obel I, Rubboli A, Storey RF,
Valgimigli M, Huber K, ESC Scientific Document Group. 2018 Joint European
consensus document on the management of antithrombotic therapy in atrial
fibrillation patients presenting with acute coronary syndrome and/or under-
going percutaneous cardiovascular interventions: a joint consensus document
of the European Heart Rhythm Association (EHRA), European Society of
Cardiology Working Group on Thrombosis, European Association of
Percutaneous Cardiovascular Interventions (EAPCI), and European
Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm
Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), Latin America
Heart Rhythm Society (LAHRS), and Cardiac Arrhythmia Society of Southern
Africa (CASSA). Europace 2019;21:192193.
1070. Gargiulo G, Goette A, Tijssen J, Eckardt L, Lewalter T, Vranckx P, Valgimigli
M. Safety and efficacy outcomes of double vs. triple antithrombotic therapy in
patients with atrial fibrillation following percutaneous coronary intervention: a
systematic review and meta-analysis of non-vitamin K antagonist oral
anticoagulant-based randomized clinical trials. Eur Heart J 2019;40:3757 3767.
1071. Potpara TS, Mujovic N, Proietti M, Dagres N, Hindricks G, Collet JP, Valgimigli
M, Heidbuchel H, Lip GYH. Revisiting the effects of omitting aspirin in com-
bined antithrombotic therapies for atrial fibrillation and acute coronary syn-
dromes or percutaneous coronary interventions: meta-analysis of pooled data
from the PIONEER AF-PCI, RE-DUAL PCI, and AUGUSTUS trials. Europace
2020;22:3346.
1072. Yasuda S, Kaikita K, Akao M, Ako J, Matoba T, Nakamura M, Miyauchi K,
Hagiwara N, Kimura K, Hirayama A, Matsui K, Ogawa H; AFIRE Investigators.
Antithrombotic therapy for atrial fibrillation with stable coronary disease. N
Engl J Med 2019;381:11031113.
1073. Karjalainen PP, Vikman S, Niemela M, Porela P, Ylitalo A, Vaittinen MA,
Puurunen M, Airaksinen TJ, Nyman K, Vahlberg T, Airaksinen KE. Safety of
percutaneous coronary intervention during uninterrupted oral anticoagulant
treatment. Eur Heart J 2008;29:10011010.
1074. Vranckx P, Leebeek FW, Tijssen JG, Koolen J, Stammen F, Herman JP, de
Winter RJ, van THAW, Backx B, Lindeboom W, Kim SY, Kirsch B, van Eickels
M, Misselwitz F, Verheugt FW. Peri-procedural use of rivaroxaban in elective
percutaneous coronary intervention to treat stable coronary artery disease.
The X-PLORER trial. Thromb Haemost 2015;114:258267.
1075. Vranckx P, Verheugt FW, de Maat MP, Ulmans VA, Regar E, Smits P, ten Berg
JM, Lindeboom W, Jones RL, Friedman J, Reilly P, Leebeek FW. A randomised
study of dabigatran in elective percutaneous coronary intervention in stable
coronary artery disease patients. EuroIntervention 2013;8:10521060.
1076. Fiedler KA, Maeng M, Mehilli J, Schulz-Schupke S, Byrne RA, Sibbing D,
Hoppmann P, Schneider S, Fusaro M, Ott I, Kristensen SD, Ibrahim T,
Massberg S, Schunkert H, Laugwitz KL, Kastrati A, Sarafoff N. Duration of tri-
ple therapy in patients requiring oral anticoagulation after drug-eluting stent
implantation: the ISAR-TRIPLE trial. J Am Coll Cardiol 2015;65:16191629.
1077. Lamberts M, Gislason GH, Olesen JB, Kristensen SL, Schjerning Olsen AM,
Mikkelsen A, Christensen CB, Lip GY, Kober L, Torp-Pedersen C, Hansen ML.
Oral anticoagulation and antiplatelets in atrial fibrillation patients after myocar-
dial infarction and coronary intervention. J Am Coll Cardiol 2013;62:981989.
1078. Dewilde WJ, Oirbans T, Verheugt FW, Kelder JC, De Smet BJ, Herrman JP,
Adriaenssens T, Vrolix M, Heestermans AA, Vis MM, Tijsen JG, van ’t Hof
AW, ten Berg JM, for the WOEST Study Investigators. Use of clopidogrel with
or without aspirin in patients taking oral anticoagulant therapy and undergoing
percutaneous coronary intervention: an open-label, randomised, controlled
trial. Lancet 2013;381:11071115.
1079. Cannon CP, Bhatt DL, Oldgren J, Lip GYH, Ellis SG, Kimura T, Maeng M,
Merkely B, Zeymer U, Gropper S, Nordaby M, Kleine E, Harper R, Manassie J,
Januzzi JL, Ten Berg JM, Steg PG, Hohnloser SH; RE-DUAL PCI Steering
Committee Investigators. Dual antithrombotic therapy with dabigatran after
PCI in atrial fibrillation. N Engl J Med 2017;377:1513
1524.
1080. Gibson CM, Mehran R, Bode C, Halperin J, Verheugt FW, Wildgoose P,
Birmingham M, Ianus J, Burton P, van Eickels M, Korjian S, Daaboul Y, Lip
GY, Cohen M, Husted S, Peterson ED, Fox KA. Prevention of bleeding in
patients with atrial fibrillation undergoing PCI. NEnglJMed
2016;375:24232434.
1081. Lopes RD, Heizer G, Aronson R, Vora AN, Massaro T, Mehran R, Goodman
SG, Windecker S, Darius H, Li J, Averkov O, Bahit MC, Berwanger O, Budaj
A, Hijazi Z, Parkhomenko A, Sinnaeve P, Storey RF, Thiele H, Vinereanu D,
Granger CB, Alexander JH; AUGUSTUS Investigators. Antithrombotic therapy
after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med
2019;380:15091524.
1082. Vranckx P, Valgimigli M, Eckardt L, Tijssen J, Lewalter T, Gargiulo G, Batushkin
V, Campo G, Lysak Z, Vakaliuk I, Milewski K, Laeis P, Reimitz PE, Smolnik R,
Zierhut W, Goette A. Edoxaban-based versus vitamin K antagonist-based
antithrombotic regimen after successful coronary stenting in patients with
atrial fibrillation (ENTRUST-AF PCI): a randomised, open-label, phase 3b trial.
Lancet 2019;394:13351343.
1083. Golwala HB, Cannon CP, Steg PG, Doros G, Qamar A, Ellis SG, Oldgren J,
Ten Berg JM, Kimura T, Hohnloser SH, Lip GYH, Bhatt DL. Safety and efficacy
of dual vs. triple antithrombotic therapy in patients with atrial fibrillation fol-
lowing percutaneous coronary intervention: a systematic review and meta-
analysis of randomized clinical trials. Eur Heart J 2018;39:17261735a.
1084. Lopes RD, Hong H, Harskamp RE, Bhatt DL, Mehran R, Cannon CP, Granger
CB, Verheugt FWA, Li J, Ten Berg JM, Sarafoff N, Gibson CM, Alexander JH.
Safety and efficacy of antithrombotic strategies in patients with atrial fibrillation
undergoing percutaneous coronary intervention: a network meta-analysis of
randomized controlled trials. JAMA Cardiol 2019:pii:2735647.
1085. Andreou I, Briasoulis A, Pappas C, Ikonomidis I, Alexopoulos D. Ticagrelor
versus clopidogrel as part of dual or triple antithrombotic therapy: a system-
atic review and meta-analysis. Cardiovasc Drugs Ther 2018;32:287294.
1086. Fu A, Singh K, Abunassar J, Malhotra N, Le May M, Labinaz M, Glover C,
Marquis JF, Froeschl M, Dick A, Hibbert B, Chong AY, So DY; CAPITAL
Investigators. Ticagrelor in triple antithrombotic therapy: predictors of ische-
mic and bleeding complications. Clin Cardiol 2016;39:1923.
1087. Jackson LR, 2nd, Ju C, Zettler M, Messenger JC, Cohen DJ, Stone GW, Baker
BA, Effron M, Peterson ED, Wang TY. Outcomes of patients with acute myo-
cardial infarction undergoing percutaneous coronary intervention receiving an
oral anticoagulant and dual antiplatelet therapy: a comparison of clopidogrel
versus prasugrel from the TRANSLATE-ACS study. JACC Cardiovasc Interv
2015;8:18801889.
1088. Sarafoff N, Martischnig A, Wealer J, Mayer K, Mehilli J, Sibbing D, Kastrati A.
Triple therapy with aspirin, prasugrel, and vitamin K antagonists in patients
with drug-eluting stent implantation and an indication for oral anticoagulation.
J Am Coll Cardiol 2013;61:20602066.
1089. Verlinden NJ, Coons JC, Iasella CJ, Kane-Gill SL. Triple antithrombotic therapy
with aspirin, P2Y12 inhibitor, and warfarin after percutaneous coronary
114 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
intervention: an evaluation of prasugrel or ticagrelor versus clopidogrel. J
Cardiovasc Pharmacol Ther 2017;22:546 551.
1090. Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L,
Haeusler KG, Oldgren J, Reinecke H, Roldan-Schilling V, Rowell N, Sinnaeve P,
Collins R, Camm AJ, Heidbuchel H, ESC Scientific Document Group. The
2018 European Heart Rhythm Association Practical Guide on the use of non-
vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur
Heart J 2018;39:13301393.
1091. Pikija S, Sztriha LK, Sebastian Mutzenbach J, Golaszewski SM, Sellner J.
Idarucizumab in dabigatran-treated patients with acute ischemic stroke receiv-
ing alteplase: a systematic review of the available evidence. CNS Drugs
2017;31:747757.
1092. Saxena R, Lewis S, Berge E, Sandercock PA, Koudstaal PJ. Risk of early death
and recurrent stroke and effect of heparin in 3169 patients with acute ische-
mic stroke and atrial fibrillation in the International Stroke Trial. Stroke
2001;32:23332337.
1093. Hart RG, Coull BM, Hart D. Early recurrent embolism associated with non-
valvular atrial fibrillation: a retrospective study. Stroke 1983;14:688693.
1094. Berge E, Abdelnoor M, Nakstad PH, Sandset PM. Low molecular-weight hepa-
rin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation:
a double-blind randomised study. HAEST Study Group. Heparin in Acute
Embolic Stroke Trial. Lancet 2000;355:12051210.
1095. Paciaroni M, Agnelli G, Micheli S, Caso V. Efficacy and safety of anticoagulant
treatment in acute cardioembolic stroke: a meta-analysis of randomized con-
trolled trials. Stroke 2007;38:423430.
1096. von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD,
Treurniet KM, Majoie CB, Marquering HA, Mazya MV, San Roman L, Saver JL,
Strbian D, Whiteley W, Hacke W. The Heidelberg Bleeding Classification:
classification of bleeding events after ischemicstroke and reperfusion therapy.
Stroke 2015;46:29812986.
1097. Paciaroni M, Agnelli G, Corea F, Ageno W, Alberti A, Lanari A, Caso V,
Micheli S, Bertolani L, Venti M, Palmerini F, Biagini S, Comi G, Previdi P,
Silvestrelli G. Early hemorrhagic transformation of brain infarction: rate, pre-
dictive factors, and influence on clinical outcome: results of a prospective mul-
ticenter study. Stroke 2008;39:22492256.
1098. Kablau M, Kreisel SH, Sauer T, Binder J, Szabo K, Hennerici MG, Kern R.
Predictors and early outcome of hemorrhagic transformation after acute
ischemic stroke. Cerebrovasc Dis 2011;32:334341.
1099. Seiffge DJ, Werring DJ, Paciaroni M, Dawson J, Warach S, Milling TJ, Engelter
ST, Fischer U, Norrving B. Timing of anticoagulation after recent ischaemic
stroke in patients with atrial fibrillation. Lancet Neurol 2019;18:117126.
1100. Paciaroni M, Agnelli G, Falocci N, Tsivgoulis G, Vadikolias K, Liantinioti C,
Chondrogianni M, Bovi P, Carletti M, Cappellari M, Zedde M, Ntaios G,
Karagkiozi E, Athanasakis G, Makaritsis K, Silvestrelli G, Lanari A, Ciccone A,
Putaala J, Tomppo L, Tatlisumak T, Abdul-Rahim AH, Lees KR, Alberti A,
Venti M, Acciarresi M, D’Amore C, Becattini C, Mosconi MG, Cimini LA,
Soloperto R, Masotti L, Vannucchi V, Lorenzini G, Tassi R, Guideri F, Acampa
M, Martini G, Sohn SI, Marcheselli S, Mumoli N, De Lodovici ML, Bono G,
Furie KL, Tadi P, Yaghi S, Toni D, Letteri F, Tassinari T, Kargiotis O, Lotti EM,
Flomin Y, Mancuso M, Maccarrone M, Giannini N, Bandini F, Pezzini A, Poli L,
Padovani A, Scoditti U, Denti L, Consoli D, Galati F, Sacco S, Carolei A, Tiseo
C, Gourbali V, Orlandi G, Giuntini M, Chiti A, Giorli E, Gialdini G, Corea F,
Ageno W, Bellesini M, Colombo G, Monaco S, Maimone Baronello M,
Karapanayiotides T, Caso V. Early Recurrence and Major Bleeding in Patients
With Acute Ischemic Stroke and Atrial Fibrillation Treated With Non-
Vitamin-K Oral Anticoagulants (RAF-NOACs) study. J Am Heart Assoc 2017;6.
1101. Seiffge DJ, Traenka C, Polymeris A, Hert L, Peters N, Lyrer P, Engelter ST,
Bonati LH, De Marchis GM. Early start of DOAC after ischemic stroke: risk of
intracranial hemorrhage and recurrent events. Neurology 2016;87:18561862.
1102. Arihiro S, Todo K, Koga M, Furui E, Kinoshita N, Kimura K, Yamagami H,
Terasaki T, Yoshimura S, Shiokawa Y, Kamiyama K, Takizawa S, Okuda S,
Okada Y, Nagakane Y, Kameda T, Hasegawa Y, Shibuya S, Ito Y, Nakashima T,
Takamatsu K, Nishiyama K, Matsuki T, Homma K, Takasugi J, Tokunaga K, Sato
S, Kario K, Kitazono T, Toyoda K; SAMURAI Study Investigators. Three-month
risk-benefit profile of anticoagulation after stroke with atrial fibrillation: the
SAMURAI-Nonvalvular Atrial Fibrillation (NVAF) study. Int J Stroke
2016;11:565574.
1103. Hong KS, Kwon SU, Lee SH, Lee JS, Kim YJ, Song TJ, Kim YD, Park MS, Kim
EG, Cha JK, Sung SM, Yoon BW, Bang OY, Seo WK, Hwang YH, Ahn SH,
Kang DW, Kang HG, Yu KH, Phase 2 exploratory clinical study to assess the
effects of xarelto versus warfarin on ischemia B, hospital stay in acute cerebral
infarction patients with non-valvular atrial fibrillation study G. Rivaroxaban vs
warfarin sodium in the ultra-early period after atrial fibrillation-related mild
ischemic stroke: a randomized clinical trial. JAMA Neurol 2017;74:12061215.
1104. Ntaios G, Papavasileiou V, Diener HC, Makaritsis K, Michel P. Nonvitamin-K-
antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation
and previous stroke or transient ischemic attack: an updated systematic review
and meta-analysis of randomized controlled trials. Int J Stroke
2017;12:589596.
1105. Gonzalez ME, Klein FR, Riccio PM, Cassara FP, Munoz Giacomelli F, Racosta
JM, Roberts ES, Sposato, LA. Atrial fibrillation detected after acute ischemic
stroke: evidence supporting the neurogenic hypothesis. J Stroke Cerebrovasc Dis
2013;22:e486491.
1106. Sposato LA, Cerasuolo JO, Cipriano LE, Fang J, Fridman S, Paquet M, Saposnik
G. Atrial fibrillation detected after stroke is related to a low risk of ischemic
stroke recurrence. Neurology 2018;90:e924e931.
1107. Steinberg BA, Shrader P, Pieper K, Thomas L, Allen LA, Ansell J, Chan PS,
Ezekowitz MD, Fonarow GC, Freeman JV, Gersh BJ, Kowey PR, Mahaffey KW,
NaccarelliGV,ReiffelJA,Singer,DE,PetersonED,Piccini,JP;OutcomesRegistry
for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) II Investigators.
Frequency and outcomes of reduced dose non-vitamin K antagonist anticoagulants:
results from ORBIT-AF II (the Outcomes Registry for Better Informed Treatment
of Atrial Fibrillation II). J Am Heart Assoc 2018;7:e007633.
1108. Hart RG, Sharma M, Mundl H, Kasner SE, Bangdiwala SI, Berkowitz SD,
Swaminathan B, Lavados P, Wang Y, Wang Y, Davalos A, Shamalov N, Mikulik
R, Cunha L, Lindgren A, Arauz A, Lang W, Czlonkowska A, Eckstein J,
Gagliardi RJ, Amarenco P, Ameriso SF, Tatlisumak T, Veltkamp R, Hankey GJ,
Toni D, Bereczki D, Uchiyama S, Ntaios G, Yoon BW, Brouns R, Endres M,
Muir KW, Bornstein N, Ozturk S, O’Donnell MJ, De Vries Basson MM, Pare
G, Pater C, Kirsch B, Sheridan P, Peters G, Weitz JI, Peacock WF, Shoamanesh
A, Benavente OR, Joyner C, Themeles E, Connolly SJ; NAVIGATE ESUS
Investigators. Rivaroxaban for Stroke Prevention after Embolic Stroke of
Undetermined Source. N Engl J Med 2018;378:21912201.
1109. Diener HC, Sacco RL, Easton JD, Granger CB, Bernstein RA, Uchiyama S,
Kreuzer J, Cronin L, Cotton D, Grauer C, Brueckmann M, Chernyatina M,
Donnan G, Ferro JM, Grond M, Kallmunzer B, Krupinski J, Lee BC, Lemmens
R, Masjuan J, Odinak M, Saver JL, Schellinger PD, Toni D, Toyoda K; RE-
SPECT ESUS Steering Committee Investigators. Dabigatran for prevention of
stroke after embolic stroke of undetermined source. N Engl J Med
2019;380:19061917.
1110. Healey JS, Gladstone DJ, Swaminathan B, Eckstein J, Mundl H, Epstein AE,
Haeusler KG, Mikulik R, Kasner SE, Toni D, Arauz A, Ntaios G, Hankey GJ,
Perera K, Pagola J, Shuaib A, Lutsep H, Yang X, Uchiyama S, Endres M, Coutts
SB, Karlinski M, Czlonkowska A, Molina CA, Santo G, Berkowitz SD, Hart RG,
Connolly SJ. Recurrent stroke with rivaroxaban compared with aspirin accord-
ing to predictors of atrial fibrillation: secondary analysis of the NAVIGATE
ESUS randomized clinical trial. JAMA Neurol
2019.
1111. Geisler T, Poli S, Meisner C, Schreieck J, Zuern CS, Nagele T, Brachmann J,
Jung W, Gahn G, Schmid E, Baezner H, Keller T, Petzold GC, Schrickel JW,
Liman J, Wachter R, Schon F, Schabet M, Lindner A, Ludolph AC, Kimmig H,
Jander S, Schlegel U, Gawaz M, Ziemann U. Apixaban for treatment of embolic
stroke of undetermined source (ATTICUS randomized trial): rationale and
study design. Int J Stroke 2017;12:985990.
1112. Li Y-G, Bisson A, Bodin A, Herbert J, Grammatico-Guillon L, Joung B, Wang
Y-T, Lip GYH, Fauchier L. C2HEST score and prediction of incident atrial
fibrillation in poststroke patients: a French nationwide study. J Am Heart Assoc
2019;8:e012546.
1113. Gladstone DJ, Spring M, Dorian P, Panzov V, Thorpe KE, Hall J, Vaid H,
O’Donnell M, Laupacis A, Cote R, Sharma M, Blakely JA, Shuaib A, Hachinski
V, Coutts SB, Sahlas DJ, Teal P, Yip S, Spence JD, Buck B, Verreault S,
Casaubon LK, Penn A, Selchen D, Jin A, Howse D, Mehdiratta M, Boyle K,
Aviv R, Kapral MK, Mamdani M; EMBRACE Investigators and Coordinators.
Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med
2014;370:24672477.
1114. Sanna T, Diener HC, Passman RS, Di Lazzaro V, Bernstein RA, Morillo CA,
Rymer MM, Thijs V, Rogers T, Beckers F, Lindborg K, Brachmann J; CRYSTAL
AF Investigators. Cryptogenic stroke and underlying atrial fibrillation. N Engl J
Med 2014;370:24782486.
1115. Wachter R, Groschel K, Gelbrich G, Hamann GF, Kermer P, Liman J, Seegers
J, Wasser K, Schulte A, Jurries F, Messerschmid A, Behnke N, Groschel S,
Uphaus T, Grings A, Ibis T, Klimpe S, Wagner-Heck M, Arnold M, Protsenko
E, Heuschmann PU, Conen D, Weber-Kruger M; Find-AF(randomised)
Investigators and Coordinators. Holter-electrocardiogram-monitoring in
patients with acute ischaemic stroke (Find-AFRANDOMISED): an open-label
randomised controlled trial. Lancet Neurol 2017;16:282290.
1116. Grond M, Jauss M, Hamann G, Stark E, Veltkamp R, Nabavi D, Horn M,
Weimar C, Kohrmann M, Wachter R, Rosin L, Kirchhof P. Improved detection
of silent atrial fibrillation using 72-hour Holter ECG in patients with ischemic
stroke: a prospective multicenter cohort study. Stroke 2013;44:33573364.
1117. Kishore A, Vail A, Majid A, Dawson J, Lees KR, Tyrrell PJ, Smith CJ. Detection
of atrial fibrillation after ischemic stroke or transient ischemic attack: a system-
atic review and meta-analysis. Stroke 2014;45:520526.
ESC Guidelines 115

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1118. Sposato LA, Cipriano LE, Saposnik G, Ruiz Vargas E, Riccio PM, Hachinski V.
Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: a sys-
tematic review and meta-analysis. Lancet Neurol 2015;14:377387.
1119. Thijs VN, Brachmann J, Morillo CA, Passman RS, Sanna T, Bernstein RA,
Diener HC, Di Lazzaro V, Rymer MM, Hogge L, Rogers TB, Ziegler PD, Assar
MD. Predictors for atrial fibrillation detection after cryptogenic stroke: results
from CRYSTAL AF. Neurology 2016;86:261269.
1120. Levin LA, Husberg M, Sobocinski PD, Kull VF, Friberg L, Rosenqvist M,
Davidson T. A cost-effectiveness analysis of screening for silent atrial fibrilla-
tion after ischaemic stroke. Europace 2015;17:207214.
1121. Yong JH, Thavorn K, Hoch JS, Mamdani M, Thorpe KE, Dorian P, Sharma M,
Laupacis A, Gladstone DJ, on behalf of the EMBRACE Steering Committee.
Potential cost-effectiveness of ambulatory cardiac rhythm monitoring after
cryptogenic stroke. Stroke 2016;47:2380 2385.
1122. Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in
the risk of intracranial hemorrhage among patients with atrial fibrillation. JAm
Coll Cardiol 2007;50:309315.
1123. Wilson D, Ambler G, Lee KJ, Lim JS, Shiozawa M, Koga M, Li L, Lovelock C,
Chabriat H, Hennerici M, Wong YK, Mak HKF, Prats-Sanchez L, Martinez-
Domeno A, Inamura S, Yoshifuji K, Arsava EM, Horstmann S, Purrucker J, Lam
BYK, Wong A, Kim YD, Song TJ, Schrooten M, Lemmens R, Eppinger S,
Gattringer T, Uysal E, Tanriverdi Z, Bornstein NM, Assayag EB, Hallevi H,
Tanaka J, Hara H, Coutts SB, Hert L, Polymeris A, Seiffge DJ, Lyrer P, Algra A,
Kappelle J, Al-Shahi Salman R, Jager HR, Lip GYH, Mattle HP, Panos LD, Mas
JL, Legrand L, Karayiannis C, Phan T, Gunkel S, Christ N, Abrigo J, Leung T,
Chu W, Chappell F, Makin S, Hayden D, Williams DJ, Kooi ME, van Dam-
Nolen DHK, Barbato C, Browning S, Wiegertjes K, Tuladhar AM, Maaijwee N,
Guevarra C, Yatawara C, Mendyk AM, Delmaire C, Kohler S, van
Oostenbrugge R, Zhou Y, Xu C, Hilal S, Gyanwali B, Chen C, Lou M, Staals J,
Bordet R, Kandiah N, de Leeuw FE, Simister R, van der Lugt A, Kelly PJ,
Wardlaw JM, Soo Y, Fluri F, Srikanth V, Calvet D, Jung S, Kwa VIH, Engelter
ST, Peters N, Smith EE, Yakushiji Y, Orken DN, Fazekas F, Thijs V, Heo JH,
Mok V, Veltkamp R, Ay H, Imaizumi T, Gomez-Anson B, Lau KK, Jouvent E,
Rothwell PM, Toyoda K, Bae HJ, Marti-Fabregas J, Werring DJ. Cerebral
microbleeds and stroke risk after ischaemic stroke or transient ischaemic
attack: a pooled analysis of individual patient data from cohort studies. Lancet
Neurol 2019;18:653665.
1124. Murthy SB, Gupta A, Merkler AE, Navi BB, Mandava P, Iadecola C, Sheth KN,
Hanley DF, Ziai WC, Kamel H. Restarting anticoagulant therapy after intracra-
nial hemorrhage: a systematic review and meta-analysis. Stroke
2017;48:15941600.
1125. Diener HC, Connolly SJ, Ezekowitz MD, Wallentin L, Reilly PA, Yang S, Xavier
D, Di Pasquale G, Yusuf S. Dabigatran compared with warfarin in patients with
atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup
analysis of the RE-LY trial. Lancet Neurol 2010;9:11571163.
1126. Easton JD, Lopes RD, Bahit MC, Wojdyla DM, Granger CB, Wallentin L,
Alings M, Goto S, Lewis BS, Rosenqvist M, Hanna M, Mohan P, Alexander JH,
Diener HC; ARISTOTLE Committees and Investigators. Apixaban compared
with warfarin in patients with atrial fibrillation and previous stroke or transient
ischaemic attack: a subgroup analysis of the ARISTOTLE trial. Lancet Neurol
2012;11:503511.
1127. Hankey GJ, Patel MR, Stevens SR, Becker RC, Breithardt G, Carolei A, Diener
HC, Donnan GA, Halperin JL, Mahaffey KW, Mas JL, Massaro A, Norrving B,
Nessel CC, Paolini JF, Roine RO, Singer DE, Wong L, Califf RM, Fox KA,
Hacke W; ROCKET AF Steering Committee Investigators. Rivaroxaban com-
pared with warfarin in patients with atrial fibrillation and previous stroke or
transient ischaemic attack: a subgroup analysis of ROCKET AF. Lancet Neurol
2012;11:315322.
1128. Rost NS, Giugliano RP, Ruff CT, Murphy SA, Crompton AE, Norden AD,
Silverman S, Singhal AB, Nicolau JC, SomaRaju B, Mercuri MF, Antman EM,
Braunwald E. Outcomes with edoxaban versus warfarin in patients with pre-
vious cerebrovascular events: findings from ENGAGE AF-TIMI 48 (Effective
Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation-
Thrombolysis in Myocardial Infarction 48). Stroke 2016;47
:20752082.
1129. Diener HC, Eikelboom J, Connolly SJ, Joyner CD, Hart RG, Lip GY, O’Donnell
M, Hohnloser SH, Hankey GJ, Shestakovska O, Yusuf S. Apixaban versus
aspirin in patients with atrial fibrillation and previous stroke or transient
ischaemic attack: a predefined subgroup analysis from AVERROES, a rando-
mised trial. Lancet Neurol 2012;11:225231.
1130. Secondary prevention in non-rheumatic atrial fibrillation after transient ischae-
mic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study
Group. Lancet 1993;342:12551262.
1131. Cuker A. Laboratory measurement of the non-vitamin K antagonist oral anti-
coagulants: selecting the optimal assay based on drug, assay availability, and
clinical indication. J Thromb Thrombolysis 2016;41:241 247.
1132. Salmonson T, Dogne JM, Janssen H, Garcia Burgos J, Blake P. Non-vitamin-K
oral anticoagulants and laboratory testing: now and in the future: views from a
workshop at the European Medicines Agency (EMA). Eur Heart J Cardiovasc
Pharmacother 2017;3:4247.
1133. Chai-Adisaksopha C, Hillis C, Lim W, Boonyawat K, Moffat K, Crowther M.
Hemodialysis for the treatment of dabigatran-associated bleeding: a case
report and systematic review. J Thromb Haemost 2015;13:17901798.
1134. Anderson I, Cifu AS. Management of bleeding in patients taking oral anticoagu-
lants. JAMA 2018;319:20322033.
1135. Milling TJ Jr, Refaai MA, Sarode R, Lewis B, Mangione A, Durn BL, Harman A,
Lee ML, Goldstein JN. Safety of a four-factor prothrombin complex concen-
trate versus plasma for vitamin K antagonist reversal: an integrated analysis of
two phase IIIb clinical trials. Acad Emerg Med 2016;23:466475.
1136. Pollack CV Jr, Reilly PA, van Ryn J, Eikelboom JW, Glund S, Bernstein RA,
Dubiel R, Huisman MV, Hylek EM, Kam CW, Kamphuisen PW, Kreuzer J, Levy
JH, Royle G, Sellke FW, Stangier J, Steiner T, Verhamme P, Wang B, Young L,
Weitz JI. Idarucizumab for dabigatran reversal full cohort analysis. N Engl J
Med 2017;377:431441.
1137. Connolly SJ, Crowther M, Eikelboom JW, Gibson CM, Curnutte JT, Lawrence
JH, Yue P, Bronson MD, Lu G, Conley PB, Verhamme P, Schmidt J,
Middeldorp S, Cohen AT, Beyer-Westendorf J, Albaladejo P, Lopez-Sendon J,
Demchuk AM, Pallin DJ, Concha M, Goodman S, Leeds J, Souza S, Siegal DM,
Zotova E, Meeks B, Ahmad S, Nakamya J, Milling TJ Jr; ANNEXA Investigators.
Full study report of andexanet alfa for bleeding associated with factor Xa
inhibitors. N Engl J Med 2019;380:13261335.
1138. Levi M, Moore KT, Castillejos CF, Kubitza D, Berkowitz SD, Goldhaber SZ,
Raghoebar M, Patel MR, Weitz JI, Levy JH. Comparison of three-factor and
four-factor prothrombin complex concentrates regarding reversal of the anti-
coagulant effects of rivaroxaban in healthy volunteers. J Thromb Haemost
2014;12:14281436.
1139. Nagalla S, Thomson L, Oppong Y, Bachman B, Chervoneva I, Kraft WK.
Reversibility of apixaban anticoagulation with a four-factor prothrombin com-
plex concentrate in healthy volunteers. Clin Transl Sci 2016;9:176180.
1140. Zahir H, Brown KS, Vandell AG, Desai M, Maa JF, Dishy V, Lomeli B, Feussner
A, Feng W, He L, Grosso MA, Lanz HJ, Antman EM. Edoxaban effects on
bleeding following punch biopsy and reversal by a 4-factor prothrombin com-
plex concentrate. Circulation 2015;131:8290.
1141. Isnard R, Bauer F, Cohen-Solal A, Damy T, Donal E, Galinier M, Hagege A,
Jourdain P, Leclercq C, Sabatier R, Trochu JN, Cohen A. Non-vitamin K antagonist
oral anticoagulants and heart failure. Arch Cardiovasc Dis 2016;109:641650.
1142. Xiong Q, Lau YC, Senoo K, Lane DA, Hong K, Lip GY. Non-vitamin K antago-
nist oral anticoagulants (NOACs) in patients with concomitant atrial fibrilla-
tion and heart failure: a systemic review and meta-analysis of randomized
trials. Eur J Heart Fail 2015;17:11921200.
1143. Ezekowitz JA, O’Meara E, McDonald MA, Abrams H, Chan M, Ducharme A,
Giannetti N, Grzeslo A, Hamilton PG, Heckman GA, Howlett JG, Koshman
SL, Lepage S, McKelvie RS, Moe GW, Rajda M, Swiggum E, Virani SA, Zieroth
S, Al-Hesayen A, Cohen-Solal A, D’Astous M, De S, Estrella-Holder E, Fremes
S, Green L, Haddad H, Harkness K, Hernandez AF, Kouz S, LeBlanc MH,
Masoudi FA, Ross HJ, Roussin A, Sussex B. 2017 comprehensive update of the
Canadian Cardiovascular Society Guidelines for the management of heart fail-
ure. Can J Cardiol 2017;33:13421433.
1144. Atherton JJ, Sindone A, De Pasquale CG, Driscoll A, MacDonald PS, Hopper I,
Kistler PM, Briffa T, Wong J, Abhayaratna W, Thomas L, Audehm R, Newton
P, O’Loughlin J, Branagan M, Connell C. National Heart Foundation of
Australia and Cardiac Society of Australia and New Zealand: Guidelines for
the prevention, detection, and management of heart failure in Australia 2018.
Heart Lung Circ 2018;27:11231208.
1145. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V,
Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C,
Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM,
Ruschitzka F, Rutten FH, van der Meer P; ESC Scientific Document Group.
2016 ESC Guidelines for the diagnosis and treatment of acute and chronic
heart failure: the Task Force for the diagnosis and treatment of acute and
chronic heart failure of the European Society of Cardiology (ESC). Developed
with the special contribution of the Heart Failure Association (HFA) of the
ESC. Eur Heart J 2016;37:21292200.
1146. Kelly JP, DeVore AD, Wu J, Hammill BG, Sharma A, Cooper LB, Felker GM,
Piccini JP, Allen LA, Heidenreich PA, Peterson ED, Yancy CW, Fonarow GC,
Hernandez AF. Rhythm control versus rate control in patients with atrial fibril-
lation and heart failure with preserved ejection fraction: insights from Get
With The Guidelines-Heart Failure. J Am Heart Assoc 2019;8:e011560.
1147. Filippatos G, Farmakis D. How to use beta-blockers in heart failure with
reduced ejection fraction and atrial fibrillation. J Am Coll Cardiol
2017;69:28972900.
116 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1148. Nielsen PB, Larsen TB, Gorst-Rasmussen A, Skjoth F, Lip GY. beta-Blockers in
atrial fibrillation patients with or without heart failure: association with mortal-
ity in a nationwide cohort study. Circ Heart Fail 2016;9:e002597.
1149. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano
M. Burden of valvular heart diseases: a population-based study. Lancet
2006;368:10051011.
1150. Barbash IM, Minha S, Ben-Dor I, Dvir D, Torguson R, Aly M, Bond E, Satler LF,
Pichard AD, Waksman R. Predictors and clinical implications of atrial fibrilla-
tion in patients with severe aortic stenosis undergoing transcatheter aortic
valve implantation. Catheter Cardiovasc Interv 2015;85:468477.
1151. Eguchi K, Ohtaki E, Matsumura T, Tanaka K, Tohbaru T, Iguchi N, Misu K,
Asano R, Nagayama M, Sumiyoshi T, Kasegawa H, Hosoda S. Pre-operative
atrial fibrillation as the key determinant of outcome of mitral valve repair for
degenerative mitral regurgitation. Eur Heart J 2005;26:18661872.
1152. Maan A, Heist EK, Passeri J, Inglessis I, Baker J, Ptaszek L, Vlahakes G, Ruskin
JN, Palacios I, Sundt T, Mansour M. Impact of atrial fibrillation on outcomes in
patients who underwent transcatheter aortic valve replacement. Am J Cardiol
2015;115:220226.
1153. Ngaage DL, Schaff HV, Barnes SA, Sundt TM 3rd, Mullany CJ, Dearani JA, Daly
RC, Orszulak TA. Prognostic implications of preoperative atrial fibrillation in
patients undergoing aortic valve replacement: is there an argument for con-
comitant arrhythmia surgery?Ann Thorac Surg 2006;82:13921399.
1154. Ngaage DL, Schaff HV, Mullany CJ, Barnes S, Dearani JA, Daly RC, Orszulak
TA, Sundt TM 3rd. Influence of preoperative atrial fibrillation on late results of
mitral repair: is concomitant ablation justified?Ann Thorac Surg
2007;84:434442.
1155. Lim E, Barlow CW, Hosseinpour AR, Wisbey C, Wilson K, Pidgeon W,
Charman S, Barlow JB, Wells FC. Influence of atrial fibrillation on outcome fol-
lowing mitral valve repair. Circulation 2001;104:I5963.
1156. Philippart R, Brunet-Bernard A, Clementy N, Bourguignon T, Mirza A, Babuty
D, Angoulvant D, Lip GY, Fauchier L. Prognostic value of CHA2DS2-VASc
score in patients with ‘non-valvular atrial fibrillation’ and valvular heart disease:
the Loire Valley Atrial Fibrillation Project. Eur Heart J 2015;36:18221830.
11547. Lip GYH, Jensen M, Melgaard L, Skjoth F, Nielsen PB, Larsen TB. Stroke and
bleeding risk scores in patients with atrial fibrillation and valvular heart dis-
ease: evaluating ‘valvular heart disease’ in a nationwide cohort study.
Europace 2019;21:3340.
1158. Szekely P. Systemic embolism and anticoagulant prophylaxis in rheumatic heart
disease. Br Med J 1964;1:12091212.
1159. Philippart R, Brunet-Bernard A, Clementy N, Bourguignon T, Mirza A,
Angoulvant D, Babuty D, Lip GY, Fauchier L. Oral anticoagulation, stroke and
thromboembolism in patients with atrial fibrillation and valve bioprosthesis.
The Loire Valley Atrial Fibrillation Project. Thromb Haemost
2016;115:10561063.
1160. Siontis KC, Yao X, Gersh BJ, Noseworthy PA. Direct oral anticoagulants in
patients with atrial fibrillation and valvular heart disease other than significant
mitral stenosis and mechanical valves: a meta-analysis. Circulation
2017;135:714716.
1161. Kim JY, Kim SH, Myong JP, Kim YR, Kim TS, Kim JH, Jang SW, Oh YS, Lee MY,
Rho TH. Outcomes of direct oral anticoagulants in patients with mitral steno-
sis. J Am Coll Cardiol 2019;73:11231131.
1162. Bisson A, Bodin A, Clementy N, Bernard A, Babuty D, Lip GYH, Fauchier L.
Stroke, thromboembolism and bleeding in patients with atrial fibrillation
according to the EHRA valvular heart disease classification. Int J Cardiol
2018;260:9398.
1163. Seeger J, Gonska B, Rodewald C, Rottbauer W, Wohrle J. Apixaban in patients
with atrial fibrillation after transfemoral aortic valve replacement. JACC
Cardiovasc Interv 2017;10:6674.
1164. Dangas GD, Tijssen JGP, Wohrle J, Sondergaard L, Gilard M, Mollmann H,
Makkar RR, Herrmann HC, Giustino G, Baldus S, De Backer O, Guimaraes
AHC, Gullestad L, Kini A, von Lewinski D, Mack M, Moreno R, Schafer U,
Seeger J, Tchetche D, Thomitzek K, Valgimigli M, Vranckx P, Welsh RC,
Wildgoose P, Volkl AA, Zazula A, van Amsterdam RGM, Mehran R,
Windecker S, for the GALILEO Investigators. A controlled trial of rivaroxa-
ban after transcatheter aortic-valve replacement. NEnglJMed
2020;382:120129.
1165. Eikelboom JW, Connolly SJ, Brueckmann M, Granger CB, Kappetein AP, Mack
MJ, Blatchford J, Devenny K, Friedman J, Guiver K, Harper R, Khder Y,
Lobmeyer MT, Maas H, Voigt JU, Simoon ML, Van de Werf, F; RE-ALIGN
Investigators. Dabigatran versus warfarin in patients with mechanical heart
valves. N Engl J Med 2013;369:12061214.
1166. Potpara TS, Ferro CJ, Lip GYH. Use of oral anticoagulants in patients with
atrial fibrillation and renal dysfunction. Nat Rev Nephrol 2018;14:337351.
1167. Albertsen IE, Rasmussen LH, Overvad TF, Graungaard T, Larsen TB, Lip GY.
Risk of stroke or systemic embolism in atrial fibrillation patients treated with
warfarin: a systematic review and meta-analysis. Stroke 2013;44:13291336.
1168. Olesen JB, Lip GY, Kamper AL, Hommel K, Kober L, Lane DA, Lindhardsen J,
Gislason GH, Torp-Pedersen C. Stroke and bleeding in atrial fibrillation with
chronic kidney disease. N Engl J Med 2012;367:625635.
1169. Hart RG, Eikelboom JW, Brimble KS, McMurtry MS, Ingram AJ. Stroke preven-
tion in atrial fibrillation patients with chronic kidney disease. Can J Cardiol
2013;29:S7178.
1170. Zimmerman D, Sood MM, Rigatto C, Holden RM, Hiremath S, Clase CM.
Systematic review and meta-analysis of incidence, prevalence and outcomes of
atrial fibrillation in patients on dialysis. Nephrol Dial Transplant
2012;27:38163822.
1171. Banerjee A, Fauchier L, Vourc’h P, Andres CR, Taillandier S, Halimi JM, Lip
GYH. A prospective study of estimated glomerular filtration rate and out-
comes in patients with atrial fibrillation: the Loire Valley Atrial Fibrillation
Project. Chest 2014;145:1370
1382.
1172. Fauchier L, Bisson A, Clementy N, Vourc’h P, Angoulvant D, Babuty D, Halimi
JM, Lip GYH. Changes in glomerular filtration rate and outcomes in patients
with atrial fibrillation. Am Heart J 2018;198:3945.
1173. Bohula EA, Giugliano RP, Ruff CT, Kuder JF, Murphy SA, Antman EM,
Braunwald E. Impact of renal function on outcomes with edoxaban in the
ENGAGE AF-TIMI 48 trial. Circu lation 2016;134:2436.
1174. Hijazi Z, Hohnloser SH, Oldgren J, Andersson U, Connolly SJ, Eikelboom JW,
Ezekowitz MD, Reilly PA, Siegbahn A, Yusuf S, Wallentin L. Efficacy and safety
of dabigatran compared with warfarin in relation to baseline renal function in
patients with atrial fibrillation: a RE-LY (Randomized Evaluation of Long-term
Anticoagulation Therapy) trial analysis. Circulation 2014;129:961970.
1175. Fox KA, Piccini JP, Wojdyla D, Becker RC, Halperin JL, Nessel CC, Paolini JF,
Hankey GJ, Mahaffey KW, Patel MR, Singer DE, Califf RM. Prevention of stroke
and systemic embolism with rivaroxaban compared with warfarin in patients
with non-valvular atrial fibrillation and moderate renal impairment. Eur Heart J
2011;32:23872394.
1176. Hohnloser SH, Hijazi Z, Thomas L, Alexander JH, Amerena J, Hanna M, Keltai
M, Lanas F, Lopes RD, Lopez-Sendon J, Granger CB, Wallentin L. Efficacy of
apixaban when compared with warfarin in relation to renal function in patients
with atrial fibrillation: insights from the ARISTOTLE trial. Eur Heart J
2012;33:28212830.
1177. Coleman CI, Kreutz R, Sood NA, Bunz TJ, Eriksson D, Meinecke AK, Baker
WL. Rivaroxaban versus warfarin in patients with nonvalvular atrial fibrillation
and severe kidney disease or undergoing hemodialysis. Am J Med
2019;132:10781083.
1178. Ha JT, Neuen BL, Cheng LP, Jun M, Toyama T, Gallagher MP, Jardine MJ, Sood
MM, Garg AX, Palmer SC, Mark PB, Wheeler DC, Jha V, Freedman B, Johnson
DW, Perkovic V, Badve SV. Benefits and harms of oral anticoagulant therapy
in chronic kidney disease: a systematic review and meta-analysis. Ann Intern
Med 2019;171:181189.
1179. Pokorney SD. RENal hemodialysis patients ALlocated apixaban versus warfarin
in Atrial Fibrillation (RENAL-AF). Presentation at the American Heart
Association Annual Scientific Sessions (AHA 2019), Philadelphia, PA, 16
November 2019.
1180. Violi F, Davi G, Hiatt W, Lip GY, Corazza GR, Perticone F, Proietti M,
Pignatelli P, Vestri AR, Basili S; ARAPACIS Study Investigators. Prevalence of
peripheral artery disease by abnormal ankle-brachial index in atrial fibrillation:
implications for risk and therapy. J Am Coll Cardiol 2013;62:22552256.
1181. Bruere H, Fauchier L, Bernard Brunet A, Pierre B, Simeon E, Babuty D,
Clementy N. History of thyroid disorders in relation to clinical outcomes in
atrial fibrillation. Am J Med 2015;128:3037.
1182. Nakazawa HK, Sakurai K, Hamada N, Momotani N, Ito K. Management of
atrial fibrillation in the post-thyrotoxic state. Am J Med 1982;72:903906.
1183. Kristensen SL, Lindhardsen J, Ahlehoff O, Erichsen R, Lamberts M, Khalid U,
Torp-Pedersen C, Nielsen OH, Gislason GH, Hansen PR. Increased risk of
atrial fibrillation and stroke during active stages of inflammatory bowel disease:
a nationwide study. Europace 2014;16:477484.
1184. Holster IL, Valkhoff VE, Kuipers EJ, Tjwa ETTL. New oral anticoagulants
increase risk for gastrointestinal bleeding: a systematic review and meta-analy-
sis. Gastroenterology 2013;145:105112.e15.
1185. Caldeira D, Barra M, Ferreira A, Rocha A, Augusto A, Pinto FJ, Costa J,
Ferreira JJ. Systematic review with meta-analysis: the risk of major gastrointes-
tinal bleeding with non-vitamin K antagonist oral anticoagulants. Aliment
Pharmacol Ther 2015;42:12391249.
1186. Kolb JM, Flack KF, Chatterjee-Murphy P, Desai J, Wallentin LC, Ezekowitz M,
Connolly S, Reilly P, Brueckmann M, Ilgenfritz J, Aisenberg J. Locations and
mucosal lesions responsible for major gastrointestinal bleeding in patients on
warfarin or dabigatran. Dig Dis Sci 2018;63:18781889.
1187. Chai-Adisaksopha C, Hillis C, Monreal M, Witt DM, Crowther M.
Thromboembolic events, recurrent bleeding and mortality after resuming anti-
coagulant following gastrointestinal bleeding. A meta-analysis. Thromb Haemost
2015;114:819825.
ESC Guidelines 117

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1188. O’Dea D, Whetteckey J, Ting N. A prospective, randomized, open-label study
to evaluate two management strategies for gastrointestinal symptoms in
patients newly on treatment with dabigatran. Cardiol Ther 2016;5:187201.
1189. Lai HC, Chien WC, Chung CH, Lee WL, Wu TJ, Wang KY, Liu CN, Liu TJ.
Atrial fibrillation, liver disease, antithrombotics and risk of cerebrovascular
events: a population-based cohort study. Int J Cardiol 2016;223:829837.
1190. Lip GY, Frison L, Halperin JL, Lane DA. Comparative validation of a novel risk
score for predicting bleeding risk in anticoagulated patients with atrial fibrilla-
tion: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke,
Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol
Concomitantly) score. J Am Coll Cardiol 2011;57:173180.
1191. Potpara TS, Lip GY. Drug-induced liver injury with oral anticoagulants: a threat
or not?Heart 2017;103:809811.
1192. Hoolwerf EW, Kraaijpoel N, Buller HR, van Es N. Direct oral anticoagulants in
patients with liver cirrhosis: a systematic review. Thromb Res
2018;170:102108.
1193. Kubitza D, Roth A, Becka M, Alatrach A, Halabi A, Hinrichsen H, Mueck W.
Effect of hepatic impairment on the pharmacokinetics and pharmacodynamics
of a single dose of rivaroxaban, an oral, direct factor Xa inhibitor. Br J Clin
Pharmacol 2013;76:8998.
1194. Bonde AN, Blanche P, Staerk L, Gerds TA, Gundlund A, Gislason G, Torp-
Pedersen C, Lip GYH, Hlatky MA, Olesen JB. Oral anticoagulation among
atrial fibrillation patients with anaemia: an observational cohort study. Eur
Heart J 2019.
1195. Arun M, Brauneis D, Doros G, Shelton AC, Sloan JM, Quillen K, Ruberg FL,
Sanchorawala V, Varga C. The incidence of atrial fibrillation among patients
with AL amyloidosis undergoing high-dose melphalan and stem cell transplan-
tation: experience at a single institution. Bone Marrow Transplant
2017;52:13491351.
1196. Yuan M, Tse G, Zhang Z, Han X, Wu WKK, Li G, Xia Y, Liu T. The incidence
of atrial fibrillation with trastuzumab treatment: a systematic review and meta-
analysis. Cardiovasc Ther 2018;36:e12475.
1197. Ganatra S, Sharma A, Shah S, Chaudhry GM, Martin DT, Neilan TG,
Mahmood SS, Barac A, Groarke JD, Hayek SS, Dani S, Venesy D, Patten R,
Nohria A. Ibrutinib-associated atrial fibrillation. JACC Clin Electrophysiol
2018;4:14911500.
1198. Boriani G, Corradini P, Cuneo A, Falanga A, Foa R, Gaidano G, Ghia PP,
Martelli M, Marasca R, Massaia M, Mauro FR, Minotti G, Molica S, Montillo M,
Pinto A, Tedeschi A, Vitolo U, Zinzani PL. Practical management of ibrutinib in
the real life: focus on atrial fibrillation and bleeding. Hematol Oncol
2018;36:624632.
1199. Yun S, Vincelette ND, Acharya U, Abraham I. Risk of atrial fibrillation and
bleeding diathesis associated with ibrutinib treatment: a systematic review and
pooled analysis of four randomized controlled trials. Clin Lymphoma Myeloma
Leuk 2017;17:3137.e13.
1200. Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age
distribution, and gender of patients with atrial fibrillation. Analysis and implica-
tions. Arch Intern Med 1995;155:469473.
1201. Lane DA, Skjoth F, Lip GYH, Larsen TB, Kotecha D. Temporal trends in inci-
dence, prevalence, and mortality of atrial fibrillation in primary care. JAm
Heart Assoc 2017;6:e005155.
1202. Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward
JB, Tsang TS. Secular trends in incidence of atrial fibrillation in Olmsted
County, Minnesota, 1980 to 2000,and implication s on the projections for future
prevalence. Circulation 2006;114:119125.
1203. Ohlmeier C, Mikolajczyk R, Haverkamp W, Garbe E. Incidence, prevalence,
and antithrombotic management of atrial fibrillation in elderly Germans.
Europace 2013;15:14361444.
1204. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE.
Prevalence of diagnosed atrial fibrillation in adults: national implications for
rhythm management and stroke prevention: the AnTicoagulation and Risk
Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:23702375.
1205. Wilke T, Groth A, Mueller S, Pfannkuche M, Verheyen F, Linder R, Maywald
U, Bauersachs R, Breithardt G. Incidence and prevalence of atrial fibrillation:
an analysis based on 8.3 million patients. Europace 2013;15:486493.
1206. Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial
fibrillation: European perspective. Clin Epidemiol 2014;6:213220.
1207. Marinigh R, Lip GY, Fiotti N, Giansante C, Lane DA. Age as a risk factor for
stroke in atrial fibrillation patients: implications for thromboprophylaxis. JAm
Coll Cardiol 2010;56:827837.
1208. Stroke Risk in Atrial Fibrillation Working Group. Independent predictors of
stroke in patients with atrial fibrillation: a systematic review. Neurology
2007;69:546554.
1209. Graham DJ, Reichman ME, Wernecke M, Zhang R, Southworth MR, Levenson
M, Sheu TC, Mott K, Goulding MR, Houstoun M, MaCurdy TE, Worrall C,
Kelman JA. Cardiovascular, bleeding, and mortality risks in elderly Medicare
patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation.
Circulation 2015;131:157164.
1210. Biteker M, Basaran O, Dogan V, Altun I, Ozpamuk Karadeniz F, Tekkesin AI,
Cakilli Y, Turkkan C, Hamidi M, Demir V, Gursoy MO, Tek Ozturk M, Aksan
G, Seyis S, Balli M, Alici MH, Bozyel S. Real-world clinical characteristics and
treatment patterns of individuals aged 80 and older with nonvalvular atrial
fibrillation: results from the ReAl-life Multicenter Survey Evaluating Stroke
Study. J Am Geriatr Soc 2017;65:16841690.
1211. Gage BF, Boechler M, Doggette AL, Fortune G, Flaker GC, Rich MW, Radford
MJ. Adverse outcomes and predictors of underuse of antithrombotic therapy
in Medicare beneficiaries with chronic atrial fibrillation. Stroke
2000;31:822827.
1212. Ghaswalla PK, Harpe SE, Slattum PW. Warfarin use in nursing home residents:
results from the 2004 national nursing home survey. Am J Geriatr Pharmacother
2012;10:2536.e2.
1213. Kotecha D, Chudasama R, Lane DA, Kirchhof P, Lip GY. Atrial fibrillation and
heart failure due to reduced versus preserved ejection fraction: a systematic
review and meta-analysis of death and adverse outcomes. Int J Cardiol
2016;203:660666.
1214. Oqab Z, Pournazari P, Sheldon RS. What is the impact of frailty on prescrip-
tion of anticoagulation in elderly patients with atrial fibrillation? A systematic
review and meta-analysis. J Atr Fibrillation 2018;10:1870.
1215. Proietti M, Laroche C, Opolski G, Maggioni AP, Boriani G, Lip GYH, on behalf
of the AF Gen Pilot Investigators. ‘Real-world’ atrial fibrillation management in
Europe: observations from the 2-year follow-up of the EURObservational
Research Programme-Atrial Fibrillation General Registry Pilot Phase. Europace
2017;19:722733.
1216. Singh P, Arrevad PS, Peterson GM, Bereznicki LR. Evaluation of antithrombotic
usage for atrial fibrillation in aged care facilities. J Clin Pharm Ther
2011;36:166171.
1217. Annoni G, Mazzola P. Real-world characteristics of hospitalized frail elderly
patients with atrial fibrillation: can we improve the current prescription of
anticoagulants?J Geriatr Cardiol 2016;13:226232.
1218. Deandrea S, Bravi F, Turati F, Lucenteforte E, La Vecchia C, Negri E. Risk fac-
tors for falls in older people in nursing homes and hospitals. A systematic
review and meta-analysis. Arch Gerontol Geriatr 2013;56:407415.
1219. Phelan EA, Mahoney JE, Voit JC, Stevens JA. Assessment and management of
fall risk in primary care settings. Med Clin North Am 2015;99:281293.
1220. Donze J, Clair C, Hug B, Rodondi N, Waeber G, Cornuz J, Aujesky D. Risk of
falls and major bleeds in patients on oral anticoagulation therapy. Am J Med
2012;125:773778.
1221. Garwood CL, Corbett TL. Use of anticoagulation in elderly patients
with atrial fibrillation who are at risk for falls. Ann Pharmacother 2008;42:
523532.
1222. Hart RG, Pearce LA, Aguilar MI. Adjusted-dose warfarin versus aspirin for pre-
venting stroke in patients with atrial fibrillation. Ann Intern Med
2007;147:590592.
1223. Jacobs LG, Billett HH, Freeman K, Dinglas C, Jumaquio L. Anticoagulation for
stroke prevention in elderly patients with atrial fibrillation, including those
with falls and/or early-stage dementia: a single-center, retrospective, observa-
tional study. Am J Geriatr Pharmacother 2009;7:159166.
1224. Rash A, Downes T, Portner R, Yeo WW, Morgan N, Channer KS. A rando-
mised controlled trial of warfarin versus aspirin for stroke prevention in
octogenarians with atrial fibrillation (WASPO). Age A ge ing
2007;
36:151156.
1225. Sardar P, Chatterjee S, Chaudhari S, Lip GY. New oral anticoagulants in eld-
erly adults: evidence from a meta-analysis of randomized trials. J Am Geriatr Soc
2014;62:857864.
1226. Siu CW, Tse HF. Net clinical benefit of warfarin therapy in elderly Chinese
patients with atrial fibrillation. Circ Arrhythm Electrophysiol 2014;7:300306.
1227. Alnsasra H, Haim M, Senderey AB, Reges O, Leventer-Roberts M, Arnson Y,
Leibowitz M, Hoshen M, Avgil-Tsadok M. Net clinical benefit of anticoagulant
treatments in elderly patients with nonvalvular atrial fibrillation: experience
from the real world. Heart Rhythm 2019;16:3137.
1228. Eikelboom JW, Wallentin L, Connolly SJ, Ezekowitz M, Healey JS, Oldgren J,
Yang S, Alings M, Kaatz S, Hohnloser SH, Diener HC, Franzosi MG, Huber K,
Reilly P, Varrone J, Yusuf S. Risk of bleeding with 2 doses of dabigatran com-
pared with warfarin in older and younger patients with atrial fibrillation: an
analysis of the randomized evaluation of long-term anticoagulant therapy (RE-
LY) trial. Circulation 2011;123:23632372.
1229. Halperin JL, Hankey GJ, Wojdyla DM, Piccini JP, Lokhnygina Y, Patel MR,
Breithardt G, Singer DE, Becker RC, Hacke W, Paolini JF, Nessel CC,
Mahaffey KW, Califf RM, Fox KA; ROCKET AF Steering Committee
Investigators. Efficacy and safety of rivaroxaban compared with warfarin
among elderly patients with nonvalvular atrial fibrillation in the Rivaroxaban
Once Daily, Oral, Direct Factor Xa Inhibition Compared With Vitamin K
118 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation
(ROCKET AF). Circulation 2014;130:138146.
1230. Halvorsen S, Atar D, Yang H, De Caterina R, Erol C, Garcia D, Granger CB,
Hanna M, Held C, Husted S, Hylek EM, Jansky P, Lopes RD, Ruzyllo W,
Thomas L, Wallentin L. Efficacy and safety of apixaban compared with warfarin
according to age for stroke prevention in atrial fibrillation: observations from
the ARISTOTLE trial. Eur Heart J 2014;35:18641872.
1231. Hori M, Matsumoto M, Tanahashi N, Momomura S, Uchiyama S, Goto S,
Izumi T, Koretsune Y, Kajikawa M, Kato M, Ueda H, Iekushi K, Yamanaka S,
Tajiri M; J-ROCKET AF Study Investigators. Rivaroxaban vs. warfarin in
Japanese patients with non-valvular atrial fibrillation in relation to age. Circ J
2014;78:13491356.
1232. Kato ET, Giugliano RP, Ruff CT, Koretsune Y, Yamashita T, Kiss RG, Nordio F,
Murphy SA, Kimura T, Jin J, Lanz H, Mercuri M, Braunwald E, Antman, EM.
Efficacy and safety of edoxaban in elderly patients with atrial fibrillation in the
ENGAGE AF-TIMI 48 trial. J Am Heart Assoc 2016;5:e003432.
1233. Kim IS, Kim HJ, Kim TH, Uhm JS, Joung B, Lee MH, Pak HN. Non-vitamin K
antagonist oral anticoagulants have better efficacy and equivalent safety com-
pared to warfarin in elderly patients with atrial fibrillation: a systematic review
and meta-analysis. J Cardiol 2018;72:105112.
1234. Ng KH, Shestakovska O, Connolly SJ, Eikelboom JW, Avezum A, Diaz R, Lanas
F, Yusuf S, Hart RG. Efficacy and safety of apixaban compared with aspirin in
the elderly: a subgroup analysis from the AVERROES trial. Age Ageing
2016;45:7783.
1235. Ruiz Ortiz M, Muniz J, Rana Miguez P, Roldan I, Marin F, Asuncion Esteve-
Pastor M Cequier A, Martinez-Selles M, Bertomeu V, Anguita M; FANTASIIA
Study Investigators. Inappropriate doses of direct oral anticoagulants in real-
world clinical practice: prevalence and associated factors. A subanalysis of the
FANTASIIA Registry. Europace 2018;20:15771583.
1236. Deitelzweig S, Keshishian A, Li X, Kang A, Dhamane AD, Luo X, Balachander
N, Rosenblatt L, Mardekian J, Pan X, Nadkarni A, Di Fusco M, Garcia Reeves
AB, Yuce H, Lip GYH. Comparisons between oral anticoagulants among older
nonvalvular atrial fibrillation patients. J Am Geriatr Soc 2019;67:16621671.
1237. Dillinger JG, Aleil B, Cheggour S, Benhamou Y, Bejot Y, Marechaux S, Delluc
A, Bertoletti L, Lellouche N. Dosing issues with non-vitamin K antagonist oral
anticoagulants for the treatment of non-valvular atrial fibrillation: why we
should not underdose our patients. Arch Cardiovasc Dis 2018;111:8594.
1238. Nieuwlaat R, Olsson SB, Lip GY, Camm AJ, Breithardt G, Capucci A, Meeder
JG, Prins MH, Levy S, Crijns HJ; Euro Heart Survey Investigators. Guideline-
adherent antithrombotic treatment is associated with improved outcomes
compared with undertreatment in high-risk patients with atrial fibrillation. The
Euro Heart Survey on Atrial Fibrillation. Am Heart J 2007;153:10061012.
1239. Fumagalli S, Said SAM, Laroche C, Gabbai D, Marchionni N, Boriani G,
Maggioni AP, Popescu MI, Rasmussen LH, Crijns H, Lip GYH; EORP-AF
Investigators. Age-related differences in presentation, treatment, and outcome
of patients with atrial fibrillation in europe: the EORP-AF General Pilot
Registry (EURObservational Research Programme-Atrial Fibrillation). JACC Clin
Electrophysiol 2015;1:326
334.
1240. Paciullo F, Proietti M, Bianconi V, Nobili A, Pirro M, Mannucci PM, Lip GYH,
Lupattelli G; REPOSI Investigators. Choice and outcomes of rate control ver-
sus rhythm control in elderly patients with atrial fibrillation: a report from the
REPOSI Study. Drugs Aging 2018;35:365373.
1241. Shariff N, Desai RV, Patel K, Ahmed MI, Fonarow GC, Rich MW, Aban IB,
Banach M, Love TE, White M, Aronow WS, Epstein AE, Ahmed A. Rate-con-
trol versus rhythm-control strategies and outcomes in septuagenarians with
atrial fibrillation. Am J Med 2013;126:887893.
1242. Purmah Y, Proietti M, Laroche C, Mazurek M, Tahmatzidis D, Boriani G, Novo
S, Lip GYH; EORP-AF General Pilot Registry Investigators. Rate vs. rhythm
control and adverse outcomes among European patients with atrial fibrillation.
Europace 2018;20:243252.
1243. Abdin A, Yalin K, Lyan E, Sawan N, Liosis S, Meyer-Saraei R, Elsner C, Lange
SA, Heeger CH, Eitel C, Eitel I, Tilz RR. Safety and efficacy of cryoballoon abla-
tion for the treatment of atrial fibrillation in elderly patients. Clin Res Cardiol
2019;108:167174.
1244. Bhargava M, Marrouche NF, Martin DO, Schweikert RA, Saliba W, Saad EB,
Bash D, Williams-Andrews M, Rossillo A, Erciyes D, Khaykin Y, Burkhardt JD,
Joseph G, Tchou PJ, Natale A. Impact of age on the outcome of pulmonary
vein isolation for atrial fibrillation using circular mapping technique and
cooled-tip ablation catheter. J Cardiovasc Electrophysiol 2004;15:813.
1245. Bulava A, Hanis J, Dusek L. Clinical outcomes of radiofrequency catheter abla-
tion of atrial fibrillation in octogenarians-10-year experience of a one high-
volume center. J Geriatr Cardiol 2017;14:575581.
1246. Bunch TJ, Weiss JP, Crandall BG, May HT, Bair TL, Osborn JS, Anderson JL,
Lappe DL, Muhlestein JB, Nelson J, Day JD. Long-term clinical efficacy and risk
of catheter ablation for atrial fibrillation in octogenarians. Pacing Clin
Electrophysiol 2010;33:146152.
1247. Heeger CH, Bellmann B, Fink T, Bohnen JE, Wissner E, Wohlmuth P, Rottner
L, Sohns C, Tilz RR, Mathew S, Reissmann B, Lemes C, Maurer T, Luker J,
Sultan A, Plenge T, Goldmann B, Ouyang F, Kuck KH, Metzner I, Metzner A,
Steven D, Rillig A. Efficacy and safety of cryoballoon ablation in the elderly: a
multicenter study. Int J Cardiol 2019;278:108113.
1248. Kis Z, Noten AM, Martirosyan M, Hendriks AA, Bhagwandien R, Szili-Torok T.
Comparison of long-term outcome between patients aged <65 years vs. >/
=65 years after atrial fibrillation ablation. J Geriatr Cardiol 2017;14:569574.
1249. Lim T, Day D, Weiss P, Crandall BG, May HAT, Bair TL, Osborn JS, Anderson
JL, Muhlestein JB, Lappe DL, Mahapatra S, Bunch TJ. More aggressive left atrial
ablation in elderly patients does not increase procedural complications. J Innov
Card Rhythm Manag 2011;2:206211.
1250. Lin T, Du X, Bai R, Chen YW, Yu RH, Long DY, Tang RB, Sang CH, Li SN, Ma
CS, Dong JZ. Long-term results of single-procedure catheter ablation for atrial
fibrillationin pre- and post-menopausal women. J Geriatr Cardiol
2014;11:120125.
1251. Lioni L, Letsas KP, Efremidis M, Vlachos K, Giannopoulos G, Kareliotis V,
Deftereos S, Sideris A. Catheter ablation of atrial fibrillation in the elderly.
J
Geriatr Cardiol 2014;11:291295.
1252. Metzner I, Wissner E, Tilz RR, Rillig A, Mathew S, Schmidt B, Chun J,
Wohlmuth P, Deiss S, Lemes C, Maurer T, Fink T, Heeger C, Ouyang F, Kuck
KH, Metzner A. Ablation of atrial fibrillation in patients >/=75 years: long-
term clinical outcome and safety. Europace 2016;18:543549.
1253. Santangeli P, Di Biase L, Mohanty P, Burkhardt JD, Horton R, Bai R, Mohanty
S, Pump A, Gibson D, Couts L, Hongo R, Beheiry S, Natale A. Catheter abla-
tion of atrial fibrillation in octogenarians: safety and outcomes. J Cardiovasc
Electrophysiol 2012;23:687693.
1254. Tan HW, Wang XH, Shi HF, Yang GS, Zhou L, Gu JN, Jiang WF, Liu X.
Efficacy, safety and outcome of catheter ablation for atrial fibrillation in octo-
genarians. Int J Cardiol 2010;145:147148.
1255. Zado E, Callans DJ, Riley M, Hutchinson M, Garcia F, Bala R, Lin D, Cooper J,
Verdino R, Russo AM, Dixit S, Gerstenfeld E, Marchlinski FE. Long-term clini-
cal efficacy and risk of catheter ablation for atrial fibrillation in the elderly. J
Cardiovasc Electrophysiol 2008;19:621626.
1256. Abugattas JP, Iacopino S, Moran D, De Regibus V, Takarada K, Mugnai G,
Stroker E, Coutino-Moreno HE, Choudhury R, Storti C, De Greef Y, Paparella
G, Brugada P, de Asmundis C, Chierchia GB. Efficacy and safety of the second
generation cryoballoon ablation for the treatment of paroxysmal atrial fibrilla-
tion in patients over 75 years: a comparison with a younger cohort. Europace
2017;19:17981803.
1257. Bunch TJ, May HT, Bair TL, Jacobs V, Crandall BG, Cutler M, Weiss JP,
Mallender C, Osborn JS, Anderson JL, Day JD. The impact of age on 5-year
outcomes after atrial fibrillation catheter ablation. J Cardiovasc Electrophysiol
2016;27:141146.
1258. Guiot A, Jongnarangsin K, Chugh A, Suwanagool A, Latchamsetty R, Myles JD,
Jiang Q, Crawford T, Good E, Pelosi F Jr, Bogun F, Morady F, Oral H.
Anticoagulant therapy and risk of cerebrovascular events after catheter abla-
tion of atrial fibrillation in the elderly. J Cardiovasc Electrophysiol
2012;23:3643.
1259. Kusumoto F, Prussak K, Wiesinger M, Pullen T, Lynady C. Radiofrequency
catheter ablation of atrial fibrillation in older patients: outcomes and complica-
tions. J Interv Card Electrophysiol 2009;25:3135.
1260. Liu Y, Huang H, Huang C, Zhang S, Ma C, Liu X, Yang Y, Cao K, Wu S, Wang
F; National Atrial Fibrillation Working Group of Chinese Society of Pacing and
Electrophysiology. Catheter ablation of atrial fibrillation in Chinese elderly
patients. Int J Cardiol 2011;152:266267.
1261. Shah RU, Freeman JV, Shilane D, Wang PJ, Go AS, Hlatky MA. Procedural
complications, rehospitalizations, and repeat procedures after catheter abla-
tion for atrial fibrillation. J Am Coll Cardiol 2012;59:143149.
1262. Spragg DD, Dalal D, Cheema A, Scherr D, Chilukuri K, Cheng A, Henrikson
CA, Marine JE, Berger RD, Dong J, Calkins H. Complications of catheter abla-
tion for atrial fibrillation: incidence and predictors. J Cardiovasc Electrophysiol
2008;19:627631.
1263. Srivatsa UN, Danielsen B, Anderson I, Amsterdam E, Pezeshkian N, Yang Y,
White RH. Risk predictors of stroke and mortality after ablation for atrial
fibrillation: the California experience 20052009. Heart Rhythm
2014;11:18981903.
1264. Friberg L, Rosenqvist M. Less dementia with oral anticoagulation in atrial fibril-
lation. Eur Heart J 2018;39:453460.
1265. Jacobs V, Woller SC, Stevens S, May HT, Bair TL, Anderson JL, Crandall BG,
Day JD, Johanning K, Long Y, Mallender C, Olson JL, Osborn JS, Weiss JP,
Bunch TJ. Time outside of therapeutic range in atrial fibrillation patients is
associated with long-term risk of dementia. Heart Rhythm
2014;11:22062213.
1266. Jacobs V, Woller SC, Stevens SM, May HT, Bair TL, Crandall BG, Cutler M,
Day JD, Weiss JP, Osborn JS, Mallender C, Anderson JL, Bunch TJ. Percent
ESC Guidelines 119

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
time with a supratherapeutic INR in atrial fibrillation patients also using an
antiplatelet agent is associated with long-term risk of dementia. J Cardiovasc
Electrophysiol 2015;26:11801186.
1267. Jacobs V, May HT, Bair TL, Crandall BG, Cutler MJ, Day JD, Mallender C,
Osborn JS, Stevens SM, Weiss JP, Woller SC, Bunch TJ. Long-term
population-based cerebral ischemic event and cognitive outcomes of direct
oral anticoagulants compared with warfarin among long-term anticoagulated
patients for atrial fibrillation. Am J Cardiol 2016;118:210214.
1268. Zhang C, Gu ZC, Shen L, Pan MM, Yan YD, Pu J, Liu XY, Lin HW. Non-vita-
min K antagonist oral anticoagulants and cognitive impairment in atrial fibrilla-
tion: insights from the meta-analysis of over 90,000 patients of randomized
controlled trials and real-world studies. Front Aging Neurosci 2018;10:258.
1269. Sogaard M, Skjoth F, Jensen M, Kjaeldgaard JN, Lip GYH, Larsen TB, Nielsen
PB. Nonvitamin K antagonist oral anticoagulants versus warfarin in atrial fibril-
lation patients and risk of dementia: a nationwide propensity-weighted cohort
study. J Am Heart Assoc 2019;8:e011358.
1270. Friberg L, Andersson T, Rosenqvist M. Less dementia and stroke in low-risk
patients with atrial fibrillation taking oral anticoagulation. Eur Heart J
2019;40:23272335.
121. Okuno J, Yanagi H, Tomura S. Is cognitive impairment a risk factor for poor
compliance among Japanese elderly in the community?Eur J Clin Pharmacol
2001;57:589594.
1272. Salas M, In’t Veld BA, van der Linden PD, Hofman A, Breteler M, Stricker
BH. Impaired cognitive function and compliance with antihypertensive
drugs in elderly: the Rotterdam Study. Clin Pharm acol Ther
2001;70:561566.
1273. Jensen AS, Idorn L, Norager B, Vejlstrup N, Sondergaard L. Anticoagulation in
adults with congenital heart disease: the who, the when and the how?Heart
2015;101:424429.
1274. Renda G, Ricci F, Giugliano RP, De Caterina R. Non-vitamin K antagonist oral
anticoagulants in patients with atrial fibrillation and valvular heart disease. JAm
Coll Cardiol 2017;69:13631371.
1275. Caldeira D, David C, Costa J, Ferreira JJ, Pinto FJ. Non-vitamin K antagonist
oral anticoagulants in patients with atrial fibrillation and valvular heart disease:
systematic review and meta-analysis. Eur Heart J Cardiovasc Pharm acother
2018;4:111118.
1276. Ammash NM, Phillips SD, Hodge DO, Connolly HM, Grogan MA, Friedman
PA, Warnes CA, Asirvatham SJ. Outcome of direct current cardioversion for
atrial arrhythmias in adults with congenital heart disease. Int J Cardiol
2012;154:270274.
1277. Feltes TF, Friedman RA. Transesophageal echocardiographic detection of atrial
thrombi in patients with nonfibrillation atrial tachyarrhythmias and congenital
heart disease. J Am Coll Cardiol 1994;24:13651370.
1278. Roos-Hesselink J, Meijboom F, Spitaels S, van Domburg R, van Rijen E, Utens
E, Bogers A, Simoons M, Simoons ML. Excellent survival and low incidence of
arrhythmias, stroke and heart failure long-term after surgical ASD closure at
young age. A prospective follow-up study of 2133 years. Eur Heart J
2003;24:190197.
1279. Mas JL, Derumeaux G, Guillon B, Massardier E, Hosseini H, Mechtouff L,
Arquizan C, Bejot Y, Vuillier F, Detante O, Guidoux C, Canaple S, Vaduva C,
Dequatre-Ponchelle N, Sibon I, Garnier P, Ferrier A, Timsit S, Robinet-
Borgomano E, Sablot D, Lacour JC, Zuber M, Favrole P, Pinel JF, Apoil M,
Reiner P, Lefebvre C, Guerin P, Piot C, Rossi R, Dubois-Rande JL, Eicher JC,
Meneveau N, Lusson JR, Bertrand B, Schleich JM, Godart F, Thambo JB,
Leborgne L, Michel P, Pierard L, Turc G, Barthelet M, Charles-Nelson A,
Weimar C, Moulin T, Juliard JM, Chatellier G; CLOSE Investigators. Patent
foramen ovale closure or anticoagulation vs. antiplatelets after stroke. NEnglJ
Med 2017;377:10111021.
1280. Gutierrez SD, Earing MG, Singh AK, Tweddell JS, Bartz PJ. Atrial tachyarrhyth-
mias and the Cox-maze procedure in congenital heart disease. Congenit Heart
Dis 2013;8:434439.
1281. Kobayashi J, Yamamoto F, Nakano K, Sasako Y, Kitamura S, Kosakai Y. Maze
procedure for atrial fibrillation associated with atrial septal defect. Circulation
1998;98:II399402.
1282. Shim H, Yang JH, Park PW, Jeong DS, Jun TG. Efficacy of the maze procedure
for atrial fibrillation associated with atrial septal defect. Korean J Thorac
Cardiovasc Surg 2013;46:98103.
1283. Sherwin ED, Triedman JK, Walsh EP. Update on interventional electrophysiol-
ogy in congenital heart disease: evolving solutions for complex hearts. Circ
Arrhythm Electrophysiol 2013;6:10321040.
1284. Johnson JN, Tester DJ, Perry J, Salisbury BA, Reed CR, Ackerman MJ.
Prevalence of early-onset atrial fibrillation in congenital long QT syndrome.
Heart Rhythm 2008;5:704709.
1285. Zellerhoff S, Pistulli R, Monnig G, Hinterseer M, Beckmann BM, Kobe J,
Steinbeck G, Kaab S, Haverkamp W, Fabritz L, Gradaus R, Breithardt G,
Schulze-Bahr E, Bocker D, Kirchhof P. Atrial arrhythmias in long-QT syndrome
under daily life conditions: a nested case control study. J Cardiovasc
Electrophysiol 2009;20:401407.
1286. Gaita F, Giustetto C, Bianchi F, Wolpert C, Schimpf R, Riccardi R, Grossi S,
Richiardi E, Borggrefe M. Short QT syndrome: a familial cause of sudden death.
Circulation 2003;108:965970.
1287. Borggrefe M, Wolpert C, Antzelevitch C, Veltmann C, Giustetto C, Gaita F,
Schimpf R. Short QT syndrome. Genotype-phenotype correlations. J
Electrocardiol 2005;38:7580.
1288. Giustetto C, Di Monte F, Wolpert C, Borggrefe M, Schimpf R, Sbragia P,
Leone G, Maury P, Anttonen O, Haissaguerre M, Gaita F. Short QT syn-
drome: clinical findings and diagnostic-therapeutic implications. Eur Heart J
2006;27:24402447.
1289. Giustetto C, Schimpf R, Mazzanti A, Scrocco C, Maury P, Anttonen O, Probst
V, Blanc JJ, Sbragia P, Dalmasso P, Borggrefe M, Gaita F. Long-term follow-up
of patients with short QT syndrome. J Am Coll Cardiol 2011;58:587595.
1290. Gollob MH, Redpath CJ, Roberts JD. The short QT syndrome: proposed diag-
nostic criteria. J Am Coll Cardiol 2011;57:802812.
1291. Bordachar P, Reuter S, Garrigue S, Cai X, Hocini M, Jais P, Haissaguerre M,
Clementy J. Incidence, clinical implications and prognosis of atrial arrhythmias
in Brugada syndrome. Eur Heart J 2004;25:879884.
1292. Kusano KF, Taniyama M, Nakamura K, Miura D, Banba K, Nagase S, Morita H,
Nishii N, Watanabe A, Tada T, Murakami M, Miyaji K, Hiramatsu S, Nakagawa
K, Tanaka M, Miura A, Kimura H, Fuke S, Sumita W, Sakuragi S, Urakawa S,
Iwasaki J, Ohe T. Atrial fibrillation in patients with Brugada syndrome relation-
ships of gene mutation, electrophysiology, and clinical backgrounds. J Am Coll
Cardiol 2008;51:11691175.
1293. Francis J, Antzelevitch C. Atrial fibrillation and Brugada syndrome. J Am Coll
Cardiol 2008;51:11491153.
1294. Rodriguez-Manero M, Namdar M, Sarkozy A, Casado-Arroyo R, Ricciardi D,
de Asmundis C, Chierchia GB, Wauters K, Rao JY, Bayrak F, Van Malderen S,
Brugada P. Prevalence, clinical characteristics and management of atrial fibrilla-
tion in patients with Brugada syndrome. Am J Cardiol 2013;111:362367.
1295. Sacher F, Probst V, Maury P, Babuty D, Mansourati J, Komatsu Y, Marquie C,
Rosa A, Diallo A, Cassagneau R, Loizeau C, Martins R, Field ME, Derval N,
Miyazaki S, Denis A, Nogami A, Ritter P, Gourraud JB, Ploux S, Rollin A,
Zemmoura A, Lamaison D, Bordachar P, Pierre B, Jais P, Pasquie JL, Hocini M,
Legal F, Defaye P, Boveda S, Iesaka Y, Mabo P, Haissaguerre M. Outcome after
implantation of a cardioverter-defibrillator in patients with Brugada syndrome:
a multicenter study part 2. Circulation 2013;128:17391747.
1296. Hernandez-Ojeda J, Arbelo E, Borras R, Berne P, Tolosana JM, Gomez-
Juanatey A, Berruezo A, Campuzano O, Sarquella-Brugada G, Mont L, Brugada
R, Brugada J. Patients with Brugada syndrome and implanted cardioverter-
defibrillators: long-term follow-up. J Am Coll Cardiol 2017;70:19912002.
1297. Sumitomo N, Sakurada H, Taniguchi K, Matsumura M, Abe O, Miyashita M,
Kanamaru H, Karasawa K, Ayusawa M, Fukamizu S, Nagaoka I, Horie M,
Harada K, Hiraoka M. Association of atrial arrhythmia and sinus node dysfunc-
tion in patients with catecholaminergic polymorphic ventricular tachycardia.
Circ J 2007;71:16061609.
1298. Sy RW, Gollob MH, Klein GJ, Yee R, Skanes AC, Gula LJ, Leong-Sit P, Gow
RM, Green MS, Birnie DH, Krahn AD. Arrhythmia characterization and long-
term outcomes in catecholaminergic polymorphic ventricular tachycardia.
Heart Rhythm 2011;8:864871.
1299. Siontis KC, Geske JB, Ong K, Nishimura RA, Ommen SR, Gersh BJ. Atrial
fibrillation in hypertrophic cardiomyopathy: prevalence, clinical correlations,
and mortality in a large high-risk population. J Am Heart Assoc 2014;3:e001002.
1300. Guttmann OP, Rahman MS, O’Mahony C, Anastasakis A, Elliott PM. Atrial
fibrillation and thromboembolism in patients with hypertrophic cardiomyop-
athy: systematic review. Heart 2014;100:465472.
1301. Rowin EJ, Hausvater A, Link MS, Abt P, Gionfriddo W, Wang W, Rastegar H,
Estes NAM, Maron MS, Maron BJ. Clinical profile and consequences of atrial
fibrillation in hypertrophic cardiomyopathy. Circulation 2017;136:24202436.
1302. Rowin EJ, Orfanos A, Estes NAM, Wang W, Link MS, Maron MS, Maron BJ.
Occurrence and natural history of clinically silent episodes of atrial fibrillation
in hypertrophic cardiomyopathy. Am J Cardiol 2017;119:18621865.
1303. van Velzen HG, Theuns DA, Yap SC, Michels M, Schinkel AF. Incidence of
device-detected atrial fibrillation and long-term outcomes in patients with
hypertrophic cardiomyopathy. Am J Cardiol 2017;119:100105.
1304. Klopotowski M, Kwapiszewska A, Kukula K, Jamiolkowski J, Dabrowski M,
Derejko P, Oreziak A, Baranowski R, Spiewak M, Marczak M, Klisiewicz A,
Szepietowska B, Chmielak Z, Witkowski A. Clinical and echocardiographic
parameters as risk factors for atrial fibrillation in patients with hypertrophic
cardiomyopathy. Clin Cardiol 2018;41:13361340.
1305. Choi YJ, Choi EK, Han KD, Jung JH, Park J, Lee E, Choe W, Lee SR, Cha MJ,
Lim WH, Oh S. Temporal trends of the prevalence and incidence of atrial
fibrillation and stroke among Asian patients with hypertrophic cardiomyop-
athy: a nationwide population-based study. Int J Cardiol 2018;273:130135.
120 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1306. Chu AF, Zado E, Marchlinski FE. Atrial arrhythmias in patients with arrhythmo-
genic right ventricular cardiomyopathy/dysplasia and ventricular tachycardia.
Am J Cardiol 2010;106:720722.
1307. Camm CF, James CA, Tichnell C, Murray B, Bhonsale A, te Riele AS, Judge
DP, Tandri H, Calkins H. Prevalence of atrial arrhythmias in arrhythmogenic
right ventricular dysplasia/cardiomyopathy. Heart Rhythm 2013;10:16611668.
1308. Saguner AM, Ganahl S, Kraus A, Baldinger SH, Medeiros-Domingo A, Saguner
AR, Mueller-Burri SA, Wolber T, Haegeli LM, Krasniqi N, Tanner FC, Steffel J,
Brunckhorst C, Duru F. Clinical role of atrial arrhythmias in patients with
arrhythmogenic right ventricular dysplasia. Circ J 2014;78:28542861.
1309. Bourfiss M, Te Riele AS, Mast TP, Cramer MJ, Van Der Heijden JF, Van Veen
TA, Loh P, Dooijes D, Hauer RN, Velthuis BK. Influence of genotype on struc-
tural atrial abnormalities and atrial fibrillation or flutter in arrhythmogenic right
ventricular dysplasia/cardiomyopathy. J Cardiovasc Electrophysiol
2016;27:14201428.
1310. Mussigbrodt A, Knopp H, Efimova E, Weber A, Bertagnolli L, Hilbert S, Kosiuk
J, Dinov B, Bode K, Kircher S, Dagres N, Richter S, Sommer P, Husser D,
Bollmann A, Hindricks G, Arya A. Supraventricular arrhythmias in patients
with arrhythmogenic right ventricular dysplasia/cardiomyopathy associate with
long-term outcome after catheter ablation of ventricular tachycardias.
Europace 2018;20:11821187.
1311. Tonet JL, Castro-Miranda R, Iwa T, Poulain F, Frank R, Fontaine GH.
Frequency of supraventricular tachyarrhythmias in arrhythmogenic right ven-
tricular dysplasia. Am J Cardiol 1991;67:1153.
1312. Hasselberg NE, Haland TF, Saberniak J, Brekke PH, Berge KE, Leren TP,
Edvardsen T, Haugaa KH. Lamin A/C cardiomyopathy: young onset, high pene-
trance, and frequent need for heart transplantation. Eur Heart J
2018;39:853860.
1313. van Rijsingen IA, Nannenberg EA, Arbustini E, Elliott PM, Mogensen J,
Hermans-van Ast JF, van der Kooi AJ, van Tintelen JP, van den Berg MP,
Grasso M, Serio A, Jenkins S, Rowland C, Richard P, Wilde AA, Perrot A,
Pankuweit S, Zwinderman AH, Charron P, Christiaans I, Pinto YM. Gender-
specific differences in major cardiac events and mortality in lamin A/C muta-
tion carriers. Eur J Heart Fail 2013;15:376384.
1314. Kumar S, Baldinger SH, Gandjbakhch E, Maury P, Sellal JM, Androulakis AF,
Waintraub X, Charron P, Rollin A, Richard P, Stevenson WG, Macintyre CJ,
Ho CY, Thompson T, Vohra JK, Kalman JM, Zeppenfeld K, Sacher F, Tedrow
UB, Lakdawala NK. Long-term arrhythmic and nonarrhythmic outcomes of
lamin A/C mutation carriers. J Am Coll Cardiol 2016;68:22992307.
1315. Pasotti M, Klersy C, Pilotto A, Marziliano N, Rapezzi C, Serio A, Mannarino S,
Gambarin F, Favalli V, Grasso M, Agozzino M, Campana C, Gavazzi A, Febo O,
Marini M, Landolina M, Mortara A, Piccolo G, Vigano M, Tavazzi L, Arbustini E.
Long-term outcome and risk stratification in dilated cardiolaminopathies. JAm
Coll Cardiol 2008;52:12501260.
1316. Stollberger C, Blazek G, Winkler-Dworak M, Finsterer J. Atrial fibrillation in
left ventricular noncompaction with and without neuromuscular disorders is
associated with a poor prognosis. Int J Cardiol 2009;133:4145.
1317. Aras D, Tufekcioglu O, Ergun K, Ozeke O, Yildiz A, Topaloglu S, Deveci B,
Sahin O, Kisacik HL, Korkmaz S. Clinical features of isolated ventricular
noncompaction in adults long-term clinical course, echocardiographic
properties, and predictors of left ventricular failure.
J Card Fail
2006;12:726733.
1318. Li S, Zhang C, Liu N, Bai H, Hou C, Wang J, Song L, Pu J. Genotype-positive
status is associated with poor prognoses in patients with left ventricular non-
compaction cardiomyopathy. J Am Heart Assoc 2018;7:e009910.
1319. Pappone C, Radinovic A, Manguso F, Vicedomini G, Sala S, Sacco FM, Ciconte
G, Saviano M, Ferrari M, Sommariva E, Sacchi S, Ciaccio C, Kallergis EM,
Santinelli V. New-onset atrial fibrillation as first clinical manifestation of latent
Brugada syndrome: prevalence and clinical significance. Eur Heart J
2009;30:29852992.
1320. Hong K, Bjerregaard P, Gussak I, Brugada R. Short QT syndrome and atrial
fibrillation caused by mutation in KCNH2. J Cardiovasc Electrophysiol
2005;16:394396.
1321. Peters S. Atrial arrhythmias in arrhythmogenic cardiomyopathy: at the begin-
ning or at the end of the disease story?Circ J 2015;79:446.
1322. Fatkin D, MacRae C, Sasaki T, Wolff MR, Porcu M, Frenneaux M, Atherton J,
Vidaillet HJ, Jr., Spudich S, De Girolami U, Seidman JG, Seidman C, Muntoni F,
Muehle G, Johnson W, McDonough B. Missense mutations in the rod domain
of the lamin A/C gene as causes of dilated cardiomyopathy and conduction-
system disease. N Engl J Med 1999;341:17151724.
1323. Olesen MS, Yuan L, Liang B, Holst AG, Nielsen N, Nielsen JB, Hedley PL,
Christiansen M, Olesen SP, Haunso S, Schmitt N, Jespersen T, Svendsen JH.
High prevalence of long QT syndrome-associated SCN5A variants in patients
with early-onset lone atrial fibrillation. Circ Cardiovasc Genet 2012;5:450459.
1324. Giustetto C, Cerrato N, Gribaudo E, Scrocco C, Castagno D, Richiardi E,
Giachino D, Bianchi F, Barbonaglia L, Ferraro A. Atrial fibrillation in a large
population with Brugada electrocardiographic pattern:
prevalence, management, and correlation with prognosis. Heart Rhythm
2014;11:259265.
1325. Conte G, Dewals W, Sieira J, de Asmundis C, Ciconte G, Chierchia GB, Di
Giovanni G, Baltogiannis G, Saitoh Y, Levinstein M, La Meir M, Wellens F,
Pappaert G, Brugada P. Drug-induced Brugada syndrome in children: clinical
features, device-based management, and long-term follow-up. J Am Coll Cardiol
2014;63:22722279.
1326. Lee SE, Park JK, Uhm JS, Kim JY, Pak HN, Lee MH, Joung B. Impact of atrial
fibrillation on the clinical course of apical hypertrophic cardiomyopathy. Heart
2017;103:14961501.
1327. Olivotto I, Cecchi F, Casey SA, Dolara A, Traverse JH, Maron BJ. Impact of
atrial fibrillation on the clinical course of hypertrophic cardiomyopathy.
Circulation 2001;104:25172524.
1328. Maron BJ, Olivotto I, Spirito P, Casey SA, Bellone P, Gohman TE, Graham KJ,
Burton DA, Cecchi F. Epidemiology of hypertrophic cardiomyopathy-related
death: revisited in a large non-referral-based patient population. Circulation
2000;102:858864.
1329. Mazzanti A, Ng K, Faragli A, Maragna R, Chiodaroli E, Orphanou N,
Monteforte N, Memmi M, Gambelli P, Novelli V, Bloise R, Catalano O, Moro
G, Tibollo V, Morini M, Bellazzi R, Napolitano C, Bagnardi V, Priori SG.
Arrhythmogenic right ventricular cardiomyopathy: clinical course and predic-
tors of arrhythmic risk.
J Am Coll Cardiol 2016;68:25402550.
1330. Pizzale S, Gollob MH, Gow R, Birnie DH. Sudden death in a young man with
catecholaminergic polymorphic ventricular tachycardia and paroxysmal atrial
fibrillation. J Cardiovasc Electrophysiol 2008;19:13191321.
1331. Roses-Noguer F, Jarman JW, Clague JR, Till J. Outcomes of defibrillator ther-
apy in catecholaminergic polymorphic ventricular tachycardia. Heart Rhythm
2014;11:5866.
1332. van der Werf C, Lieve KV, Bos JM, Lane CM, Denjoy I, Roses-Noguer F, Aiba
T, Wada Y, Ingles J, Leren IS, Rudic B, Schwartz PJ, Maltret A, Sacher F,
Skinner JR, Krahn AD, Roston TM, Tfelt-Hansen J, Swan H, Robyns T, Ohno S,
Roberts JD, van den Berg MP, Kammeraad JA, Probst V, Kannankeril PJ, Blom
NA, Behr ER, Borggrefe M, Haugaa KH, Semsarian C, Horie M, Shimizu W, Till
JA, Leenhardt A, Ackerman MJ, Wilde AA. Implantable cardioverter-
defibrillators in previously undiagnosed patients with catecholaminergic poly-
morphic ventricular tachycardia resuscitated from sudden cardiac arrest. Eur
Heart J 2019;40:29532961.
1333. Sugiyasu A, Oginosawa Y, Nogami A, Hata Y. A case with catecholaminergic
polymorphic ventricular tachycardia unmasked after successful ablation of
atrial tachycardias from pulmonary veins. Pacing Clin Electrophysiol
2009;32:e2124.
1334. Veltmann C, Kuschyk J, Schimpf R, Streitner F, Schoene N, Borggrefe M,
Wolpert C. Prevention of inappropriate ICD shocks in patients with Brugada
syndrome. Clin Res Cardiol 2010;99:3744.
1335. Klein GJ, Bashore TM, Sellers TD, Pritchett EL, Smith WM, Gallagher JJ.
Ventricular fibrillation in the Wolff-Parkinson-White syndrome. N Engl J Med
1979;301:10801085.
1336. Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomstrom-Lundqvist C,
Calkins H, Corrado D, Deftereos SG, Diller GP, Gomez-Doblas JJ, Gorenek B,
Grace A, Ho SY, Kaski JC, Kuck KH, Lambiase PD, Sacher F, Sarquella-Brugada
G, Suwalski P, Zaza A; ESC Scientific Document Group. 2019 ESC Guidelines
for the management of patients with supraventricular tachycardia. The Task
Force for the management of patients with supraventricular tachycardia of the
European Society of Cardiology (ESC). Eur Heart J 2020;41:655720.
1337. Morady F, DiCarlo LA, Jr., Baerman JM, De Buitleir M. Effect of propranolol
on ventricular rate during atrial fibrillation in the Wolff-Parkinson-White syn-
drome. Pacing Clin Electrophysiol 1987;10:492496.
1338. Sellers TD Jr, Bashore TM, Gallagher JJ. Digitalis in the pre-excitation syn-
drome. Analysis during atrial fibrillation. Circulation 1977;56:260267.
1339. Glatter KA, Dorostkar PC, Yang Y, Lee RJ, Van Hare GF, Keung E, Modin G,
Scheinman MM. Electrophysiological effects of ibutilide in patients with acces-
sory pathways. Circulation 2001;104:19331939.
1340. Ludmer PL, McGowan NE, Antman EM, Friedman PL. Efficacy of propafenone
in Wolff-Parkinson-White syndrome: electrophysiologic findings and long-
term follow-up. J Am Coll Cardiol 1987;9:13571363.
1341. Boahene KA, Klein GJ, Yee R, Sharma AD, Fujimura O. Termination of acute
atrial fibrillation in the Wolff-Parkinson-White syndrome by procainamide and
propafenone: importance of atrial fibrillatory cycle length. J Am Coll Cardiol
1990;16:14081414.
1342. Crijns HJ, den Heijer P, van Wijk LM, Lie KI. Successful use of flecainide in
atrial fibrillation with rapid ventricular rate in the Wolff-Parkinson-White syn-
drome. Am Heart J 1988;115:13171321.
1343. Simonian SM, Lotfipour S, Wall C, Langdorf MI. Challenging the superiority of
amiodarone for rate control in Wolff-Parkinson-White and atrial fibrillation.
Intern Emerg Med 2010;5:421426.
ESC Guidelines 121

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1344. Vaidya VR, Arora S, Patel N, Badheka AO, Patel N, Agnihotri K, Billimoria Z,
Turakhia MP, Friedman PA, Madhavan M, Kapa S, Noseworthy PA, Cha YM,
Gersh B, Asirvatham SJ, Deshmukh AJ. Burden of arrhythmia in pregnancy.
Circulation 2017;135:619621.
1345. Drenthen W, Pieper PG, Roos-Hesselink JW, van Lottum WA, Voors AA,
Mulder BJ, van Dijk AP, Vliegen HW, Yap SC, Moons P, Ebels T, van
Veldhuisen DJ; Zahara Investigators. Outcome of pregnancy in women with
congenital heart disease: a literature review. J Am Coll Cardiol
2007;49:23032311.
1346. Opotowsky AR, Siddiqi OK, D’Souza B, Webb GD, Fernandes SM, Landzberg
MJ. Maternal cardiovascular events during childbirth among women with con-
genital heart disease. Heart 2012;98:145151.
1347. Lee MS, Chen W, Zhang Z, Duan L, Ng A, Spencer HT, Kwan DM, Shen AY.
Atrial fibrillation and atrial flutter in pregnant women a population-based
study. J Am Heart Assoc 2016;5:e003182.
1348. Li JM, Nguyen C, Joglar JA, Hamdan MH, Page RL. Frequency and outcome of
arrhythmias complicating admission during pregnancy: experience from a
high-volume and ethnically-diverse obstetric service. Clin Cardiol
2008;31:538541.
1349. Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomstrom-Lundqvist C,
Cifkova R, De Bonis M, Iung B, Johnson MR, Kintscher U, Kranke P, Lang IM,
Morais J, Pieper PG, Presbitero P, Price S, Rosano GMC, Seeland U, Simoncini
T, Swan L, Warnes CA; ESC Scientific Document Group. 2018 ESC
Guidelines for the management of cardiovascular diseases during pregnancy.
Eur Heart J 2018;39:31653241.
1350. Wang YC, Chen CH, Su HY, Yu MH. The impact of maternal cardioversion
on fetal haemodynamics. Eur J Obstet Gynecol Reprod Biol 2006;126:268269.
1351. Moore JS, Teefey P, Rao K, Berlowitz MS, Chae SH, Yankowitz J. Maternal
arrhythmia: a case report and review of the literature. Obstet Gynecol Surv
2012;67:298312.
1352. Page RL. Treatment of arrhythmias during pregnancy. Am Heart J
1995;130:871876.
1353. Barnes EJ, Eben F, Patterson D. Direct current cardioversion during pregnancy
should be performed with facilities available for fetal monitoring and emer-
gency caesarean section. BJOG 2002;109:14061407.
1354. Katritsis DG, Boriani G, Cosio FG, Hindricks G, Jais P, Josephson ME, Keegan
R, Kim YH, Knight BP, Kuck KH, Lane DA, Lip GYH, Malmborg H, Oral H,
Pappone C, Themistoclakis S, Wood KA, Blomstrom-Lundqvist C. European
Heart Rhythm Association (EHRA) consensus document on the management
of supraventricular arrhythmias, endorsed by Heart Rhythm Society (HRS),
Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de
Estimulacion Cardiaca y Electrofisiologia (SOLAECE). Eur Heart J
2018;39:14421445.
1355. Kockova R, Kocka V, Kiernan T, Fahy GJ. Ibutilide-induced cardioversion of
atrial fibrillation during pregnancy. J Cardiovasc Electrophysiol 2007;18:545547.
1356. Lip GY, Beevers M, Churchill D, Shaffer LM, Beevers DG. Effect of atenolol on
birth weight. Am J Cardiol
1997;79:14361438.
1357. Heidbuchel H, Anne W, Willems R, Adriaenssens B, Van de Werf F, Ector H.
Endurance sports is a risk factor for atrial fibrillation after ablation for atrial
flutter. Int J Cardiol 2006;107:6772.
1358. Calvo N, Ramos P, Montserrat S, Guasch E, Coll-Vinent B, Domenech M,
Bisbal F, Hevia S, Vidorreta S, Borras R, Falces C, Embid C, Montserrat JM,
Berruezo A, Coca A, Sitges M, Brugada J, Mont L. Emerging risk factors and
the dose-response relationship between physical activity and lone atrial fibrilla-
tion: a prospective case-control study. Europace 2016;18:5763.
1359. Crump C, Sundquist J, Winkleby MA, Sundquist K. Height, weight, and aerobic
fitness level in relation to the risk of atrial fibrillation. Am J Epidemiol
2018;187:417426.
1360. Mont L, Sambola A, Brugada J, Vacca M, Marrugat J, Elosua R, Pare C, Azqueta
M, Sanz G. Long-lasting sport practice and lone atrial fibrillation. Eur Heart J
2002;23:477482.
1361. Mont L, Tamborero D, Elosua R, Molina I, Coll-Vinent B, Sitges M, Vidal B,
Scalise A, Tejeira A, Berruezo A, Brugada J; GIRAFA Investigators. Physical
activity, height, and left atrial size are independent risk factors for lone atrial
fibrillation in middle-aged healthy individuals. Europace 2008;10:1520.
1362. Guasch E, Mont L. Diagnosis, pathophysiology, and management of exercise-
induced arrhythmias. Nat Rev Cardiol 2017;14:88101.
1363. Stein R, Medeiros CM, Rosito GA, Zimerman LI, Ribeiro JP. Intrinsic sinus and
atrioventricular node electrophysiologic adaptations in endurance athletes. J
Am Coll Cardiol 2002;39:10331038.
1364. Calvo N, Mont L, Tamborero D, Berruezo A, Viola G, Guasch E, Nadal M, Andreu
D, Vidal B, Sitges M, Brugada J. Efficacy of circumferential pulmonary vein ablation
of atrial fibrillation in endurance athletes. Europace 2010;12:3036.
1365. Koopman P, Nuyens D, Garweg C, La Gerche A, De Buck S, Van Casteren L,
Alzand B, Willems R, Heidbuchel H. Efficacy of radiofrequency catheter abla-
tion in athletes with atrial fibrillation. Europace 2011;13:13861393.
1366. Aizer A, Gaziano JM, Cook NR, Manson JE, Buring JE, Albert CM. Relation of
vigorous exercise to risk of atrial fibrillation. Am J Cardiol
2009;103:15721577.
1367. Mozaffarian D, Furberg CD, Psaty BM, Siscovick D. Physical activity and inci-
dence of atrial fibrillation in older adults: the cardiovascular health study.
Circulation 2008;118:800807.
1368. Thelle DS, Selmer R, Gjesdal K, Sakshaug S, Jugessur A, Graff-Iversen S,
Tverdal A, Nystad W. Resting heart rate and physical activity as risk factors
for lone atrial fibrillation: a prospective study of 309,540 men and women.
Heart
2013;99:17551760.
1369. O’Brien B, Burrage PS, Ngai JY, Prutkin JM, Huang CC, Xu X, Chae SH, Bollen
BA, Piccini JP, Schwann NM, Mahajan A, Ruel M, Body SC, Sellke FW, Mathew
J, Muehlschlegel JD. Society of Cardiovascular Anesthesiologists/European
Association of Cardiothoracic Anaesthetists practice advisory for the manage-
ment of perioperative atrial fibrillation in patients undergoing cardiac surgery. J
Cardiothorac Vasc Anesth 2019;33:1226.
1370. Lubitz SA, Yin X, Rienstra M, Schnabel RB, Walkey AJ, Magnani JW, Rahman F,
McManus DD, Tadros TM, Levy D, Vasan RS, Larson MG, Ellinor PT, Benjamin
EJ. Long-term outcomes of secondary atrial fibrillation in the community: the
Framingham Heart Study. Circulation 2015;131:16481655.
1371. Dobrev D, Aguilar M, Heijman J, Guichard JB, Nattel S. Postoperative atrial
fibrillation: mechanisms, manifestations and management. Nat Rev Card iol
2019;16:417436.
1372. Echahidi N, Pibarot P, O’Hara G, Mathieu P. Mechanisms, prevention, and
treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol
2008;51:793801.
1373. Gillinov AM, Bagiella E, Moskowitz AJ, Raiten JM, Groh MA, Bowdish ME,
Ailawadi G, Kirkwood KA, Perrault LP, Parides MK, Smith RL 2nd, Kern JA,
Dussault G, Hackmann AE, Jeffries NO, Miller MA, Taddei-Peters WC, Rose
EA, Weisel RD, Williams DL, Mangusan RF, Argenziano M, Moquete EG,
O’Sullivan KL, Pellerin M, Shah KJ, Gammie JS, Mayer ML, Voisine P, Gelijns
AC, O’Gara PT, Mack MJ, CTSN. Rate control versus rhythm control for atrial
fibrillation after cardiac surgery. N Engl J Med 2016;374:19111921.
1374. Amar D. Postthoracotomy atrial fibrillation. Curr Opin Anaesthesiol
2007;20:4347.
1375. Philip I, Berroeta C, Leblanc I. Perioperative challenges of atrial fibrillation. Curr
Opin Anaesthesiol 2014;27:344352.
1376. Lowres N, Mulcahy G, Jin K, Gallagher R, Neubeck L, Freedman B. Incidence
of postoperative atrial fibrillation recurrence in patients discharged in sinus
rhythm after cardiac surgery: a systematic review and meta-analysis. Interact
Cardiovasc Thorac Surg 2018;26:504511.
1377. Lee SH, Kang DR, Uhm JS, Shim J, Sung JH, Kim JY, Pak HN, Lee MH, Joung
B. New-onset atrial fibrillation predicts long-term newly developed atrial
fibrillation after coronary artery bypass graft. Am Heart J 2014;167:593
600.e1.
1378. Konstantino Y, Zelnik Yovel D, Friger MD, Sahar G, Knyazer B, Amit G.
Postoperative atrial fibrillation following coronary artery bypass graft surgery
predicts long-term atrial fibrillation and stroke. Isr Med Assoc J
2016;18:744748.
1379. Lin MH, Kamel H, Singer DE, Wu YL, Lee M, Ovbiagele B. Perioperative/post-
operative atrial fibrillation and risk of subsequent stroke and/or mortality.
Stroke 2019;50:13641371.
1380. AlTurki A, Marafi M, Proietti R, Cardinale D, Blackwell R, Dorian P, Bessissow
A, Vieira L, Greiss I, Essebag V, Healey JS, Huynh T. Major adverse cardiovas-
cular events associated with postoperative atrial fibrillation after noncardiac
surgery: a systematic review and meta-analysis. Circ Arrhythm Electrophysiol
2020;13:e007437.
1381. Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, Barash PG, Hsu PH,
Mangano DT; Investigators of the Ischemia Research and Education Foundation,
Multicenter Study of Perioperative Ischemia Research Group. A multicenter risk
index for atrial fibrillation after cardiac surgery. JAMA 2004;291:17201729.
1382. Villareal RP, Hariharan R, Liu BC, Kar B, Lee VV, Elayda M, Lopez JA, Rasekh
A, Wilson JM, Massumi A. Postoperative atrial fibrillation and mortality after
coronary artery bypass surgery. J Am Coll Cardiol 2004;43:742748.
1383. Cardinale D, Sandri MT, Colombo A, Salvatici M, Tedeschi I, Bacchiani G,
Beggiato M, Meroni CA, Civelli M, Lamantia G, Colombo N, Veglia F,
Casiraghi M, Spaggiari L, Venturino M, Cipolla CM. Prevention of Atrial
Fibrillation in High-risk Patients Undergoing Lung Cancer Surgery: the
PRESAGE Trial. Ann Surg 2016;264:244251.
1384. Ojima T, Nakamori M, Nakamura M, Katsuda M, Hayata K, Kato T, Kitadani J,
Tabata H, Takeuchi A, Yamaue H. Randomized clinical trial of landiolol hydro-
chloride for the prevention of atrial fibrillation and postoperative complica-
tions after oesophagectomy for cancer. Br J Surg 2017;104:10031009.
1385. Arsenault KA, Yusuf AM, Crystal E, Healey JS, Morillo CA, Nair GM, Whitlock
RP. Interventions for preventing post-operative atrial fibrillation in patients
undergoing heart surgery. Cochrane Database Syst Rev 2013:CD003611.
122 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1386. Ozaydin M, Icli A, Yucel H, Akcay S, Peker O, Erdogan D, Varol E, Dogan A,
Okutan H. Metoprolol vs. carvedilol or carvedilol plus N-acetyl cysteine on
post-operative atrial fibrillation: a randomized, double-blind, placebo-con-
trolled study. Eur Heart J 2013;34:597604.
1387. O’Neal JB, Billings FTt, Liu X, Shotwell MS, Liang Y, Shah AS, Ehrenfeld JM,
Wanderer JP, Shaw AD. Effect of preoperative beta-blocker use on outcomes
following cardiac surgery. Am J Cardiol 2017;120:12931297.
1388. Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, Xavier D,
Chrolavicius S, Greenspan L, Pogue J, Pais P, Liu L, Xu S, Malaga G, Avezum A,
Chan M, Montori VM, Jacka M, Choi P. Effects of extended-release metoprolol
succinate in patients undergoing non-cardiac surgery (POISE trial): a rando-
mised controlled trial. Lancet 2008;371:18391847.
1389. Zhu J, Wang C, Gao D, Zhang C, Zhang Y, Lu Y, Gao Y. Meta-analysis of
amiodarone versus beta-blocker as a prophylactic therapy against
atrial fibrillation following cardiac surgery. Intern Med J
2012;42:10781087.
1390. Auer J, Weber T, Berent R, Puschmann R, Hartl P, Ng CK, Schwarz C, Lehner
E, Strasser U, Lassnig E, Lamm G, Eber B; Study of Prevention of
Postoperative Atrial Fibrillation. A comparison between oral antiarrhythmic
drugs in the prevention of atrial fibrillation after cardiac surgery: the pilot
study of prevention of postoperative atrial fibrillation (SPPAF), a randomized,
placebo-controlled trial. Am Heart J 2004;147:636643.
1391. Buckley MS, Nolan PE Jr, Slack MK, Tisdale JE, Hilleman DE, Copeland JG.
Amiodarone prophylaxis for atrial fibrillation after cardiac surgery: meta-
analysis of dose response and timing of initiation. Pharmacotherapy
2007;27:360368.
1392. Riber LP, Christensen TD, Jensen HK, Hoejsgaard A, Pilegaard HK.
Amiodarone significantly decreases atrial fibrillation in patients undergoing sur-
gery for lung cancer. Ann Thorac Surg 2012;94:339344; discussion 345346.
1393. Tisdale JE, Wroblewski HA, Wall DS, Rieger KM, Hammoud ZT, Young JV,
Kesler KA. A randomized trial evaluating amiodarone for prevention of atrial
fibrillation after pulmonary resection. Ann Thorac Surg 2009;88:886893; dis-
cussion 894895.
1394. Yuan X, Du J, Liu Q, Zhang L. Defining the role of perioperative statin treat-
ment in patients after cardiac surgery: a meta-analysis and systematic review
of 20 randomized controlled trials. Int J Cardiol 2017;228:958966.
1395. Fairley JL, Zhang L, Glassford NJ, Bellomo R. Magnesium status and magnesium
therapy in cardiac surgery: a systematic review and meta-analysis focusing on
arrhythmia prevention. J Crit Care 2017;42:6977.
1396. Tabbalat RA, Hamad NM, Alhaddad IA, Hammoudeh A, Akasheh BF, Khader
Y. Effect of ColchiciNe on the InciDence of atrial fibrillation in open heart sur-
gery patients: END-AF trial. Am Heart J 2016;178:102107.
1397. Ali-Hasan-Al-Saegh S, Mirhosseini SJ, Liakopoulos O, Sabashnikov A, Dehghan
HR, Sedaghat-Hamedani F, Kayvanpour E, Ghaffari N, Vahabzadeh V,
Aghabagheri M, Mozayan MR, Popov AF. Posterior pericardiotomy in cardiac
surgery: systematic review and meta-analysis. Asian Cardiovasc Thorac Ann
2015;23:354362.
1398. Hu XL, Chen Y, Zhou ZD, Ying J, Hu YH, Xu GH. Posterior pericardiotomy
for the prevention of atrial fibrillation after coronary artery bypass grafting: a
meta-analysis of randomized controlled trials. Int J Cardiol 2016;215:252256.
1399. Wang W, Mei YQ, Yuan XH, Feng XD. Clinical efficacy of epicardial applica-
tion of drug-releasing hydrogels to prevent postoperative atrial fibrillation. J
Thorac Cardiovasc Surg 2016;151:8085.
1400. Dieleman JM, Nierich AP, Rosseel PM, van der Maaten JM, Hofland J, Diephuis
JC, Schepp RM, Boer C, Moons KG, van Herwerden LA, Tijssen JG, Numan
SC, Kalkman CJ, van Dijk D; Dexamethasone for Cardiac Surgery Study
Group. Intraoperative high-dose dexamethasone for cardiac surgery: a
randomized controlled trial. JAMA 2012;308:17611767.
1401. Whitlock RP, Devereaux PJ, Teoh KH, Lamy A, Vincent J, Pogue J, Paparella D,
Sessler DI, Karthikeyan G, Villar JC, Zuo Y, Avezum A, Quantz M, Tagarakis
GI, Shah PJ, Abbasi SH, Zheng H, Pettit S, Chrolavicius S, Yusuf S; SIRS
Investigators. Methylprednisolone in patients undergoing cardiopulmonary
bypass (SIRS): a randomised, double-blind, placebo-controlled trial. Lancet
2015;386:12431253.
1402. Saxena A, Dinh DT, Smith JA, Shardey GC, Reid CM, Newcomb AE.
Usefulness of postoperative atrial fibrillation as an independent predictor for
worse early and late outcomes after isolated coronary artery bypass grafting
(multicenter Australian study of 19,497 patients). Am J Cardiol
2012;109:219225.
1403. Almassi GH, Schowalter T, Nicolosi AC, Aggarwal A, Moritz TE, Henderson
WG, Tarazi R, Shroyer AL, Sethi GK, Grover FL, Hammermeister KE. Atrial
fibrillation after cardiac surgery: a major morbid event?Ann Surg
1997;226:501511; discussion 511513.
1404. Gialdini G, Nearing K, Bhave PD, Bonuccelli U, Iadecola C, Healey JS, Kamel
H. Perioperative atrial fibrillation and the long-term risk of ischemic stroke.
JAMA 2014;312:616622.
1405. Horwich P, Buth KJ, Legare JF. New onset postoperative atrial fibrillation is
associated with a long-term risk for stroke and death following cardiac sur-
gery. J Card Surg 2013;28:813.
1406. Ahlsson A, Fengsrud E, Bodin L, Englund A. Postoperative atrial fibrillation in
patients undergoing aortocoronary bypass surgery carries an eightfold risk of
future atrial fibrillation and a doubled cardiovascular mortality. Eur J
Cardiothorac Surg 2010;37:13531359.
1407. Rubin DA, Nieminski KE, Reed GE, Herman MV. Predictors, prevention, and
long-term prognosis of atrial fibrillation after coronary artery bypass graft
operations. J Thorac Cardiovasc Surg 1987;94:331335.
1408. Butt JH, Xian Y, Peterson ED, Olsen PS, Rorth R, Gundlund A, Olesen JB,
Gislason GH, Torp-Pedersen C, Kober L, Fosbol EL. Long-term thromboem-
bolic risk in patients with postoperative atrial fibrillation after coronary artery
bypass graft surgery and patients with nonvalvular atrial fibrillation. JAMA
Cardiol 2018;
3:417424.
1409. Butt JH, Olesen JB, Havers-Borgersen E, Gundlund A, Andersson C, Gislason
GH, Torp-Pedersen C, Kober L, Fosbol EL. Risk of thromboembolism associ-
ated with atrial fibrillation following noncardiac surgery. J Am Coll Cardiol
2018;72:20272036.
1410. POISE Study group., Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar
JC, Xavier D, Chrolavicius S, Greenspan L, Pogue J, Pais P, Liu L, Xu S, Malaga
G, Avezum A, Chan M, Montori VM, Jacka M, Choi P. Effects of extended-
release metoprolol succinate in patients undergoing non-cardiac surgery
(POISE trial): a randomised controlled trial. Lancet 2008;371:18391847.
1411. Leonardi M, Bissett J. Prevention of atrial fibrillation. Curr Opin Cardiol
2005;20:417423.
1412. Roberts JD, Dewland TA, Glidden DV, Hoffmann TJ, Arking DE, Chen LY,
Psaty BM, Olgin JE, Alonso A, Heckbert SR, Marcus GM. Impact of genetic var-
iants on the upstream efficacy of renin-angiotensin system inhibitors for the
prevention of atrial fibrillation. Am Heart J 2016;175:917.
1413. Pena JM, MacFadyen J, Glynn RJ, Ridker PM. High-sensitivity C-reactive protein,
statin therapy, and risks of atrial fibrillation: an exploratory analysis of the
JUPITER trial. Eur Heart J 2012;33:531537.
1414. Maggioni AP, Fabbri G, Lucci D, Marchioli R, Franzosi MG, Latini R, Nicolosi
GL, Porcu M, Cosmi F, Stefanelli S, Tognoni G; GISSI-HF Investigators. Effects
of rosuvastatin on atrial fibrillation occurrence: ancillary results of the GISSI-
HF trial. Eur Heart J 2009;30:23272336.
1415. Zhou X, Du JL, Yuan J, Chen YQ. Statin therapy is beneficial for the preven-
tion of atrial fibrillation in patients with coronary artery disease: a meta-analy-
sis. Eur J Pharmacol 2013;707:104111.
1416. Fang WT, Li HJ, Zhang H, Jiang S. The role of statin therapy in the prevention
of atrial fibrillation: a meta-analysis of randomized controlled trials. Br J Clin
Pharmacol 2012;74:744756.
1417. Macfarlane PW, Murray H, Sattar N, Stott DJ, Ford I, Buckley B, Jukema JW,
Westendorp RG, Shepherd J. The incidence and risk factors for new onset
atrial fibrillation in the PROSPER study. Europace 2011;13:634639.
1418. Haywood LJ, Ford CE, Crow RS, Davis BR, Massie BM, Einhorn PT, Williard
A; ALLHAT Collaborative Research Group. Atrial fibrillation at baseline and
during follow-up in ALLHAT (Antihypertensive and Lipid-Lowering
Treatment to Prevent Heart Attack Trial). JAmCollCardiol2009;54:
20232031.
1419. Schwartz GG, Chaitman BR, Goldberger JJ, Messig M. High-dose atorvastatin
and risk of atrial fibrillation in patients with prior stroke or transient ischemic
attack: analysis of the Stroke Prevention by Aggressive Reduction in
Cholesterol Levels (SPARCL) trial. Am Heart J 2011;161:993999.
1420. Fauchier L, Clementy N, Babuty D. Statin therapy and atrial fibrillation: system-
atic review and updated meta-analysis of published randomized controlled tri-
als. Curr Opin Cardiol 2013;28:718.
1421. Yang Q, Qi X, Li Y. The preventive effect of atorvastatin on atrial fibrillation: a
meta-analysis of randomized controlled trials. BMC Cardiovasc Disord
2014;14:99.
1422. Martino A, Pezzi L, Magnano R, Salustri E, Penco M, Calo L. Omega 3 and
atrial fibrillation: where are we?World J Cardiol 2016;8:114119.
1423. Linde C, Bongiorni MG, Birgersdotter-Green U, Curtis AB, Deisenhofer I,
Furokawa T, Gillis AM, Haugaa KH, Lip GYH, Van Gelder I, Malik M, Poole J,
Potpara T, Savelieva I, Sarkozy A; ESC Scientific Document Group. Sex differ-
ences in cardiac arrhythmia: a consensus document of the European Heart
Rhythm Association, endorsed by the Heart Rhythm Society and Asia Pacific
Heart Rhythm Society. Europace 2018;20:15651565ao.
1424. Potpara TS, Marinkovic JM, Polovina MM, Stankovic GR, Seferovic PM, Ostojic
MC, Lip GY. Gender-related differences in presentation, treatment and long-
term outcome in patients with first-diagnosed atrial fibrillation and structurally
normal heart: the Belgrade atrial fibrillation study. Int J Cardiol
2012;161:3944.
1425. Potpara TS, Blomstrom-Lundqvist C. Sex-related differences in atrial fibrilla-
tion: can we discern true disparities from biases?Heart 2017;103:979981.
ESC Guidelines 123

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1426. Piccini JP, Simon DN, Steinberg BA, Thomas L, Allen LA, Fonarow GC, Gersh
B, Hylek E, Kowey PR, Reiffel JA, Naccarelli GV, Chan PS, Spertus JA, Peterson
ED; Outcomes Registry for Better Informed Treatment of Atrial Fibrillation
Investigators and Patients. Differences in clinical and functional outcomes of
atrial fibrillation in women and men: two-year results from the ORBIT-AF
registry. JAMA Cardiol 2016;1:282291.
1427. Lang C, Seyfang L, Ferrari J, Gattringer T, Greisenegger S, Willeit K, Toell T,
Krebs S, Brainin M, Kiechl S, Willeit J, Lang W, Knoflach M; Austrian Stroke
Registry Collaborators. Do women with atrial fibrillation experience more
severe strokes? Results from the Austrian Stroke Unit Registry. Stroke
2017;48:778780.
1428. Sullivan RM, Zhang J, Zamba G, Lip GY, Olshansky B. Relation of gender-
specific risk of ischemic stroke in patients with atrial fibrillation to differences
in warfarin anticoagulation control (from AFFIRM). Am J Cardiol
2012;110:17991802.
1429. Rienstra M, Van Veldhuisen DJ, Hagens VE, Ranchor AV, Veeger NJ, Crijns HJ,
Van Gelder IC; RACE Investigators. Gender-related differences in rhythm con-
trol treatment in persistent atrial fibrillation: data of the Rate Control Versus
Electrical Cardioversion (RACE) study. J Am Coll Cardiol 2005;46:12981306.
1430. Lehmann MH, Timothy KW, Frankovich D, Fromm BS, Keating M, Locati EH,
Taggart RT, Towbin JA, Moss AJ, Schwartz PJ, Vincent GM. Age-gender influ-
ence on the rate-corrected QT interval and the QT-heart rate relation in fam-
ilies with genotypically characterized long QT syndrome. J Am Coll Cardiol
1997;29:9399.
1431. Zylla MM, Brachmann J, Lewalter T, Hoffmann E, Kuck KH, Andresen D,
Willems S, Eckardt L, Tebbenjohanns J, Spitzer SG, Schumacher B, Hochadel
M, Senges J, Katus HA, Thomas D. Sex-related outcome of atrial fibrillation
ablation: insights from the German Ablation Registry. Heart Rhythm
2016;13:18371844.
1432. Patel N, Deshmukh A, Thakkar B, Coffey JO, Agnihotri K, Patel A, Ainani N,
Nalluri N, Patel N, Patel N, Patel N, Badheka AO, Kowalski M, Hendel R,
Viles-Gonzalez J, Noseworthy PA, Asirvatham S, Lo K, Myerburg RJ, Mitrani
RD. Gender, race, and health insurance status in patients undergoing catheter
ablation for atrial fibrillation. Am J Cardiol 2016;117:11171126.
1433. Emdin CA, Wong CX, Hsiao AJ, Altman DG, Peters SA, Woodward M,
Odutayo AA. Atrialfibrillation as risk factor for cardiovascular disease and
death in women compared with men: systematic review and meta-analysis of
cohort studies. BMJ 2016;532:h7013.
1434. Lip GY, Laroche C, Popescu MI, Rasmussen LH, Vitali-Serdoz L, Dan GA,
Kalarus Z, Crijns HJ, Oliveira MM, Tavazzi L, Maggioni AP, Boriani G.
Improved outcomes with European Society of Cardiology guideline-adherent
antithrombotic treatment in high-risk patients with atrial fibrillation: a report
from the EORP-AF General Pilot Registry. Europace 2015;17:17771786.
1435. Proietti M, Nobili A, Raparelli V, Napoleone L, Mannucci PM, Lip GY; REPOSI
Investigators. Adherence to antithrombotic therapy guidelines improves mor-
tality among elderly patients with atrial fibrillation: insights from the REPOSI
study. Clin Res Cardiol 2016;105:912920.
1436. Kirchhof P, Ammentorp B, Darius H, De Caterina R, Le Heuzey JY, Schilling
RJ, Schmitt J, Zamorano JL. Management of atrial fibrillation in seven European
countries after the publication of the 2010 ESC Guidelines on atrial fibrillation:
primary results of the PREvention oF thromboemolic events European
Registry in Atrial Fibrillation (PREFER in AF). Europace 2014;
16:614.
1437. Lip GY, Laroche C, Ioachim PM, Rasmussen LH, Vitali-Serdoz L, Petrescu L,
Darabantiu D, Crijns HJ, Kirchhof P, Vardas P, Tavazzi L, Maggioni AP, Boriani
G. Prognosis and treatment of atrial fibrillation patients by European cardiolo-
gists: one year follow-up of the EURObservational Research Programme
Atrial Fibrillation General Registry Pilot Phase (EORP-AF Pilot registry). Eur
Heart J 2014;35:33653376.
1438. Jortveit J, Pripp AH, Langorgen J, Halvorsen S. Poor adherence to guideline
recommendations among patients with atrial fibrillation and acute myocardial
infarction. Eur J Prev Cardiol 2019:2047487319841940.
1439. Potpara TS, Dan GA, Trendafilova E, Goda A, Kusljugic Z, Manola S, Music L,
Musetescu R, Badila E, Mitic G, Paparisto V, Dimitrova ES, Polovina MM,
Petranov SL, Djergo H, Loncar D, Bijedic A, Brusich S, Lip GY; Balkan-AF
Investigators. Stroke prevention in atrial fibrillation and ‘real world’ adherence
to guidelines in the Balkan region: the BALKAN-AFSurvey. Sci Rep
2016;6:20432.
1440. Kim H, Kim TH, Cha MJ, Lee JM, Park J, Park JK, Kang KW, Shim J, Uhm JS,
Kim J, Park HW, Choi EK, Kim JB, Kim C, Lee YS, Joung B. A prospective sur-
vey of atrial fibrillation management for real-world guideline adherence:
COmparison study of Drugs for symptom control and complication
prEvention of Atrial Fibrillation (CODE-AF) Registry. Korean Circ J
2017;47:877887.
1441. Miyazawa K, Li YG, Rashed WA, Al Mahmeed W, Shehab A, Zubaid M, Lip
GYH. Secondary stroke prevention and guideline adherent antithrombotic
treatment in patients with atrial fibrillation: insights from the Gulf Survey of
Atrial Fibrillation events (Gulf SAFE). Int J Cardiol 2019;274:126131.
1442. Camm AJ, Accetta G, Ambrosio G, Atar D, Bassand JP, Berge E, Cools F,
Fitzmaurice DA, Goldhaber SZ, Goto S, Haas S, Kayani G, Koretsune Y,
Mantovani LG, Misselwitz F, Oh S, Turpie AG, Verheugt FW, Kakkar AK;
GARFIELD-AF Investigators. Evolving antithrombotic treatment patterns for
patients with newly diagnosed atrial fibrillation. Heart 2017;103:307314.
1443. Steinberg BA, Gao H, Shrader P, Pieper K, Thomas L, Camm AJ, Ezekowitz
MD, Fonarow GC, Gersh BJ, Goldhaber S, Haas S, Hacke W, Kowey PR,
Ansell J, Mahaffey KW, Naccarelli G, Reiffel JA, Turpie A, Verheugt F, Piccini
JP, Kakkar A, Peterson ED, Fox KAA, Garfield AF; ORBIT-AF Investigators.
International trends in clinical characteristics and oral anticoagulation treat-
ment for patients with atrial fibrillation: results from the GARFIELD-AF,
ORBIT-AF I, and ORBIT-AF II registries. Am Heart J 2017;194:132140.
1444. Leef GC, Perino AC, Askari M, Fan J, Ho PM, Olivier CB, Longo L, Mahaffey
KW, Turakhia MP. Appropriateness of direct oral anticoagulant dosing in
patients with atrial fibrillation: insights from the Veterans Health
Administration. J Pharm Pract 2019:897190019828270.
1445. Dupree L, DeLosSantos M, Smotherman C. Evaluation of adherence to
guideline-directed antithrombotic therapy for atrial fibrillation at hospital dis-
charge. J Cardiovasc Pharmacol Ther 2018;23:502508.
1446. Heidbuchel H, Dagres N, Antz M, Kuck KH, Lazure P, Murray S, Carrera C,
Hindricks G, Vahanian A. Major knowledge gaps and system barriers to guide-
line implementation among European physicians treating patients with atrial
fibrillation: a European Society of Cardiology international educational needs
assessment. Europace 2018;20:19191928.
1447. Desteghe L, Germeys J, Vijgen J, Koopman P, Dilling-Boer D, Schurmans J,
Delesie M, Dendale P, Heidbuchel H. Effectiveness and usability of an online
tailored education platform for atrial fibrillation patients undergoing a direct
current cardioversion or pulmonary vein isolation. Int J Cardiol
2018;272:123129.
1448. Marquez-Contreras E, Martell-Claros N, Marquez-Rivero S, Hermida-Campa
E, Gracia-Diez C, Sanchez-Lopez E, Gil-Guillen V; Compliance and Inertia
Working Group, Spanish Society of Hypertension (SEH-LELHA). Strategies
for improving dabigatran adherence for stroke prevention in patients with
non-valvular atrial fibrillation: education and drug intake reminders (FACILITA
study). Curr Med Res Opin 2018;34:13011308.
1449. Piccini JP, Xu H, Cox M, Matsouaka RA, Fonarow GC, Butler J, Curtis AB,
Desai N, Fang M, McCabe PJ, Page Ii RL, Turakhia M, Russo AM, Knight BP,
Sidhu M, Hurwitz JL, Ellenbogen KA, Lewis WR; Get With The Guidelines-
AFIB Clinical Working Group and Hospitals. Adherence to guideline-directed
stroke prevention therapy for atrial fibrillation is achievable. Circulation
2019;139:14971506.
1450. Richardson KM, Singh J, Munoz D, Damp JB, Mendes LA. Improving practice
guideline adherence through peer feedback: impact of an ambulatory cardiol-
ogy curriculum. Teach Learn Med 2018;30:328336.
1451. Ferguson C, Hickman LD, Phillips J, Newton PJ, Inglis SC, Lam L, Bajorek BV.
An mHealth intervention to improve nurses’ atrial fibrillation and anticoagula-
tion knowledge and practice: the EVICOAG study. Eur J Cardiovasc Nurs
2019;18:715.
1452. Siebenhofer A, Ulrich LR, Mergenthal K, Berghold A, Pregartner G,
Kemperdick B, Schulz-Rothe S, Rauck S, Harder S, Gerlach FM, Petersen JJ.
Primary care management for patients receiving long-term antithrombotic
treatment: a cluster-randomized controlled trial. PLoS One 2019;14:e0209366.
1453. Heidenreich PA, Solis P, Estes NAM 3rd, Fonarow GC, Jurgens CY, Marine JE,
McManus DD, McNamara RL. 2016 ACC/AHA clinical performance and qual-
ity measures for adults with atrial fibrillation or atrial flutter: a report of the
American College of Cardiology/American Heart Association Task Force on
performance measures. J Am Coll Cardiol 2016;68:525568.
1454. Lewis WR, Piccini JP, Turakhia MP, Curtis AB, Fang M, Suter RE, Page RL, 2nd,
Fonarow GC. Get With The Guidelines AFIB: novel quality improvement
registry for hospitalized patients with atrial fibrillation. Circ Cardiovasc Qual
Outcomes 2014;7:770777.
1455. Friedman DJ, Al-Khatib SM. Measuring quality in electrophysiology. J Interv
Card Electrophysiol 2016;47:510.
1456. Schulman S, Kearon C; Subcommittee on Control of Anticoagulation of the
Scientific and Standardization Committee of the International Society on
Thrombosis and Haemostasis. Definition of major bleeding in clinical investiga-
tions of antihemostatic medicinal products in non-surgical patients. J Thromb
Haemost 2005;3:692694.
1457. Schulman S, Angeras U, Bergqvist D, Eriksson B, Lassen MR, Fisher W;
Subcommittee on Control of Anticoagulation of the Scientific and Standardization
Committee of the International Society on Thrombosis and Haemostasis.
Definition of major bleeding in clinical investigations of antihemostatic medicinal
products in surgical patients. JThrombHaemost2010;8:202204.
124 ESC Guidelines

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
1458. Diederichsen SZ, Haugan KJ, Brandes A, Lanng MB, Graff C, Krieger D,
Kronborg C, Holst AG, Kober L, Hojberg S, Svendsen JH. Natural history of
subclinical atrial fibrillation detected by implanted loop recorders. J Am Coll
Cardiol 2019;74:27712781.
1459. Swiryn S, Orlov MV, Benditt DG, DiMarco JP, Lloyd-Jones DM, Karst E,
Qu F, Slawsky MT, Turkel M, Waldo AL; RATE Registry Investigators.
Clinical implications of brief device-detected atrial tachyarrhythmias in a
cardiac rhythm management device population: results from the Registry
of Atrial Tachycardia and Atrial Fibrillation Episodes. Circulatio n
2016;134:11301140.
1460. Pastori D, Miyazawa K, Li Y, Szekely O, Shahid F, Farcomeni A, Lip GYH.
Atrial high-rate episodes and risk of major adverse cardiovascular events in
patients with cardiac implantable electronic devices. Clin Res Cardiol
2020;109:96102.
1461. Gonzalez M, Keating RJ, Markowitz SM, Liu CF, Thomas G, Ip JE, Lerman BB,
Cheung JW. Newly detected atrial high rate episodes predict long-term mor-
tality outcomes in patients with permanent pacemakers. Heart Rhythm
2014;11:22142221.
1462. Gorenek BC, Bax J, Boriani G, Chen SA, Dagres N, Glotzer TV, Healey JS,
Israel CW, Kudaiberdieva G, Levin LA, Lip GYH, Martin D, Okumura K,
Svendsen JH, Tse HF, Botto GLC-C; ESC Scientific Document Group. Device-
detected subclinical atrial tachyarrhythmias: definition, implications and man-
agement an European Heart Rhythm Association (EHRA) consensus docu-
ment, endorsed by Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm
Society (APHRS) and Sociedad Latinoamericana de Estimulacion Cardiaca y
Electrofisiologia (SOLEACE). Europace 2017;19:15561578.
1463. Nasir JM, Pomeroy W, Marler A, Hann M, Baykaner T, Jones R, Stoll R, Hursey
K, Meadows A, Walker J, Kindsvater S. Predicting determinants of atrial fibrilla-
tion or flutter for therapy elucidation in Patients at Risk for Thromboembolic
Events (PREDATE AF) study. Heart Rhythm 2017;14:955961.
1464. Reiffel JA, Verma A, Kowey PR, Halperin JL, Gersh BJ, Wachter R, Pouliot E,
Ziegler PD; REVEAL AF Investigators. Incidence of previously undiagnosed
atrial fibrillation using insertable cardiac monitors in a high-risk population: the
REVEAL AF study. JAMA Cardiol 2017;2:11201127.
1465. Kaplan RM, Koehler J, Ziegler PD, Sarkar S, Zweibel S, Passman RS. Stroke
risk as a function of atrial fibrillation duration and CHA2DS2-VASc score.
Circulation 2019;140:16391646.
1466. Celikyurt U, Knecht S, Kuehne M, Reichlin T, Muehl A, Spies F, Osswald S,
Sticherling C. Incidence of new-onset atrial fibrillation after cavotricuspid isth-
mus ablation for atrial flutter. Europace 2017;19:17761780.
1467. Bertaglia E, Bonso A, Zoppo F, Proclemer A, Verlato R, Coro L, Mantovan R,
Themistoclakis S, Raviele A, Pascotto P; North-Eastern Italian Study on Atrial
Flutter Ablation Investigators. Different clinical courses and predictors of atrial
fibrillation occurrence after transisthmic ablation in patients with preablation
lone atrial flutter, coexistent atrial fibrillation, and drug induced atrial flutter.
Pacing Clin Electrophysiol 2004;27:15071512.
1468. Nabar A, Rodriguez LM, Timmermans C, van Mechelen R, Wellens HJ. Class
IC antiarrhythmic drug induced atrial flutter: electrocardiographic and electro-
physiological findings and their importance for long term outcome after right
atrial isthmus ablation. Heart 2001;85:424429.
1469. Enriquez A, Sarrias A, Villuendas R, Ali FS, Conde D, Hopman WM, Redfearn
DP, Michael K, Simpson C, De Luna AB, Bayes-Genis A, Baranchuk A. New-
onset atrial fibrillation after cavotricuspid isthmus ablation: identification of
advanced interatrial block is key. Europace 2015;
17:12891293.
1470. Maskoun W, Pino MI, Ayoub K, Llanos OL, Almomani A, Nairooz R, Hakeem
A, Miller J. Incidence of atrial fibrillation after atrial flutter ablation. JACC Clin
Electrophysiol 2016;2:682690.
1471. Reithmann C, Hoffmann E, Spitzlberger G, Dorwarth U, Gerth A, Remp T,
Steinbeck G. Catheter ablation of atrial flutter due to amiodarone therapy for
paroxysmal atrial fibrillation. Eur Heart J 2000;21:565572.
1472. Vadmann H, Nielsen PB, Hjortshoj SP, Riahi S, Rasmussen LH, Lip GY, Larsen
TB. Atrial flutter and thromboembolic risk: a systematic review. Heart
2015;101:14461455.
1473. Van Gelder IC, Crijns HJ, Van Gilst WH, Verwer R, Lie KI. Prediction of
uneventful cardioversion and maintenance of sinus rhythm from direct-current
electrical cardioversion of chronic atrial fibrillation and flutter. Am J Cardiol
1991;68:4146.
1474. Gillis AM, Unterberg-Buchwald C, Schmidinger H, Massimo S, Wolfe K,
Kavaney DJ, Otterness MF, Hohnloser SH; GEM III AT Worldwide
Investigators. Safety and efficacy of advanced atrial pacing therapies for atrial
tachyarrhythmias in patients with a new implantable dual chamber cardi-
overter-defibrillator. J Am Coll Cardiol 2002;40:16531659.
1475. Crijns HJ, Van Gelder IC, Kingma JH, Dunselman PH, Gosselink AT, Lie KI.
Atrial flutter can be terminated by a class III antiarrhythmic drug but not by a
class IC drug. Eur Heart J 1994;15:14031408.
1476. Ellenbogen KA, Stambler BS, Wood MA, Sager PT, Wesley RC, Jr., Meissner
MC, Zoble RG, Wakefield LK, Perry KT, Vanderlugt JT. Efficacy of intravenous
ibutilide for rapid termination of atrial fibrillation and atrial flutter: a dose-
response study. J Am Coll Cardiol 1996;28:130136.
1477. Falk RH, Pollak A, Singh SN, Friedrich T. Intravenous dofetilide, a class III
antiarrhythmic agent, for the termination of sustained atrial fibrillation or
flutter. Intravenous Dofetilide Investigators. J Am Coll Cardiol
1997;29:385390.
1478. Singh S, Zoble RG, Yellen L, Brodsky MA, Feld GK, Berk M, Billing CB, Jr.
Efficacy and safety of oral dofetilide in converting to and maintaining sinus
rhythm in patients with chronic atrial fibrillation or atrial flutter: the sympto-
matic atrial fibrillation investigative research on dofetilide (SAFIRE-D) study.
Circulation 2000;102:23852390.
1479. Crozier IG, Ikram H, Kenealy M, Levy L. Flecainide acetate for conversion of
acute supraventricular tachycardia to sinus rhythm. Am J Cardiol
1987;59:607609.
1480. Murdock CJ, Kyles AE, Yeung-Lai-Wah JA, Qi A, Vorderbrugge S, Kerr CR.
Atrial flutter in patients treated for atrial fibrillation with propafenone. Am J
Cardiol 1990;66:755757.
1481. Da Costa A, Thevenin J, Roche F, Romeyer-Bouchard C, Abdellaoui L,
Messier M, Denis L, Faure E, Gonthier R, Kruszynski G, Pages JM, Bonijoly S,
Lamaison D, Defaye P, Barthelemy JC, Gouttard T, Isaaz K; Loire-Arde`che-
Droˆ me-Ise`re-Puy-de-Doˆme Trial of Atrial Flutter Investigators. Results from
the Loire-Arde`che-Droˆme-Ise`re-Puy-de-Dome (LADIP) trial on atrial flutter, a
multicentric prospective randomized study comparing amiodarone and radio-
frequency ablation after the first episode of symptomatic atrial flutter.
Circulation 2006;114:16761681.
1482. Schwartzman D, Callans DJ, Gottlieb CD, Dillon SM, Movsowitz C,
Marchlinski FE. Conduction block in the inferior vena caval-tricuspid valve isth-
mus: association with outcome of radiofrequency ablation of type I atrial flut-
ter. J Am Coll Cardiol 1996;28:15191531.
1483. Wasmer K, Monnig G, Bittner A, Dechering D, Zellerhoff S, Milberg P, Kobe J,
Eckardt L. Incidence, characteristics, and outcome of left atrial tachycardias
after circumferential antral ablation of atrial fibrillation. Heart Rhythm
2012;9:16601666.
1484. Satomi K, Bansch D, Tilz R, Chun J, Ernst S, Antz M, Greten H, Kuck KH,
Ouyang F. Left atrial and pulmonary vein macroreentrant tachycardia associ-
ated with double conduction gaps: a novel type of man-made tachycardia after
circumferential pulmonary vein isolation. Heart Rhythm 2008;5:4351.
1485. Chugh A, Oral H, Lemola K, Hall B, Cheung P, Good E, Tamirisa K, Han J,
Bogun F, Pelosi F Jr, Morady F. Prevalence, mechanisms, and clinical significance
of macroreentrant atrial tachycardia during and following left atrial ablation for
atrial fibrillation. Heart Rhythm 2005;2:464471.
1486. Goette A, Auricchio A, Boriani G, Braunschweig F, Terradellas JB, Burri H,
Camm AJ, Crijns H, Dagres N, Deharo JC, Dobrev D, Hatala R, Hindricks G,
Hohnloser SH, Leclercq C, Lewalter T, Lip GYH, Merino JL, Mont L, Prinzen
F, Proclemer A, Purerfellner H, Savelieva I, Schilling R, Steffel J, van Gelder
IC, Zeppenfeld K, Zupan I, Heidbuchel H. EHRA White Paper:
knowledge gaps in arrhythmia management status 2019. Europace 2019;
21:993994.
1487. De With RR, Marcos EG, Dudink E, Spronk HM, Crijns H, Rienstra M, Van
Gelder IC. Atrial fibrillation progression risk factors and associated cardiovas-
cular outcome in well-phenotyped patients: data from the AF-RISK study.
Europace 2020;22:352360.
1488. Andrade JG, Deyell MW, Lee AY, Macle L. Sex differences in atrial fibrillation.
Canadian J Cardiol 2018;34:429436.
1489. Potpara TS, Ferro C, Lip GYH, Dan GA, Lenarczyk R, Mallamaci F, Ortiz A,
Sarafidis P, Ekart R, Dagres N. Management of atrial fibrillation in patients with
chronic kidney disease in clinical practice: a joint European Heart Rhythm
Association (EHRA) and European Renal Association/European Dialysis and
Transplantation Association (ERA/EDTA) physician-based survey. Europace
2020;22:496505.
1490. Al-Khatib SM, Benjamin EJ, Buxton AE, Calkins H, Chung MK, Curtis AB,
Desvigne-Nickens P, Jais P, Packer DL, Piccini JP, Rosenberg Y, Russo AM,
Wang PJ, Cooper LS, Go AS, Workshop C. Research needs and priorities for
catheter ablation of atrial fibrillation: a report from a National Heart, Lung,
and Blood Institute Virtual Workshop. Circulation 2020;141:482492.
1491. Nielsen JC, Lin YJ, de Oliveira Figueiredo MJ, Sepehri Shamloo A, Alfie A,
Boveda S, Dagres N, Di Toro D, Eckhardt LL, Ellenbogen K, Hardy C, Ikeda T,
ESC Guidelines 125

.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Jaswal A, Kaufman E, Krahn A, Kusano K, Kutyifa V, Lim HS, Lip GYH, Nava-
Townsend S, Pak HN, RodrU
´
guez Diez G, Sauer W, Saxena A, Svendsen JH,
Vanegas D, Vaseghi M, Wilde A, Bunch TJ; ESC Scientific Document Group,
Buxton AE, Calvimontes G, Chao TF, Eckardt L, Estner H, Gillis AM, Isa R,
Kautzner J, Maury P, Moss JD, Nam GB, Olshansky B, Pava Molano LF,
Pimentel M, Prabhu M, Tzou WS, Sommer P, Swampillai J, Vidal A, Deneke T,
Hindricks G, Leclercq C. European Heart Rhythm Association (EHRA)/Heart
Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin
American Heart Rhythm Society (LAHRS) expert consensus on risk assess-
ment in cardiac arrhythmias: use the right tool for the right outcome, in the
right population. Europace 2020;22:11471148.
1492. Blessberger H, Lewis SR, Pritchard MW, Fawcett LJ, Domanovits H, Schlager
O, Wildner B, Kammler J, Steinwender C. Perioperative beta-blockers for pre-
venting surgery-related mortality and morbidity in adults undergoing cardiac
surgery. Cochrane Database Syst Rev 2019 23;9:CD013435.
126 ESC Guidelines
