
Radiography
Student
Handbook
2023
Rev.2023
1
RADIOGRAPHY PROGRAM HANDBOOK
Table of Contents
Welcome Letter 4
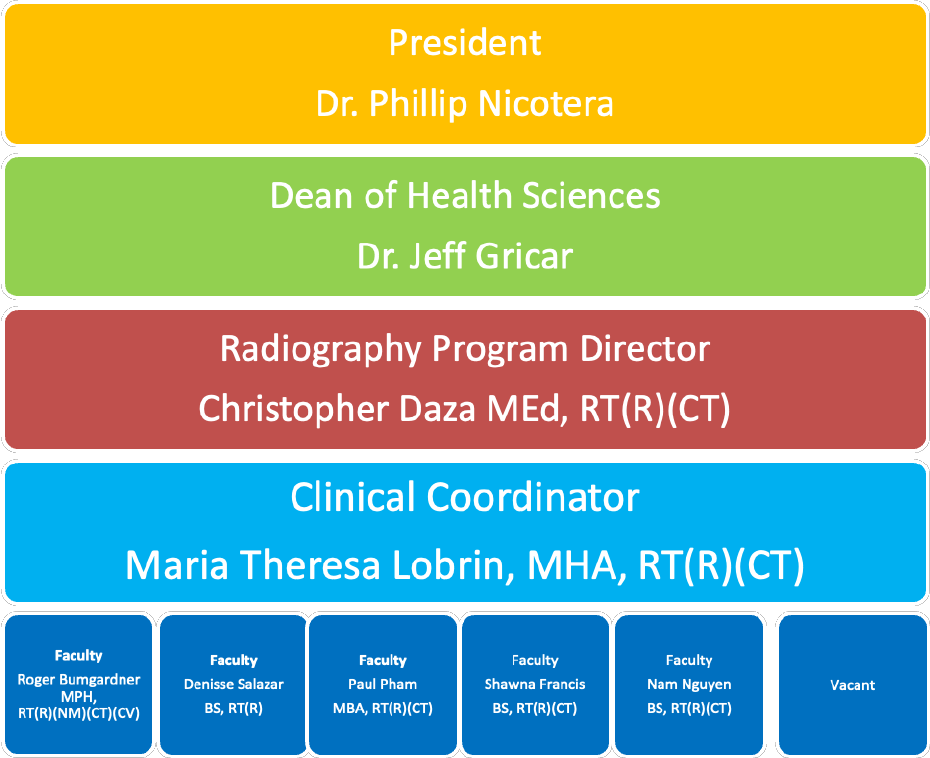
Program Organizational Chart 5
Program Description 6
Non-discrimination Policy 6
Mission Statement 6
Program Goals 6
Program Benchmarks 7
Expected Outcomes 7-8
Program Roles Defined 8-10
Program Effectiveness Data 11
Change of Personal Information 12
Parking 12
Health Insurance 12
Medical Liability Insurance 12
Radiation Monitor Fee 12
Registration/Enrollment Process 12
ADA Considerations 13
Advisement 13
Student Services 13
Academic Success Center 13
College Identification Badge 13
Lead Markers 13
Radiography Program Student Organization 13
Confidentiality Statement 14
Advisory Committee 14
Radiography Faculty & Adjunct 14
Clinical Affiliates 16-18
Radiography Program Curriculum 19
Curriculum Sequencing 19
Final Grade of FX 19-21
Description of the Semesters 21-23
Course Evaluations 23
Book List 24-26
Program Estimated Cost 27
Technical Standards for Radiography 28-30
ARRT Standards of Ethics 30
Scholarship Information 31
Program Policies 32
ADA Compliance 32
Title IX Amendment 33
2
Texas House Bill 1508
33
Attendance Policy
34
Bereavement Leave Policy
34
Catastrophic Leave
34
Pregnancy Leave
34
Medical Leave
35
Drug Screen & Background
35
Drug Testing
35
Due Process
36
Financial Aid & Veteran’s Benefits
36
Harassment
37
JRCERT Compliance
37-38
Pregnancy Policy
39-40
Radiation Safety and Monitor Policy
40-41
Readmission Policy
42
Transfer Policy
42
Withdrawals
42
Program Procedures
42
Graduation
42
Graduation Requirements
43
Application for ARRT Examination
43
Application for Certification TMB
44
Program Readmission Procedures
45-46
Academic and Clinical Standards
47
Social Networking and Students in Health Care Programs
47
Trajecsys
47
Trajecsys Digital Clock In/Out
47-48
Clinical Attendance
48-49
Definitions
49-50
Personal Insurance
50
Clinical Code of Conduct
50-51
Unsafe or Unprofessional Practice
51-53
Clinical Supervision Policy-Direct/Indirect and Repeat Images
53-54
Clinical Objectives
55
Professional Behavior
56
Probation Guidelines for Clinic
57-58
Entry into Clinical Courses
58
Health Record Requirements
58
COVID Policy
58-59
CPR Requirement
60
Dress Code and Uniforms
60-62
ID Badges
62
Student Safety
62
Transportation
62
Weather Emergencies
62-63
Clinical Education Assignments
63
3
Lead Markers 63
Dosimeter 63-64
MRI Safety 64
Pregnancy 64
Injury/Surgery/Illness 64
Competencies 64-65
Testing 65
Reviewing Trajecsys 65
Readmitted & Transfer Students 66
ARRT Requirements 67-72
Appendices
Appendix A: Application for Readmission to the Radiography 73-75
Program
Appendix B: NCR Publication 76-83
Appendix C: Form Letter for Voluntarily Declaring Pregnancy 84
Form Letter for Withdrawal of Pregnancy Declaration 85
Appendix D: Course Grade Appeal 86-90
Appendix E: Grievance Procedure 91-92
Appendix F: Exceeding Radiation Dose 93-94
4
WELCOME LETTER
To the Prospective Radiologic Technologist Student:
We are pleased that you are considering becoming a member of the Radiologic Technology
Program at Houston Community College Coleman Health Science Center. If you have already
been accepted to the program, we congratulate and welcome you. We are very proud of the
program and the achievements of its graduates.
This Handbook has been written to provide you with program guidelines and helpful
information. Since this experience will probably be a very different learning experience than
any you have encountered before, we expect you to become familiar with all college program
policies. These policies encompass the professional, clinical, and academic behaviors that are
to be explicitly followed. It is your responsibility to become knowledgeable of this Handbook
contents. You will sign a statement verifying that you do understand the contents of the
Handbook, and that you do agree to abide by the guidelines set forth within. This form will be
retained in your permanent file for the duration of your participation in the program.
During your Radiology education, the program faculty will strive to prepare you to become a
professional radiologic technologist who is eligible to sit for the national certification
examination. This healthcare career program is one which takes much time and dedication on
your part. Realizing this, we would like to wish you all success as you make a commitment to
yourselves and this course of study for the next two years. In addition, let us offer our
assistance in helping you make these upcoming years fulfilling ones. We believe that your
graduation from the Radiologic Technology Program and your successful career in the field
will be the reward for all your efforts.
Sincerely,
Christopher Allen Daza
Christopher Allen Daza, MEd, RT(R) (CT), Program Director
5
HOUSTON COMMUNITY COLLEGE
COLEMAN COLLEGE FOR HEALTH SCIENCES
RADIOGRAPHY PROGRAM
ORGANIZATIONAL CHART

6
PROGRAM DESCRIPTION
The program of Radiography at the Houston Community College System (HCCS) is a two-
year (six semesters) program with graduates receiving an Associate Degree in Applied
Science (AAS). Program graduates are eligible to sit for the certification examination given by
the American Registry of Radiologic Technologists (ARRT). The program is accredited by the
Joint Review Committee on Education in Radiologic Technology (JRCERT), and the Texas
Coordinating Board of Higher Education (THECB). The Standards for an Accredited
Educational Program in Radiologic Sciences, adopted by the JRCERT, can be found in the
Department Chair’s office. Copies will be made available upon request. HCCS is accredited
by the Southern Association of Colleges and Schools (SACS). A copy of this handbook can be
found on-line at https://www.hccs.edu/programs/areas-of-study/health-sciences/radiography/
NON-DISCRIMINATION POLICY
HCC is committed to providing an educational climate that is conducive to the personal and
professional development of everyone. Students should be aware that discrimination and/or
other harassment based upon race, color, religion, sex, gender identity, gender expression,
national origin, age, disability, sexual orientation, and veteran status is prohibited by HCC
policy.
MISSION STATEMENT
Consistent with the mission of Houston Community College, the faculty of the Radiography
Program is committed to providing quality instruction to educate competent entry level
radiographers to meet the needs of the ever changing, diverse, and multi-cultural health care
community. The Program strives to develop within all students, an appreciation and desire for
the continued quest for knowledge, lifelong learning, integrity, and community-mindedness.
PROGRAM GOALS
The goals of the program include:
1. Upon completion of the program, the graduate will satisfactorily demonstrate the following
skills in radiography:
a. Clinical Performance and Competency
b. Communication Skills
c. Problem Solving Capabilities and Critical Thinking
2. Upon completion of the program, a minimum of 90 percent of the graduates will be
successful on the national credentialing examination
3. 80 percent of the graduates seeking employment in Radiography will be employed
within one year.
4. 75 percent of the students admitted to the program will complete the two-year
curriculum

7
PROGRAM BENCHMARKS
The program has set the following benchmarks:
1. A pass rate on the ARRT exam of 90% for first time test takers.
2. A job placement rate of 80% within one year of graduation.
3. A program completion rate of 75% per year.
The Radiography Program at Houston Community College is quite intense and requires
many hours of study to be successful. All radiography courses are scheduled Monday
through Friday during daytime hours. At designated times within the program, with
proper evaluation and approval by the clinic coordinator, students may be scheduled on
a limited evening clinical rotation.
To assure patient safety in the clinical area, student radiographers must perform the
following essential skill sets:
1. Read and write at a college level. The student must be able to communicate
effectively in verbal and written aspects of the English language.
2. Perform basic mathematical functions.
3. Be able to function within a high stress hospital environment and in
emergency situations be able to respond rapidly and accurately.
4. Be able to use independent judgment in decision making with patient care
and technical procedures.
5. Demonstrate interpersonal skills with classmates and the staff of clinical
education centers.
6. Be clean and neat in personal appearance for dress and personal hygiene.
7. Demonstrate self-motivation in accomplishing personal goals within the
program.
8. Follow college and program policies and procedures as outlined in Student
Handbook and HCC College Catalog.
EXPECTED OUTCOMES
The radiographer is an important member of the health care team. The Radiography
Program at Houston Community College has identified the following expected
outcomes, which represent entry-level skills for the radiologic technologist. Upon
completion of the program, the graduate should be able to meet the following:
1. Use verbal and written communication effectively.
2. Apply knowledge of anatomy, physiology, positioning, radiographic
techniques, and imaging systems.
3. Calculate and determine exposure factors to achieve optimum radiographic
techniques with minimum radiation exposure to the patient.
4. Evaluate radiographic images for appropriate positioning and image quality.
5. Apply the principles of radiation protection for the patient, self, and others.
6. Provide quality patient care, safety, and comfort.
7. Recognize emergency patient conditions and respond appropriately.
8. Evaluate the performance of radiographic systems, recognize, and
understand the safe limits of equipment operation and report malfunctions to
the proper personnel.
8
9. Apply critical thinking skills to adapt the technical performance of
radiographic procedures to patient ability and situation.
10. Process and annotate digital radiographic images.
11. Apply principles of proper body mechanics while positioning and transferring
patients.
12. Demonstrate knowledge and skills relating to quality assurance of images
and equipment operation.
13. Demonstrate professional working standards with patients, hospital staff and
administrators.
PROGRAM ROLES DEFINED
Program Director
Duties include:
ï
Organize, administer, review, and assure program effectiveness
ï
Evaluate and assure clinical education effectiveness
ï
Maintain current knowledge of the professional discipline and educational
methodologies through professional development
ï
Develop and maintain the program’s master plan of education
ï
Coordination development, and revision of course descriptions and objectives
ï
Develop, coordinate, and conduct ongoing program evaluation through outcome
Assessment education
ï
Actively coordinate procedures required to maintain programmatic accreditation
ï
Periodically meet with faculty, clinical instructors, staff, and administrators
ï
Contribute to the formulation of the program budget
ï
Facilitate the program Advisory Committee
ï
Provide student guidance and academic advising
ï
Establish appropriate communication and feedback for student concerns
ï
Maintain professional certification
ï
Oversee fair and just enforcement of program policies
ï
Maintain professional certification
Clinical Coordinator
Duties include:
ï
Correlate clinical education with didactic education
ï
Evaluate and assure clinical education effectiveness through regularly scheduled
visits to all clinical settings
ï
Instruct students and evaluate student clinical skills
ï
Contribute to the development, implementation, and evaluation of program goals
and objectives participating in accreditation and assessment process
ï
Provide student guidance and academic advising
ï
Establish and enforce clinical policies and procedures
ï
Exhibit a positive attitude toward students and clinical process
ï
Coordinate and maintain all clinical records in a safe and confidential manner
ï
Meet regularly with program faculty to document student clinical progress
ï
Coordinate annual Adjunct Clinical Instructor meeting
9
ï
Maintain current knowledge of discipline through professional development
ï
Serve on College committees
ï
Participate on Program’s Advisory Committee
ï
Maintain professional certification
ï
Establish standard methods for evaluation for student clinical performance
ï
Acts as a liaison and maintain open communication between clinical sites and
the program
Full Time Faculty
Duties include:
ï
Review, and assure program effectiveness
ï
Coordinate, prepare and maintain revision of course descriptions and objectives
ï
Exhibit a positive attitude toward students, faculty and administration promoting
cooperation and mutual benefit
ï
Participate and support the program director in the accreditation and assessment
process
ï
Periodically meet with faculty, staff, and administrators
ï
Participate on Program’s Advisory Committee
ï
Provide student guidance and academic advising
ï
Perform clinical progress and competency evaluations for each student assigned to
the appointed clinical site
ï
Provide regular feedback to the Clinical Coordinator and Program Director to
communicate student progress, and/or strengths and weaknesses
ï
Serve on College committees
ï
Maintain current knowledge of discipline through professional development
ï
Establish appropriate communication and feedback for student concerns
ï
Oversee fair and just enforcement of program policies
ï
Maintain professional certification
Adjunct (PT) Faculty
Duties include:
ï
Demonstrates current knowledge of program goals, clinical objectives, and
clinical evaluations and online clinical evaluation system
ï
Provide students with appropriate and adequate clinical instruction
ï
Assure students have appropriate and adequate clinical supervision identified
by direct and indirect policies with documented student competencies
ï
Perform clinical progress and competency evaluations for each student assigned
to the appointed clinical site
ï
Provide regular feedback to the Clinical Coordinator and Program Director to
communicate student progress, and/or strengths and weaknesses
ï
Exhibit a positive professional attitude toward students learning and teaching
process
ï
Maintain professional certification
ï
Assist with maintaining effective well documented student clinical records in a
timely manner
ï
Participates in faculty program meetings
ï
Oversee and monitor student competencies
10
ï
Communicate with the in a timely manner Clinical Coordinator pertinent
information (competency forms, behavioral concerns and evaluations, attendance
reports, disciplinary records, radiation badge readings, grades, etc.)
ï
Maintains availability to students and program faculty
ï
Participates in the Adjunct Clinical Instructors meetings
ï
Supports and promotes program goals and ideas
ï
Acts as a liaison between the students and the Clinical Coordinator
ï
Keeps current with professional certification and state license
Clinical Staff (Clinical Preceptor)
Duties include:
ï
Understand the clinical competency system
ï
Understand requirements for student supervision
ï
Evaluate students’ clinical competency
ï
Meet with Clinical Instructors to maintain knowledge of program policies,
procedures and student progress
ï
Maintains current with professional certification and state license

11
Institution Name:
Houston Community College
Program Type: Radiography
Degree Type:
Associate of Applied Science
Program Effectiveness Data
The following is the most current program effectiveness data. Our programmatic accreditation agency, the Joint Review Committee on
Education in Radiologic Technology (JRCERT), defines and publishes this information. The information can be found directly on the
JRCERT webpage.
Credentialing Examination: The number of students who pass, on the first attempt, the American Registry of Radiologic
Technologists (ARRT) certification examination, or an unrestricted state licensing examination, compared with the number of
graduates who take the examination within six months of graduation. The five-year average benchmark established by the
JRCERT is 75%.
Credentialing Examination Rate
number passed on 1
st
attempt divided by
number attempted within 6 months of
graduation
Year
Results
Year 1 - 2018
29 out of 29
100
%
Year 2 - 2019
27 out of 28
96
%
Year 3 - 2020
26 out of 30
87%
Year 4 - 2021
32 out of 36
89%
Year 5 - 2022
28 out of 28
100%
Program 5-Year Average
142 out of 151
94%
Job Placement: The number of graduates employed in the radiologic sciences compared to the number of graduates actively
seeking employment in the radiologic sciences within twelve months of graduating. The five-year average benchmark established
by the JRCERT is 75%.
Job Placement Rate
number employed divided by number actively
seeking employment within 12 months of
graduation
Year
Results
Year 1 - 2018
27 out of 31
93
%
Year 2 - 2019
27 out of 29
96
%
Year 3 - 2020
27 out of 29
93
%
Year 4 - 2021
30 out of 31
97%
Year 5 - 2022
28 out of 28
100%
Program 5-Year Average
139 out of 148
94%
Program Completion: The number of students who complete the program within the stated program length. The annual
benchmark established by the program is 75%.
Program Completion Rate
number graduated divided by number
started the program
Year
Results
Year 1 -
2022
28 out of 49
57%
Annual Completion Rate

12
CHANGE OF PERSONAL INFORMATION
Each student is responsible for providing the HCC and the program with information
regarding a change in postal address, e-mail address, phone number and name change.
This information is important in case of an emergency during the time the student is part of
the program. This also assists in mailing or e-mailing any correspondence and post graduate
information to each alumni.
PARKING
Students are responsible for any parking fees required when attending didactic and
clinical education classes. Parking contracts (for on campus parking) are available. The
monthly parking cost is approximately 126.65. (Additional fees may apply)
SIGN up for parking in 3 easy steps:
1. Go online to: https://www.tmc.edu/parking/contract-parking/
2. Click “Create New User” and follow the steps to select your preferred parking location.
3. Receive your parking card either in person at 2450 Holcombe Blvd. in 2 business days
or mailed to you in 5-9 business days.
HEALTH INSURANCE
Students are responsible for carrying their own health insurance. Treatment for injuries
incurred in class, lab, or clinic is the responsibility of the student.
MEDICAL LIABILITY INSURANCE
All students enrolled in the program are required to purchase medical liability insurance
at the time of registration. The amount will be charged as a special fee coded under
clinical practicum courses at registration. The insurance is necessary for each student's
protection in the case a patient or employee of the hospital is injured when under the
student's care. The insurance fee is paid each semester the student is enrolled in
clinical practicum courses. The cost is approximately $13.00/semester when students
are assigned to clinic.
RADIATION MONITOR FEE
All students in the Radiography Program are required to wear a radiation detection
badge during the two years enrolled in the program. This fee is also paid at registration
and is $12.00/semester when students are assigned to clinic.
REGISTRATION/ENROLLMENT PROCESS
All students at Houston Community College must register and pay for classes prior to
the beginning of each semester. All fees are to be paid prior to attending classes.
Students will register themselves in the first semester of the program, but all
subsequent semesters, the program will register students. Radiography students are
not allowed to register late.
1. Any student not registered in a Radiography class on the first day will be sent
to the registrar’s office, counted absent and readmitted to class with proof of
registration.
2. Students will not be allowed to attend either didactic or clinical
education courses unless they are registered prior to/on the first day of
class. (No exceptions)

13
ADA CONSIDERATIONS
Qualifying individuals under the Americans with Disabilities Act (ADA) guidelines who require
reasonable accommodations should report to the ADA counselor. The ADA counselor for the
Coleman College is located on the 1st floor in the Learning Success Center (LSC). Faculty will
adhere to ADA accommodations from the point at which those accommodations are received from
the student. (See Page 29 for Complete Details)
ADVISEMENT
Once students are enrolled in the program, they are assigned a college advisor.
Students are free to contact their advisor, or any program instructor, with whom they
feel comfortable when they deem necessary. Students enrolled in the program will also
have a designated radiography faculty advisor.
STUDENT SERVICES
College services (financial aid, registration, counseling, etc.) are provided at the
Coleman College on the 1
st
Floor. The bookstore is located at the West Loop Center,
5601 West Loop South Houston, TX 77081. Phone#: 713-718-7930
ACADEMIC SUCCESS CENTER
The Academic Success Center assists students enrolled in the HCC-Coleman Campus
for Health Sciences through a variety of means: one on one academic development
meetings with ASC-Coordinator, tutoring, workshops, career development, test-friendly
environment, and respite activities. It is located on the 1st floor in the Student Success
Center.
COLLEGE IDENTIFICATION BADGE
HCCS will provide the students with I.D. badges at no cost to the students. The I.D. is
to be worn on campus and at clinic. Students should report to The Center, located on
the first floor of the Coleman Campus to obtain a student I.D. A paid tuition receipt is
required to obtain a badge.
LEAD MARKERS
Lead markers will be required of each student. They are to be purchased. It is
recommended that you initially purchase two (2) sets. The cost is between $10-20 per
set. It is the student’s responsibility to maintain these markers.
RADIOGRAPHY PROGRAM STUDENT ORGANIZATION
Faculty member Paul Pham, Shawna Francis, and Nam Nguyen serve as coordinators
for the Radiography Student Organization/Council. They will work to organize and
advise students on activities.

14
CONFIDENTIALITY STATEMENT
In compliance with the Family Educational Rights and Privacy Act of 1974", the
following types of student information may be released to the public unless the student
desires to withhold all or any portion of it: student’s name, address, email address,
phone number, date, and place of birth, major, participation in activities and sports,
semesters enrolled degrees, certificates, enrollment status and previous institutions
attended. Any student objecting to the release of all or any portion of such information
must notify the admissions office in writing as soon as possible during each semester of
enrollment.
Release of any additional information pertaining to the student records must be
authorized by the student (i.e., grades, transcripts). The student’s parents may
authorize release of information if the student is younger than 18 years of age and a
dependent as defined by the IRS
Program files, which are maintained within the campus office or the clinical education
settings, are kept in locked drawers or file cabinets. Access to these records, is limited
to the Clinical Instructor and Program Faculty of the campus or clinical education
setting.
ADVISORY COMMITTEE
The Advisory Committee is designed to discuss current trends in health care, curriculum
revision, supports the mission, review goals and outcomes of the program, and issues
directly related to the Radiography and Computed Tomography programs. In addition,
The Advisory Committee also serves as a forum to discuss student related issues and
to provide the long-term planning of the program, evaluation, and give input on key
issues occurring in the field of radiography.
The membership composition includes: two (2) currently enrolled students from first
year and two (2) second year class, representatives from clinical affiliates,
radiography faculty members, and medical and/or radiological professions. The
Program Advisory Committee will have meetings twice during each academic year
(Spring and Fall semester). Additional meetings will be scheduled when a need is
indicated.

15
RADIOGRAPHY PROGRAM FACULTY
Christopher Daza, MEd, RT(R) (CT): Program Director
A.A.S. Houston Community College, B.S.R.S., Midwestern State University, MEd, University of Houston
M. Theresa Lobrin, M.H.A., RT(R) (CT): Clinical Coordinator
A.A.S. Houston Community College, B.S. Capella University-Minneapolis, MN., M.H.A Capella University
Roger Bumgardner, MPH, RT(R) (N) (CT) (CV): Clinical Instructor-Memorial Hermann
TMC, Methodist Bone and Joint & Methodist Pin Oak
B.S. Northwestern State University – Natchitoches, LA, M.P.H. University of Texas – Houston, TX
Shawna Francis, BS, RT(R) (CT): Clinical Instructor – Texas Children’s West, Methodist Bone
and Joint West
A.A.S. Houston Community College, B.S.R.S – Midwestern State University
Nam Nguyen, BS, RT(R) (CT): Clinical Instructor – HCA North Cypress
A.A.S. Houston Community College, B.S.R.S – Midwestern State University
Paul Pham, MBA, RT(R) (CT): Clinical Instructor – HCA West, Kelsey Villages
A.A.S. Houston Community College, M.B.A. - Columbia Southern University
Denisse Salazar, BS, RT(R): Clinical Instructor – Texas Children’s West Campus
A.A.S. Houston Community College, B.S. University of Texas, M.D. Anderson-Houston, TX.
ADJUNCT FACULTY
Latasha Andrews, BS, RT(R) (M): Clinical Instructor
A.A.S. Delgado Community College, B.S. – Boise State University
Mark Conran,BS, RT(R), EMT: Clinical Instructor
A.A.S. Houston Community College- Houston, TX. B.S.R.S., Midwestern State University
Patricia Gow, RT(R): Clinical Instructor
A.A.S. Houston Community College- Houston, TX.
Jose Jaimes, BS, RT(R): Clinical Instructor
A.A.S. Houston Community College, B.S. - University of Houston Downtown
Kioyka Jones, BS, RT(R) (MR): Clinical Instructor
A.A.S. Lone Star College – Montgomery, BS – Pima Medical Institute
Rhonda Marcel, BS, RT(R): Clinical Coordinator
A.A.S. Houston Community College, B.S. University of Memphis – Memphis, TN,
Gilbert Micu, RT(R): Clinical Instructor
A.A.S. Houston Community College- Houston, TX.
Mailing address for faculty of the HCC Coleman College for Health Sciences:
HCC Coleman College for Health Sciences – Radiography
1919 Pressler Street
Houston, Texas 77030

16
CLINICAL AFFILIATES
1) HCA Houston Northwest Medical Center 281-440-2504
710 Cypress Creek Pkwy
Houston, TX 77090
Clinical Preceptor: Sara Mikolas
2) HCA Houston Healthcare North Cypress 832-912-3575
21214 Northwest Freeway
Cypress, TX 77429
Clinical Preceptor: Steve Montes
3) HCA Houston Healthcare West 281-588-8148
12141 Richmond Avenue
Houston, TX 77082
Clinical Preceptor: Erica Garcia
4) Houston Methodist Orthopedics – Pin Oak 713-441-8400
5505 W. Loop South Freeway
Houston, TX 77835
Clinical Preceptor: Adjunct Faculty
5) Houston Methodist Orthopedics – Spring Valley 832-522-8721
9090 Katy Freeway, Suite 200
Houston, TX 77024
Clinical Preceptor: Adjunct Faculty
6) Houston Methodist Orthopedics – TMC 713-790-1818
6550 Fannin St. Suite 2600 ext. 56515
Houston, TX 77030
Clinical Preceptor: Jaike Lukose
7) Houston Methodist Orthopedics – West 832-522-8290
18400 Katy Freeway, Suite 200
Houston, TX 77094
Clinical Preceptor: Neeta Patel
8) Kelsey-Seybold (Cypress) Clinic 713-442-4000
13105 Wortham Center Dr.
Houston, TX 77065
Clinical Preceptor: Cathy Johnson
9) Kelsey-Seybold (Fort Bend) Clinic 713-442-9243
11555 University Blvd
Sugarland, TX 77478
Clinical Preceptor: Tracy Anderson

17
10) Kelsey-Seybold (Memorial Villages) Clinic 713-442-6421
1001 Campbell Rd
Houston, TX 77055
Clinical Preceptor: Annette Hernandez
11) Kelsey-Seybold (Spring) Clinic 713-442-1700
15655 Cypress Woods Medical Dr., Suite 100
Houston, TX 77014
Clinical Preceptor: Eddie Sweeten
12) Memorial Hermann Greater Heights Hospital 713-867-3341
1635 North Loop West
Houston, TX 77008
Clinical Preceptor: Christina Soto
13) Memorial Hermann Hospital – Southwest 713-456-5000
7600 Beechnut St.
Houston, TX 77074
Clinical Preceptor: Adjunct Faculty
14) Memorial Hermann Orthopedic & Spine Hospital 713-314-4444
5410 W Loop S
Bellaire, TX 77401
Clinical Preceptor: Adjunct Faculty
15) Memorial Hermann – Texas Medical Center 713-704-3990
6411 Fannin
Houston, TX 77030
Clinical Preceptor: Russell Booth
16) Michael E Debakey VA Medical Center 713-791-1414
2002 Holcombe Blvd. ext. 4516
Houston, TX 77030
Clinical Preceptor: Michael Daza
17) River Oaks Hospital and Clinics 713-980-7900
4200 Twelve Oaks Pl
Houston, TX 77027
Clinical Preceptor: Adjunct Faculty
18) St. Joseph Medical Center 713-756-4138
1401 St. Joseph Parkway
Houston, TX 77002
Clinical Preceptor: Angela Allen
18
19) St. Lukes Episcopal Hospital 832-355-2979
6720 Bertner Ave
Houston, TX 77030
Clinical Preceptor: Adjunct Faculty
20) Texas Children’s Hospital 832-824-5353
6621 Fannin Street
MC-2-2521
Houston, TX 77030
Clinical Preceptor: Avis Wilson
21) Texas Children’s Hospital – West Campus 832-227-1219
18200 Katy Freeway
Houston, TX 77030
Clinical Preceptor: Juliette Lee
22) Texas Orthopedic Hospital 713-799-8600
7401 Main Street
Houston, TX 77030
Clinical Preceptor: Thomas Kottor

19
RADIOGRAPHY PROGRAM CURRICULUM
2023-2025
PREREQUISITE SEMESTER
SEMESTER HOURS
MATH 1314: College Algebra
3
ENGL 1301: English Composition I
3
BIOL 2301 or 2101: Anatomy and Physiology
4
EDUC 1300: Student Success and Career Development 3
*****************************************************************************
FALL FIRST SEMESTER
RADR 1303: Patient Care
3
RADR 1411: Basic Radiographic Procedures
4
RADR 1160: Clinical Practicum I
1
RADR 1301: Introduction to Radiography
3
XXXXX3XX: Approved Fine Arts Elective
3
SPRING SECOND SEMESTER
RADR 2401: Intermediate Radiographic Procedures
4
RADR 1266: Clinical Practicum II
2
RADR 1313: Principles of Radiographic Imaging I
3
SUMMER THIRD SEMESTER* 8 weeks
RADR 2331: Advanced Radiographic Procedures
3
RADR 2260: Clinical Practicum III
2
FALL FOURTH SEMESTER
RADR 2333: Advanced Medical Imaging
3
RADR 2366: Clinical Practicum IV
3
RADR 2309 Radiographic Imaging Equipment
3
PSYC 2301: Introduction to Psychology or
SOCI 1301: Introduction to Sociology
3
SPRING FIFTH SEMESTER
RADR 2367: Clinical Practicum V
3
RADR 2217: Radiographic Pathology
2
RADR 2213: Radiation Biology & Protection
2
SUMMER SIXTH SEMESTER* 8 weeks
RADR 2335: Radiologic Technology Seminar
3
RADR 2167: Clinical Practicum VI
1
TOTAL
64 Total Credit Hour

20
CURRICULUM SEQUENCING
The basic plan of the curriculum encompasses the following steps:
a. Didactic instruction with lab experiences
b. Practicum testing on campus in procedures and image production
c. Working under the direct supervision of a qualified technologist in the clinic,
keeping a log of exams observed, participated in, repeated, and performed.
d. Competency testing in the clinic, with a minimum grade of 90%
e. Performing exams under indirect supervision
A. Students must be successful at each step to be able to proceed to the next step.
Students must pass a practical exam on campus before testing on the exam in
the clinic is allowed.
Students in the Radiography program are required to maintain a minimum
GPA of 2.0 (C average) to remain in the program and to qualify for
graduation. The grading scale for the Program is as follows:
Didactic Grading
Clinical Grading
A--Excellent
90% - 100%
A--Excellent
93% - 100%
B--Above average
80% - 89%
B—Above average
85% - 92%
C--Average
75% - 79%
C--Average
75% - 84%
D - Below Average
60% - 74%
D - Below Average
60% - 74%
F - Failure
Below 60%
F - Failure
Below 60%
Any grade below a "C" is considered unacceptable and will prevent the student from
progressing to the next semester. The grading scale has been set to indicate the
necessary proficiency level required for passing the certification examination given by
the American Registry of Radiologic Technologists (ARRT).
Failure of a course may result in dismissal from the program; however, this does not
mean that a student would be ineligible to register for other courses at Houston
Community College. Students may apply for readmission to the program, but they are
not guaranteed a space in the next class. If the student's GPA falls below 2.0, he/she
will not be readmitted to the program. Other factors that would make a student ineligible
for readmission include scholastic dishonesty, unprofessional behavior in the
classroom/clinical setting, removal from a clinical sight and documentation from a
clinical affiliate asking for removal or non-reassignment of a student, failure/refusal to
meet with Department Chair/Program Officials. The student has the right to file a grade
appeal. (See Program Policy, Grade Appeal [p.76-81] and Appendix D)
FINAL GRADE OF FX
Students who stop attending class and do not withdraw themselves prior to the
withdrawal deadline may either be dropped by their professor for excessive absences or
be assigned the final grade of “FX” at the end of the semester. Students who stop
attending classes will receive a grade of “FX”, compared to an earned grade of “F”
which is due to poor performance. Logging into a DE course without active participation

21
is seen as non-attending. Please note that HCC will not disperse financial aid funding
for students who have never attended class. Students who receive financial aid but fail
to attend class will be reported to the Department of Education and may have to pay
back their aid. A grade of “FX” is treated exactly the same as a grade of “F” in terms of
GPA, probation, suspension, and satisfactory academic progress
A. Eligibility to sit for the certification examination given by ARRT is
predicated on the completion of the course work in the program and the
graduate must have earned his/her associate degree. No student will be
permitted to sit for the examination unless all clinical education and all
academic course work is completed.
B. Each semester is a prerequisite for subsequent semesters. All courses must
be completed in the semester before a student may continue in the program.
C. All prerequisites must be satisfied before entering a class. Course prerequisites
are printed in the college catalog.
D. Grades will be posted at the end of each semester. Students will be able to
access their grades online after the end of the semester. Students should
follow the instructions on the hccs.edu website for accessing grades.
E. STUDENTS WHO RECEIVE A “D” or an "F" IN ANY RADIOGRAPHY
COURSE WILL NOT BE PERMITTED TO CONTINUE IN THE PROGRAM. If a
student earns a “D” or an "F" in an academic course in the degree plan, which
causes his/her GPA to fall below a 2.0, the student will be withdrawn from the
program and may apply for readmission. Readmission is not guaranteed.
F. RADR 2335 is the Capstone Course for the program. It is taught as a seminar
course designed to evaluate student’s knowledge of Radiography as they
prepare to graduate from the program. It is an essential course to prepare
students to apply for the ARRT examination. It is the last course to be
completed in the program.
The Radiography Program is considered a full-time Program. Although there may be
some semesters where the credit hour load is less than 12 hours, the amount of time
spent in class and clinic averages 25 - 30 hours per week.
All Radiography students are committed to a six-semester (two-year) program.
Semester breaks will be observed as they are by other HCC students and the HCC
systems. During these breaks, students will be excused from classroom and clinic
schedules. Some classes may need to be made-up after the holiday and will be
announced in the course calendar. Students must schedule personal time off after
all announced final exams.

22
Often, failure in the program is caused by a conflict between work and school. Both job
and scholastic performance suffers. The Program discourages students from working in
the capacity of radiographers prior to graduation. Until the program is completed,
students do not have all the necessary skills to perform the tasks required of a
radiographer. The policy of the program is to counsel students who appear to have a
conflict between academic and non-academic life. Students may be sent an Early Alert
if a student continues to exhibit unacceptable behaviors, the student will be placed on
probation for the remainder of the semester. The following are examples of behaviors
that would warrant a counseling session:
1. Poor clinic evaluations
2. Patterned and/or excessive tardiness
3. Decline in academic and/or clinical performance
4. Unwillingness to accept feedback
5. Disrespect for clinic/class/departmental faculty and/or students
DESCRIPTION OF SEMESTERS
First semester
In the first semester (Fall), students are enrolled in RADR 1303 Patient Care , RADR
1411 Basic Radiographic Procedures, RADR 1301 Introduction to Radiography and
RADR 1160 Clinical Practicum I *(see syllabi for complete course content). These four
courses complement each other in a way that prepares the students for an introduction
to the clinical environment. RADR 1303 is a lecture course. Topics include patient
assessment, infection control procedures, emergency and safety procedures,
communication and patient interaction skills and basic pharmacology. Basic radiation
protection, medical ethics and legal issues will also be discussed. RADR 1411 is a
lecture/lab course. Students cover anatomy and positioning of the chest, abdomen, and
upper and lower extremities as well as body systems. Lab competency must be
achieved before a student can attend clinic. Students participate in positioning lab,
including practicums. RADR 1301 provides a general overview of the radiography field;
many topics will be discussed pertaining to radiography. RADR 1160 is the first clinical
experience. This clinical begins in the 5
th
week of the semester after basic patient care
skills, lab competency and positioning exposure has occurred. To receive a grade for
the course, a student must successfully competency test on One (1) exam. If the
student does not fulfill the requirement, they will receive an “F” in the course.
Second semester
In the second semester (Spring), students are enrolled in RADR 2401 Intermediate
Radiographic Procedures, RADR 1313 Principles of Radiographic Imagining and RADR
1266* Clinical Practicum II (see syllabi for complete course content). RADR 2401 is the
2
nd
anatomy and positioning course. Students are taught pelvis, hip, spine, thorax and

23
contrast exams. Body systems will also be taught. RADR 1313 is a lecture/lab course
where techniques and principles of imaging are covered. In RADR 1266, the student
must attempt/complete twelve (12) exams to receive a grade. If the 12 exams are not
completed in this semester (see RADR 1266 syllabus), an incomplete will be
recorded, and a Change of Grade form is prepared for the following semester. For the
grade to change, the student MUST complete the make-up exams in the following
semester.
The student performs chest and abdomen exams and competency tests on upper and
lower extremities. At any time, the instructor may require the student to repeat a
competency exam if continued competency is not demonstrated. Students are
evaluated by the clinical instructor and staff technologists at the clinical education
center. National and local society participation is highly encouraged in preparation for
participation in professional society events.
Third semester
In the third semester (Summer), the student is enrolled in RADR 2331 Advanced
Radiographic Positioning and RADR 2260 Clinical Practicum III* (see syllabi for
complete course content). In RADR 2331, students will be taught positioning for skull
and facial region, pediatric, trauma and mobile radiography. In RADR 2260, the student
must attempt/complete eight (8) exams to receive a grade. If the 8 exams are not
completed in this semester (see RADR 2260 syllabus), an incomplete will be recorded,
and a Change of Grade form is prepared for the following semester. For the grade to
change, the student MUST complete the make-up exams in the following semester.
Students can competency test on upper and lower extremities, spine, and contrast
studies. Students may rotate through ancillary imaging areas. The students are
required to perform those exams in which competency were demonstrated.
Fourth semester
In the fourth semester (Fall), students are enrolled in RADR 2333 Advanced Medical
Imaging, RADR 2309 Radiographic Imaging and Equipment and RADR 2366 Clinical
Practicum IV* (see syllabi for complete course content). RADR 2333 provides
instruction in specialized imaging modalities. covers study of the equipment and
physics of x-ray production, basic x-ray circuits and relationship of equipment
components to the imaging process.. In RADR 2366, the student must
attempt/complete thirteen (13) exams to receive a grade. If the 13 exams are not
completed in this semester (see RADR 2366 syllabus), an incomplete will be
recorded, and a Change of Grade form is prepared for the following semester. For the
grade to change, the student MUST complete the make-up exams in the following
semester. Students can competency test on head and neck procedures in addition to
the extremities, thorax, entire spine, and contrast studies. Students may rotate
through ancillary imaging areas.
Fifth semester
In the fifth semester (Spring), students are enrolled in RADR 2217 Radiographic

24
Pathology, RADR 2213 Radiation Protection & Biology and RADR 2367 Clinical
Practicum IV* (see syllabi for complete course content). RADR 2217 presents the
disease process and common diseases and their radiologic appearance. In RADR
2213, students study the effects of radiation exposure on biological systems and are
taught methods for measuring and monitoring radiation as well as how to protect
personnel and patient from excessive exposure. In RADR 2367, the student must
attempt/complete thirteen (13) exams to receive a grade. If the 13 exams are not
completed in this semester (see RADR 2367 syllabus), an incomplete will be recorded,
and a Change of Grade form is prepared for the following semester. For the grade to
change, the student MUST complete the make-up exams in the following semester.
Students can competency test in all previous areas.
Sixth semester
In the sixth semester (Summer), students are enrolled in RADR 2335 Radiologic
Technology Seminar and RADR 2167 Clinical Practicum VI*. These are considered
capstone courses (see syllabi for complete course content). In RADR 2335, the student
will be regularly assessed on their competence of the didactic portion of this program.
This course also reviews the requirements for the American Registry of Radiologic
Technologists (ARRT) exam, and the (TMB) Texas Medical Board (MRT) license.
Recruiters, area human resources personnel, as well as others may be invited to do
presentations for the class. In RADR 2167, the student is required to perform four
(4) competencies, to complete the total required ARRT mandatory and elective
competencies, as well as four (4) additional terminal competencies as decided
by the clinical instructor. Competency exams may include a variety of exams covered
in the Radiography courses. To receive a grade for the course, a student must
successfully competency test on all exams required in this semester. If the student
does not fulfill the requirement, they will receive an “F” in the course.
Incomplete grades will not be given in the sixth semester.
*The Grading Scale for all clinical practicum courses are as follows:
A = 93 - 100
B = 85 - 92
C = 75 - 84
D = 60 - 74
F = Below 60
NOTE: The exact number of clinical competencies required in each clinical semester may change
and will be most accurately reflected in the course syllabus.
COURSE EVALUATIONS
Once a semester, all students are requested to complete course evaluations (EGLS3) for each
class in which they are enrolled. Students are invited to use constructive feedback in completing
the evaluations so faculty can identify strengths and weaknesses in the course. Faculty does
not review the actual evaluations by the students, but receive a summary or an average of the
course ratings.

25
BOOK LIST
1
st
semester fall
RADR 1303 Patient Care and Ethics
Title: Introduction to Radiologic Sciences and Patient Care
Author: Adler/Carlton
Publisher: Elsevier/ Saunders /8
th
edition
ISBN: 9780323872201
RADR 1411, Basic Radiographic Procedures
Title: Textbook of Radiographic Positioning and Related Anatomy (Used for 3 semesters)
Author: Bontrager, K., Lampignano, J
P
ublisher
: E
lsevier
/
Mosb
y.
202
1/
10
th
edition
ISBN: 978-0-323-653671
RADR 1411, Basic Radiographic Procedures Workbook
Title: Radiographic Positioning and Related Anatomy Procedures Workbook
Author: Bontrager, K., Lampignano, J
P
ublisher
: E
lsevier
/
10
th
edition
ISBN: 978-0-323-694230
RADR 1301 Introduction to Radiography
Title: Introduction to Radiologic Technology
Author: William J. Callaway
Publisher: Elsevier
ISBN: 978-0-323-64339-9
RADR 1160 Clinical Practicum I (No textbook required)
2
nd
semester spring
RADR 1313 Principles of Radiographic Imaging I
Title: Radiographic Imaging & Exposure
Author: Terri L Fauber
Publisher: Mosby / 6th edition
ISBN: 978-0-323-661393
RADR 2401 Intermediate Radiographic Procedures
Title: Textbook of Radiographic Positioning and Related Anatomy
Author: Bontrager, K., Lampignano, J.
P
ublisher
: E
lsevier
/
Mosb
y.
2021
/1
0
th
edition
ISBN: 978-0-323-653671

26
RADR 1266: Clinical Practicum II (No textbook required)
3
rd
semester summer
RADR 2331 Advanced Radiographic Procedures
Title: Textbook of Radiographic Positioning and Related Anatomy
Author: Bontrager, K., Lampignano, J.
P
ublisher
: E
lsevier
/
Mosb
y.
2021
/1
0
th
edition
ISBN: 978-0-323-653671
RADR 2260: Clinical Practicum III (No textbook required)
4
th
semester fall
RADR 2309 Radiographic Imaging Equipment
Title: Essentials of Radiographic Physics
and Imaging
Author: Johnston,Fauber
Publisher: Mosby, 2020/3
rd
edition
ISBN: 9780323566681
RADR 2333 Advanced Medical Imaging (No textbook required)
RADR 2366: Clinical Practicum IV (No textbook required)
5th semester spring
RADR 2213 (spring) Radiation Biology & Protection
Title: Radiation Protection in Medical Radiography” (9th edition)
Authors: Mary Alice Statkiewicz Sherer, AS, RT(R), FASRT, Paula J. Visconti, PhD, DABR, E. Russell
Ritenour, PhD, DABR, FAAPM, FACR and Kelli Haynes, MSRS, RT(R)
Publisher: Elsevier/Mosby
ISBN: 9780323825030 Copyright: 2022
RADR 2217 Radiographic Pathology Title: Radiographic Pathology for Technologists, 8
th
edition
Author: Kowalczyk
Mosby/Elsevier
ISBN: 9780323791298
RADR 2367 Clinical Practicum V (No textbook required)

27
6
th
semester summer
RADR 2335 Radiologic Technology Seminar
Title: Online Rad Review Easy
Title: RADIOGRAPHY PREP
Author: DA Saia, McGraw Hill
ISBN: 978-1-269-86357-8
RADR 2167 Clinical Practicum VI (No textbook required)
The bookstore is located at the West Loop Center, 5601 West Loop South,
Houston, TX. 77081.

28
Health - Program Information
Name of Program: Radiography 2023 - 2025 2 years
Total Hours of Instruction: Contact Hours: 2400 Credit Hours: 64
DETAILED COST INFORMATION
Program Cost
In-District
Program Cost
Out-District
Program Cost
Out-State
Tuition, Lab Fee (s) & Recreation
Fee (s)
$6880
$13024
$21248
Distance Education Fee (s)
N/A
Books
1453.00
1453.00
1453.00
Exam or Testing Fee (s)
HESI Pre –Entry 100.00
HESI Pre –Entry 100.00
HESI Pre –Entry 100.00
Background/Drug screening Fee
94.00
94.00
94.00
CPR (AHA-BLS)
Varies
Varies
Varies
Yearly Renewal Background/Drug
screening Fee
56.00
56.00
56.00
Trajecsys (Online Clinical Record
System)
150.00
150.00
150.00
MyClinical Exchange - 1year
membership
39.50
39.50
39.50
Certification Fee (s)
ARRT Board 225.00
ARRT Board 225.00
ARRT Board 225.00
TMB State License & Fingerprint
TMB State Lic. 80.00
TMB State Lic. 80.00
TMB State Lic. 80.00
TMB Jurisprudence Exam
TMB 34.00
TMB 34.00
TMB 34.00
Uniform
325.00
325.00
325.00
Health Insurance
Varies
Varies
Varies
Meningitis
N/A
N/A
N/A
Immunization (s)
425.00
425.00
425.00
Parking
Varies
Varies
Varies
Other(s)
N/A
N/A
N/A
Total cost for Supplies
Itemize supplies
Lead Markers 2 sets at 25.00
50.00
50.00
50.00
Total Cost
$9,911.50
$16,055.50
$24,279.50

29
TECHNICAL
STANDARDS FOR
RADIOGRAPHY
The following standards are capabilities related to successful practice in the
Radiography profession. They are “non-academic” criteria and include physical
capabilities required of radiography students and radiography professionals.
Students should be aware that they must be able to meet these standards to
successfully complete the program. Please read each item carefully to determine if you
can meet each requirement.
Skills
Speaking — Talking to others to convey information effectively.
Active Listening — Giving full attention to what other people are saying, taking time to
understand the points being made, asking questions as appropriate, and not interrupting
at inappropriate times.
Operation and Control — Controlling operations of equipment or systems.
Service Orientation — Actively looking for ways to help people.
Coordination — Adjusting actions in relation to others' actions.
Monitoring — Monitoring/Assessing performance of yourself, other individuals, or
organizations to make improvements or take corrective action.
Operation Monitoring — Watching gauges, dials, or other indicators to make sure a
machine is working properly.
Social Perceptiveness — Being aware of others' reactions and understanding why they
react as they do.
Science — Using scientific rules and methods to solve problems.
Instructing — Teaching others how to do something.
Abilities
Oral Comprehension — The ability to listen to and understand information and ideas
presented through spoken words and sentences.
Oral Expression — The ability to communicate information and ideas in speaking so
others will understand.
Near Vision — The ability to see details at close range (within 6 to 20 feet); observe the
patient’s condition; read radiographic/imaging equipment; evaluate medical images for
appropriate positioning and image quality; ability to see fine lines; distinguish gradual
changes in blacks, grays, and whites.
Arm-Hand Steadiness — The ability to keep hand and arm steady while moving arm or
while holding arm and hand in one position.
Information Ordering — The ability to arrange things or actions in a certain order or
pattern according to a specific rule or set of rules (e.g., patterns of numbers, letters,
words, pictures, mathematical operations).
Problem Sensitivity — The ability to tell when something is wrong or is likely to go
wrong. It does not involve solving the problem, only recognizing there is a problem.

30
Control Precision — The ability to adjust the controls of a machine quickly and
repeatedly to exact positions.
Deductive Reasoning — The ability to apply general rules to specific problems to
produce answers that make sense.
Finger Dexterity — The ability to make precisely coordinated movements of the fingers
of one or both hands to grasp, manipulate, or assemble very small objects.
Multi limb Coordination — The ability to coordinate two or more limbs (for example, two
arms, two legs, or one leg and one arm) while sitting, standing, or lying down. It does not
involve performing the activities while the whole body is in motion.
Hearing Ability – The ability to respond to patient’s verbal inquiries; hear faint or muffled
sounds when the use of surgical masks is required; communicate with other personnel
involved in the care of the patient; initiate timely response to audible alarms and signals.
Work Activities
Assisting and Caring for Others — Providing personal assistance, medical attention,
emotional support, or other personal care to others such as coworkers, customers, or
patients.
Getting Information — Observing, receiving, and otherwise obtaining information from
all relevant sources.
Performing for or Working Directly with the Public — Performing for people or dealing
directly with the public.
Updating and Using Relevant Knowledge — Keeping up-to-date technically and
applying new knowledge to your job.
Controlling Machines — Using either control mechanisms or direct physical activity to
operate machines.
Handling and Moving Objects — Using hands and arms in handling, installing,
positioning, and moving materials, and manipulating things. Pull and push heavy objects
Interacting with Computers — Using computers and computer systems to program
enter data, or process information.
Communicating with Supervisors, Peers, or Subordinates — Providing information to
supervisors, co-workers, and subordinates by telephone, in written form, e-mail, or in
person.
Performing General Physical Activities — Performing physical activities that require
considerable use of your arms and legs and moving your whole body, such as climbing,
lifting, balancing, walking, stooping, and handling of materials. Must be able to lift 25
pounds for short distances. Reach equipment at heights greater than 6 feet. Walk to
various locations for portable procedures. Standing unassisted for long periods of time.
Able to have enough strength to transfer and position patients and to move and operate
equipment such as stretchers and wheelchairs.
Documenting/Recording Information — Entering, transcribing, recording, storing, or
maintaining information in written or electronic/magnetic form.

31
Work Styles
Concern for Others — Job requires being sensitive to others' needs and feelings and
being understanding and helpful on the job.
Attention to Detail — Job requires being careful about detail and thorough in completing
work tasks.
Dependability — Job requires being reliable, responsible, and dependable, and fulfilling
obligations.
Self-Control — Job requires maintaining composure, keeping emotions in check,
controlling anger, and avoiding aggressive behavior, even in very difficult situations.
Cooperation — Job requires being pleasant with others on the job and displaying a
good-natured, cooperative attitude.
Integrity — Job requires being honest and ethical.
Stress Tolerance — Job requires accepting criticism and dealing calmly and effectively
with high stress situations.
Initiative — Job requires a willingness to take on responsibilities and challenges.
Adaptability/Flexibility — Job requires being open to change (positive or negative) and
to considerable variety in the workplace.
Achievement/Effort — Job requires establishing and maintaining personally challenging
achievement goals and exerting effort toward mastering tasks.
Sources:
Radiologic Technologists Bureau of Labor Statistics, U.S. Department of Labor.
Occupational Outlook Handbook, 2012-2013 Edition
American Registry of Radiologic Technologists (ARRT), 1255 Northland Dr., St. Paul,
MN 55120-1155. Phone: (651) 687-0048.
American Society of Radiologic Technologists (ASRT), 15000 Central Ave. SE,
Albuquerque, NM 87123-3917. Phone: (800) 444-2778. Fax: (505) 298-5063.
ARRT STANDARDS OF ETHICS (American Registry of Radiologic Technologists)
This Code shall serve as a guide through which Radiologic Technologists may evaluate
their professional conduct as it relates to patients, colleagues, other members of the
medical care team, health care consumers, and employers. The Code is intended to
assist radiographers in maintaining a high level of ethical conduct.
For the ARRT Code of Ethics, see the ARRT Standards of Ethics

32
ASRT Scholarships
The American Society of Radiologic Technologists offers 2 scholarships with application
deadlines on or around February 1
st
. Applicants must be currently enrolled in a
Radiologic Technology program maintaining a 3.0 or above GPA in the Radiography
Course work. They must be a United States Citizen, national or permanent resident
and evidence financial need.
The website for ASRT is www.asrt.org
The Jerman-Cahoon Student Scholarship
www.asrt.org/foundation/jerman_cahoon.htm
The Royce Osborn Minority Student Scholarship
www.asrt.org/foundation/royce_osborn.htm
There are scholarships available through the HCC Foundation. Students can apply for
these scholarships online.
Additionally, students may apply for PELL Grants and other forms of Financial Aid
offered through the HCCS Financial Aid Office.
Information pertaining to these scholarships is subject to change without notice.

33
PROGRAM POLICIES
To maintain a Program which provides the best possible education for the students and
efficient radiology departments that afford the highest quality medical care for the
patients, the following section of this handbook includes program policies that are
currently in effect for students enrolled in the HCCS Radiography Program. The
Radiography Program reserves the right to make any changes to this handbook at any
time with little or no notice. Policies included in the HCCS student online handbook are
also enforced.
ADA Consideration
HCCS recognizes its responsibility not to discriminate against anyone who has a
documented disability that substantially limits one or more major life activity; has a record
of such impairment; or is regarded as having impairment. Specific policies have been
established to enable students with documented disabilities who are otherwise qualified,
to request accommodations which would allow them equal access to the College under
Section 504 of the Rehabilitation Act of 1973 and under the Americans with Disabilities
Act of 1990.
A new, updated letter of accommodation would be submitted to instructors within the first
three (3) days of each semester. Students who submit a letter of accommodation any
time after the first three (3) days of a semester should expect to begin receiving
accommodations following a 24-hour timeframe for instructors to implement new
changes.
Obtaining reasonable accommodations is an interactive process that begins with the
student’s disclosure of his/her disability directly with the ADA Counselor in Ability
Services. The ADA Counselor for the Coleman College is in Room 101 of the Learning
Success Center (LSC).

34
Title IX Amendment
Houston Community College is committed to cultivating an environment free from
inappropriate conduct of a sexual or gender-based nature including sex discrimination,
sexual assault, sexual harassment, and sexual violence. Sex discrimination includes all
forms of sexual and gender-based misconduct and violates an individual’s fundamental
rights and personal dignity. Title IX prohibits discrimination based on sex-including
pregnancy and parental status in educational programs and activities. If you require an
accommodation due to pregnancy, please contact an Abilities Services Counselor. The
Director of EEO/Compliance is designated as the Title IX Coordinator and Section 504
Coordinator. All inquiries concerning HCC policies, compliance with applicable laws,
statutes, and regulations (such as Title VI, Title IX, and Section 504), and complaints
may be directed to:
David Cross
Director EEO/Compliance
Office of Institutional Equity & Diversity
3100 Main
(713) 718-8271
Houston, TX 77266-7517 or Institutional.Equity@hccs.edu
http://www.hccs.edu/departments/institutional-equity/title-ix-know-your-rights/
Texas HB 1508
Texas HB 1508 requires the following information to be given to students. If you are
applying for admission to a program that prepares an individual for an initial occupation
license or certification and/or if you later decide to change to a program that prepares
you for an initial occupational license or certification, in accordance with state law,
please be advised of the following:
1. An individual who has been charged or convicted of an offence or who is on
probation may not be eligible for issuance of an occupational license or
certification upon completion of the educational program.
2. It is the responsibility of the individual to immediately report to the program any
change in status that would affect that individual’s eligibility to apply for a license
or certification.
3. Local, state, or national licensing and certification authorities may issue
additional guidelines related to criminal history. Applicants should contact their
respective licensing or certification authority for more details.
Most health care programs require all students, admitted to the program, to submit to a
national background check. Applicants are encouraged to review all applicable eligibility
requirements related to the respective occupational license or certification. Questions
related to eligibility requirements should be directed to the individual program and
applicable licensing or certification authority.

35
ATTENDANCE POLICY
Students absent from a course for more than 12.5% of the total hours of instruction,
which includes labs, will be administratively dropped. Any student who is absent from
the class for more than 25% of a class session will be counted absent for the day.
Individual instructors have the right to make course-specific attendance and tardy
policies.
Attendance in clinic courses is addressed in this handbook under “Clinical
Considerations”.
BEREAVEMENT LEAVE POLICY
Upon submission of appropriate documentation (i.e., obituary, funeral program) to the
Program Director, a student may take up to three consecutive leave days in each year
for the death of the relative who is an immediate family member.
Immediate family members are:
Spouse Mother or Father-in-law
Mother or Father Brother or Sister-in-law
Brother or Sister Stepparents or Stepchild
Child Grandparent
Any days absent more than the three consecutive days or for the death of anyone
other than those listed above will be counted as an absence whether it occurs in a
didactic or clinical course.
CATASTROPHIC LEAVE
The HCC Radiography Program recognizes that certain life events require additional
attention from the student for short periods of time. Additional time away from the
classroom/clinic may, under catastrophic circumstances, be granted. These events will
be reviewed on a case-by-case basis by the Program Director and the Clinic
Coordinator.
Catastrophic leave will consist of no more than two weeks of the student’s clinic for that
semester. This is in addition to the time allotted for that semester’s absences. Makeup
time is mandatory and must be completed by the end of the following semester. The
student will be required to meet with the Program Director and the Clinical Coordinator
to schedule the make-up time.
PREGNANCY LEAVE
Pregnancy leave will consist of no more than two weeks of the student’s clinic for that
semester. This is in addition to the time allotted for that semester’s absences. Makeup
time is mandatory and must be completed by the end of the following semester. The
student will be required to meet with the Program Director and the Clinical Coordinator
to schedule the make-up time.

36
MEDICAL LEAVE
Should a student experience an acute injury, illness, or surgery during the Radiography
Program (either during the semester or on break time), a release from the student's
physician is required before the student may return to clinic. The release must state the
student's ability to participate in all the activities stated in the course syllabus. If the
student exceeds the absences for any semester due to injury, surgery, illness, or
pregnancy the catastrophic leave/ pregnancy leave policy will apply. Examples of
acute injuries include, but are not limited to, fractures of the extremities, whiplash,
concussion, contusions, open wounds requiring sutures, lumbar strains, etc.
DRUG SCREEN & BACKGROUND
Drug screen and Background information is offered through the CastleBranch online
system.
ï Background Check
ï 10 Panel Drug screen
- Repeated at start of the 2
nd
year of program (annually)
ï CPR certification (American Heart Association – BLS)
ï Proof of Health Insurance
ï All required Immunizations
Evidence of immunity for:
a. Measles, Mumps, Rubella (MMR) (positive titer)
b. Varicella Zoster (chicken pox) (positive titer)
c. Tetanus/diphtheria booster within the past 10 years
d. Hepatis B vaccine
e. Influenza vaccine
All students are required to have a background check and drug screen done yearly.
DRUG TESTING
To comply with the Joint Commission for Accreditation of Healthcare Organization’s
standards, the Health Science programs require criminal background checks and drug
screening on all accepted students to the Radiography program. This is required of all
students providing care, treatment or services in a JCAHO accredited clinical affiliate
and is part of the affiliation agreement.
In accordance with the Houston Community College Radiologic Technology Program,
students upon acceptance into the program are required to submit the results of a drug
screen as a condition of participation into the program. Background checks and drug
screens should be submitted to the program based on the procedures and timelines set
forth by the program. Students will be given instructions on testing procedures upon
acceptance and are responsible for the cost of the background check and drug
screening.
Students will be required to also submit another drug screen and background check
before the start of the 2
nd
year of the program. This is to ensure compliance with the

37
standards set forth by clinical affiliates.
The drug screening must include a 10-panel test type. This includes screening for
amphetamines, barbiturates, benzodiazepines, cannabinoids, cocaine, creatinine,
methadone, methaqualone, opiates, phencyclidine, and propoxyphene.
Based on the results of these tests, any affiliated clinical site may determine to not
allow your presence at their facility. Denial of clinical access could result in your
inability to successfully complete the clinical requirements of a specific course and
the program.
A student with a positive drug screen will be disallowed from clinical participation and
any course requiring clinical participation.
A student excluded for a positive drug screen may request reconsideration for program
entry the following year based on program readmission policies.
Students with a positive drug screening due to prescription medications will be required
to submit a physician’s note to support the positive drug screen results. The student will
be required to submit all physician supported documents to Castle branch. Failure to
submit physician supported documents within a timely manner will result in program
expulsion.
A clinical affiliate and/or clinical instructor reserves the right to remove a student from
the facility for suspicion of substance use or abuse, including alcohol. The affiliate
reserves the right to request that a student submit to a repeat drug screen at the
student’s expense on the same day that the student is removed from the clinical facility.
Failure to comply will result in the student’s immediate expulsion from the clinical facility
and can result in program penalties up to expulsion from the program.
DUE PROCESS
Students who wish to appeal a course grade must follow the policy as outlined in the
HCCS Radiography Program Handbook (Appendix D).
This completed information packet must be submitted to the College Dean’s office.
FINANCIAL AID & VETERAN’S BENEFITS & INCOMPLETE GRADES STATUS
The Radiography Program acknowledges that semester course work may not be
completed for various reasons. The Program follows the college policy on reporting (I)
incompletes when the student has been unable to complete the required course work
for reasons outside of his/her control. The Program shall not be held responsible for
any impact an incomplete grade has on his/her financial aid, scholarship, Veteran’s
Benefits or GPA.

38
HARASSMENT
The HCCS Radiography Program follows the HCCS Board Policy, in all matters dealing
with harassment by or of any employee of HCCS or students of HCCS.
If a student feels they have been the victim of harassment and report it to the Program
Director and/or Clinic Coordinator they must provide a written and signed statement
regarding the alleged harassment.
When the Program Director and/or the Clinic Coordinator receive this written and signed
statement, the charges of harassment will be investigated within 24 hours (Monday-
Friday business hours) and immediate action will be taken to ensure the student’s rights
are protected.
JRCERT COMPLIANCE
The Joint Review Committee on Education in Radiologic Technology (JRCERT) serves
as the accrediting body for the Houston Community College Radiography Program.
The goals of accreditation are to protect the student and the public, stimulate
programmatic improvement, provide protective measures for federal funding or financial
aid, and promote academic excellence.
There are six standards that the program must remain in compliance with and those
are:
Standard One: Accountability, Fair Practices, and Public Information
The sponsoring institution and program promote accountability and fair practices in relation to
students, faculty, and the public. Policies and procedures of the sponsoring institution and
program must support the rights of students and faculty, be well-defined, written, and readily
available.
Standard Two: Institutional Commitment and Resources
The sponsoring institution demonstrates a sound financial commitment to the program by
assuring sufficient academic, fiscal, personnel, and physical resources to achieve the
program’s mission.
Standard Three: Faculty and Staff
The sponsoring institution provides the program adequate and qualified faculty that
enable the program to meet its mission and promote student learning.
Standard Four: Curriculum and Academic Practices Health and Safety
The program’s The program’s curriculum and academic practices prepare students for
professional practice.

39
Standard Five: Health and Safety
The sponsoring institution and program have policies and procedures that promote the
health, safety, and optimal use of radiation for students, patients, and the public.
Standard Six: Programmatic Effectiveness and Assessment: Using Data for
Sustained Improvement
The extent of a program’s effectiveness is linked to the ability to meet its mission, goals,
and student learning outcomes. A systematic, ongoing assessment process provides
credible evidence that enables analysis and critical discussions to foster ongoing program
improvement.
To read more about these STANDARDS go to the JRCERT website at www.jrcert.org.
If you believe this program to be in non-compliance with JRCERT STANDARDS the
program requests that you, in writing, state the complaint to the Program Director and
allow 10 days for a written response.
If satisfaction is not achieved, you have a right to lodge a formal written, signed
complaint and send it to the JRCERT at 20 N. Wacker Drive, Suite 2850/Chicago, IL
60606-3182.
They will follow their Due Process Policies in investigating the allegations. Within 20
days following proper receipt of the complaint, the JRC will notify the complainant if
allegations are unfounded.
If yes, the JRC will acknowledge receipt of allegations to the complainant within 20
days of the receipt of the complaint and provide the policy and procedures pertaining to
investigation and resolution.
For more information regarding this, go to the JRC website, click on Policies and
Procedures and then on Public Responsibility Policies

40
PREGNANCY POLICY
A student may voluntarily inform the Program Director or Instructor of pregnancy
status (See Appendix C) and may continue enrollment in the program without
modification and interruption. Other options can include leave of absence from the
program and/or clinic. If declared, the pregnant student will then receive a fetal
monitor to wear over the abdominal area.
It is the individual student's responsibility to read and adhere to the guidelines set
forth in this policy for radiation protection of the embryo-fetus. A student is NOT under
obligation to inform the program of a pregnancy. At any time, a student may withdraw
their Declaration of Pregnancy by completing the form provided (See Appendix C).
Guidelines:
1. Each student may voluntarily report any suspected condition of, or known,
pregnancy to the Program Director so that additional protective measures can be
taken.
2. The Radiation Safety Officer or Program Director will counsel the pregnant student
concerning the effects of ionizing radiation in-utero and the additional protective
measures necessary to protect the embryo-fetus.
3. The pregnant student will acknowledge by signature, comprehension of the
instructions received during the counseling session regarding the mutual
responsibilities for protection of the embryo-fetus during her pregnancy.
4. In agreement with the Nuclear Regulatory Commissions (NRC) Regulatory Guide
8.13, the embryo-fetus is regarded as a separate entity, distinct from the woman
bearing it. Thus, the embryo-fetus carried by a woman who is a radiation worker is
not regarded as subject to the occupational limits, but rather to lower limits that are
necessary for its adequate protection.
5. In compliance with NRC Code of Federal Regulations (CFR) 10 part 19 and 20, and
the Texas Department of State Health Services (TDSHS), Texas Regulations for
Control of Radiation '289.202, the total dose equivalent limit (excluding medical
exposure) to an embryo-fetus during the entire pregnancy, due to occupational
exposure of a declared pregnant woman, shall not exceed .5 rem (5 mSv). Once a
pregnancy becomes known, exposure of the embryo-fetus shall be no greater than
0.05 rem (0.5 mSv) in any month (excluding medical exposure).
6. In compliance with NRC and TDSHS regulations, the pregnant student will be
provided a second personal monitor to assure that the dose equivalent to the
embryo-fetus does not exceed 0.05 rem (0.5 mSv) in a month. This monitor should
be worn at waist level, under the apron while in the clinical education setting. The
second monitor for the embryo-fetus should not be mixed up with the collar monitor
worn by the pregnant student radiographer.
7. It is not recommended that the pregnant student perform radiographic procedures

41
on patients receiving therapy with intra cavity or interstitial sources of radiation. If
fluoroscopy or mobile radiography procedures are performed, the pregnant
Radiography Student must wear two (2) lead aprons (one draped to the front and
the second draped to the back) with a minimum of 0.5mm lead equivalent.
(Reference: Radiologic Science for Technologists, by Stewart C. Bushong).
8. The quarterly radiation monitoring exposure report, the NRC Reports, and the
Texas Regulation for Control of Radiation are available for viewing in the office of
the Radiation Safety Officer, Coleman College, Room 527.
9. The pregnant radiologic technology student may continue enrollment in clinical
education courses. The pregnant student may resume training at the earliest
possible semester after the delivery or birth of the baby. All other clinical education
competencies and course requirements are expected to be accomplished.
10. After the student has had the opportunity to review the NCR Codes and decides to
voluntarily withdraw from clinical courses, the student must follow the re-admission
process established by the program and meet all requirements for re-admission.
Program extension due to pregnancy leave may not exceed one year beyond the
original scheduled completion date. If a student chooses to drop the course, it must
be done before or on the official drop date of the College.
The Nuclear Regulatory Commission’s publication Regarding Fetal Exposure is
included in this handbook (Appendix B). All students are to read this publication as part
of this handbook. Students may relay any questions or concerns to the Radiation Safety
Officer. Additional information regarding radiation protection can be found at
www.nrc.gov/NRC/radprotect.html
RADIATION SAFETY and MONITOR POLICY
Radiation safety is a term that includes the guidelines listed below. The lab is certified
by the Texas Department of Health for education only. Students will be expected to
always practice proper radiation safety procedures when present in clinical education
classes and in campus laboratory activities. This program embraces the ALARA
concept. When students are in the laboratory an instructor must be present when an
exposure is made. This is done to safeguard the health and safety of students. NO
HUMAN IS TO BE EXPOSED BY RADIATION IN THE RADIOGRAPHY LAB AT THE
COLLEGE CAMPUS FOR ANY REASON.
IT IS REQUIRED BY LAW THAT ALL PERSONS WORKING WITH OR AROUND X-
RAY EQUIPMENT WEAR CURRENT RADIATION MONITORS.
Radiation monitors are furnished to students in accordance with existing state and
federal regulations, which require that students wear them when working in areas
where potential radiation exposure may occur. The reports regarding exposure become
a part of the student’s permanent record and are open for their inspection. When the
student leaves this institution, he/she may request a copy of their exposure record to
either take with them or to have sent to their employer. To utilize the radiation, monitor
most effectively and to have the most accurate records possible, the following

42
regulations must be observed:
ï Students must wear radiation monitors when at their clinical affiliate and at the
college when using the energized lab.
ï Students must be supervised and monitored by a licensed Radiography Instructor
when using the energized lab at the college when practicing and simulating exams.
All energized lab rooms will be locked if an instructor is not present, and students
may use the non-energized equipment to practice.
ï The radiation monitors are to be worn as follows: At the collar, outside the apron.
ï Prevent dosimeters from exposure to moisture and from receiving excessive
exposure from radiation.
ï Dosimeters are only to be worn for HCCS assignments.
ï Any student not wearing a radiation monitor will not be allowed in radiation areas,
and the time missed to retrieve the badge will be considered a late arrival to
lab/clinic. If the student cannot arrive back to the lab within one hour or clinic within
2 hours an absence will be recorded.
ï Students will be required to wear a lead apron and thyroid shield during procedures
such as: fluoroscopy, C-arm procedures, and portable radiography.
ï Students will never hold a patient or image receptor during a procedure while ionizing
radiation is in use.
Radiation monitoring devices will be changed quarterly. Within 30 days following receipt
of the exposure reports, school faculty will bring the report to class. Exposure reports
will be reviewed, and the student is required to initial the quarterly report to
acknowledge their monthly/quarterly exposure level. A permanent record of the
student's radiation monitoring report will be kept in a secure area.
Notice: Students will be instructed in the as low as reasonably achievable (ALARA)
philosophy. The Program Director, Clinical Faculty, and Radiation Safety Officer will
investigate all instances in which dose limits are exceeded. The student will then be
counseled as to the appropriate course of action and review of radiation safety
practices. Actual dose limit is any single quarterly reading of 125 mrem or above.
“Accidental” exposures due to badges left on aprons, etc., will be documented where
proven.
If you suspect there has been an excessive exposure or radiation incident, immediately
notify Radiation Safety Officer: Dr. Elizabeth Ho, DHsc, RDMS (AB,OB), R.T.
(R)(ARRT). The RSO will then notify the bureau of radiation control. The address is:
Texas Department of Health, Bureau of Radiation Control, 1100 West 49th Street,
Austin, TX, 78756-3189. The telephone number during working hours is 512-835-
7000; the emergency telephone number is 512-458-7460.
Failure to follow these policies will result in dismissal from the program.

43
READMISSION POLICY
The program has established a policy that students may enroll in the Radiography
program twice. There is the initial admission and, if necessary, one readmission. If a
student fails (withdraws from) a class, he/she must have an Exit Interview with the
Program Director at the time of the exit. If the Program Director is not available the
student must, at the time of the exit call/email to schedule an appointment at the
Director’s earliest convenience. Documentation resulting from this interview will be
placed in the student's file. Should the student fail (withdraw from) another class after
one readmission to the Program, the student will be ineligible for readmission.
A Readmission Committee will review each student’s request for Readmission.
Applications will not be considered if the deadline is not met.
If a student fails or withdraws during the first semester, the student is not eligible for
readmission and must reapply to the Radiography program as a new student. This will
count as a second admission.
TRANSFER POLICY
The HCCS Radiography Program follows the Workforce Education Course Manual
(WECM). Radiography courses may be transferred to other community colleges in
Texas. The academic courses are transferable to most colleges and universities. For
further information on transfer and the academic calendar, see the HCCS catalog. For
tuition, fees, and refunds, and to view the academic calendar consult the online
Schedule of Classes at www.hccs.edu
WITHDRAWALS
To help students avoid having to drop/withdraw from any class, HCC has instituted an
Early Alert process by which the instructor will alert the student and the HCCS Health
Science Counselor of the failing grade, excessive absences, and/or poor academic
performance. The student is required to contact the Coleman Counselor regarding the
concern indicated by the instructor. Faculty will not be able to assign a “W” after the
drop date. Students are entirely responsible for withdrawing themselves from courses
in which they are not being academically successful.
PROGRAM PROCEDURES
GRADUATION
Radiography students must apply for graduation after completion of the 6
th
semester
and are eligible for the Fall Ceremony. This is done by completion of the required
official college form. All official transcripts must be submitted to the graduation office.
In the unlikely event that this has not already been done, students must submit official
transcripts for all college work completed prior to entering the program. Official
transcripts must be mailed to the HCCS Student Services Department (Coleman, 1
st
Floor Student Services) directly from the registrar's office of the college attended or
hand carried in an officially sealed/unopened envelope.

44
Caps and gowns must be ordered through HCCS. The Radiography Program has a
recognition ceremony (The Pinning) in the final (6
th
) semester.
GRADUATION REQUIREMENTS
Students must have fulfilled all requirements specific to the HCC Radiography
Program. This includes having maintained a grade point average of at least a 2.00,
completed all radiography courses with a grade of a “C” or higher, completed all
required hours in clinicals, and be proven competent of the expectations set forth by
the (ARRT) American Registry of Radiologic Technology.
Graduation information can be found at: https://www.hccs.edu/resources-for/current-
students/graduation/
APPLICATION FOR THE ARRT EXAMINATION
Graduates of the Radiography Program are eligible to sit for the ARRT certification
examination. Each student must officially apply to ARRT to take the examination and
the Program Director must sign approval for the student to qualify.
To be eligible, students must be graduates of the program and have received their
associate degree. This means all courses including the academic support courses have
been successfully completed and the final GPA is 2.0 or above. Students who have
been convicted of a felony or misdemeanor may not be eligible to take the ARRT exam.
If a student has a question of eligibility, contact the ARRT at (612) 687-0048 or
www.arrt.org Students must enclose official documentation of their conviction when
applying for the exam. If a student’s background comes into question at the time of
acceptance into the program or after acceptance into the program, the student will not
be allowed to start the program until a ruling has been made on their background by the
ARRT.
During the final (6
th
semester) didactic course, each student will create an ARRT online
account. The Program Director will provide the instructions and web link for students to
create the account. When the account has been set up and questions answered on
each screen, it will be reviewed and verified by the Program Director. The student must
be prepared to mail submit the appropriate fee to the ARRT.
A paper application may be required. Exceptions for Using the Online Application will
consist of those would already have an ARRT ID number, applied by paper and failed
their exam, and submitted an ethics review.
A Background Check must be cleared before a student can be accepted into the
Radiography Program.

45
APPLICATION FOR CERTIFICATION (Texas Medical Board)
Applications for the TMB may be obtained online in RADR 2335 at the appropriate time.
The student will be responsible for submitting the application and all associated fees.
As with the ARRT, a student/applicant convicted of a felony or misdemeanor may not be
eligible for a license.
If a student’s background status changes or becomes more fully known after they have
been accepted into the program and this discovery jeopardizes their ability to sit for the
registry or receive a TMB license, they will be required to withdraw from the program
until it is resolved.

46
HOUSTON COMMUNITY COLLEGE SYSTEM
HEALTH SCIENCE PROGRAMS
RADIOGRAPHY PROGRAM
PROGRAM READMISSION PROCEDURES
I. Students who withdraw from the Radiography Program and apply for
readmission must complete their program degree plan within a limited
time.
A. Students enrolled in Associate Degree programs must complete the
program degree plan within a three-year period.
B. In spring, 2005, a state law went into effect which stops reimbursing a
community college for students who have repeated a course more than 2
times.
II. Conditions under which readmission to a program will not be approved:
A. Dismissal from the program due to scholastic dishonesty.
B. Dismissal from the program due to a serious violation of
professional/ethical standards in clinical education center.
C. Dismissal from the program due to a serious violation of safety and patient
protection.
D. Dismissal from the program due to violation of the college code of conduct
(i.e., drug or alcohol abuse, theft, etc.).
E. Excessive absences, tardiness, or behavioral problems (including
students who stop showing up for class).
F. Letters received or verbal notification asking that a student not be allowed
to remain/return to a clinic site.
G. Poor academic history.
H. Student would not be able to complete all Radiography course work in a
three-year period.
I. Students who do not have an exit interview at the time of withdrawal.
J. Students who do not complete the readmission application by the date
specified in the exit interview.
III. Evaluation procedures for knowledge and skills:
A. Applicants must contact the Department Chair for approval to be
readmitted. The Department Chair will inform the applicant if challenge
examinations are necessary prior to enrollment.
B. A student who has been out of the program for 2 years or more will have
to apply as a new student and be competitive with other students initially
applying to the program.
IV. An Exit Interview is required for the student to be eligible for
readmission.
A. The interview must occur at the time of the withdrawal. Only the
Department Chair or Clinical Coordinator is allowed to sign a withdrawal slip
and conduct an exit interview. Students obtaining any other signatures on
the withdrawal slip will forfeit their chances for readmission.

47
Students who stop attending class and/or have no communication with the
Department Chair or Clinical Coordinator after failing/withdrawal also forfeits
his or her chance for readmission.
B. The Exit Interview will take place at the time of withdrawal. The content of
the interview is recorded using the Exit Interview Form. The
recommendations given to the student are documented on the form and
may include remediation courses, work with tutors, life-style changes, etc.
Any progressive action taken by the student may enhance the student’s
application for readmission.
V. Students who withdraw from a program due to personal reasons or failure
of a course, and are eligible to be readmitted, WILL BE REQUIRED TO
COMPLETE THE APPLICATION FOR READMISSION. Students who withdraw
from the program for personal reasons or failure of a course may apply for one
readmission to the program. If the student withdraws or fails a second time,
he/she will not be eligible for readmission.
VI. A Review Committee for Readmission (RCR) will evaluate each application
for re-admission. The committee's evaluation may include the Exit Interview,
action(s) related to recommendations and assessments made by program faculty
regarding the student. Each application will be reviewed on an individual basis.
The student applying for readmission will become competitive for a space in the
program along with the new class. Readmission cannot occur if the class size is
at capacity.
VII. The Readmission deadline dates for students who fail/drop out of the
program:
A. Fail/drop in the summer semester, application due on or before February
1
st
, of the following year
B. Fail/drop in the fall semester, application due on or before May 1st
the following year
C. Fail/drop in the spring semester, application due on or before October 1
st
the following year
VIII. The Readmission Committee will meet (if changes are made to this
calendar students will be notified):
A. Last week of February for summer readmissions
B. Last week of May for fall admissions
C. Last week of October for spring admissions
IX. Students who are readmitted to program in the first semester will be
required to attend the new orientation.
NOTE: THE DECISION OF THE READMISSION COMMITTEE WILL BE FINAL.
CLINICAL CONSIDERATIONS
The Coleman College for the Health Sciences promotes academic integrity and
standards of conduct for the health science community. Coleman College is also
responsible for investigating alleged violations of student conduct and for implementing
the discipline process. Health science students have a responsibility to learn the
academic theory and clinical skills needed to provide safe, efficient health care and to
follow program standards of conduct and academic integrity.

48
ACADEMIC AND CLINICAL STANDARDS
To prepare students for the high ethical standards of the health professions, Coleman
College for Health Sciences expects absolute academic and professional integrity, both
in the classroom and in the clinical setting. Students are expected to demonstrate
professional and ethical behaviors consistent with the practice standards for
Radiography as published on the American Society of Radiologic Technologists website
at http://www.asrt.org
SOCIAL NETWORKING AND STUDENTS IN HEALTH CARE PROGRAMS
Students in health care programs must adhere to federal laws regarding HIPPA protected
information and college policies regarding protection of privacy of the student’s patients.
Students may not post any photos, videos, patient information, or any other data
regarding patients or affiliations on Social Networking sites, including but not limited to
Facebook, Instagram, Myspace, Twitter, TikTok, and YouTube.
TRAJECSYS
The Radiography Program uses an on-line student record management service known
as Trajecsys. Trajecsys is also used by the faculty to maintain accurate records of each
student’s performance in the clinical setting. It is the student’s responsibility to purchase
Trajecsys before the start of clinical rotation.
This system is used by each student to:
ï
Clock In/Out from their clinical education site(s) in the main radiology department.
ï
Access the system daily for clinical announcements / updates, clinical
documents, etc.
ï
Enter Daily Log Sheets of all work/exams done in the clinical setting weekly
ï
Access monthly evaluations
ï
Submit competency attempts, view, and acknowledge completed
competencies. The Trajecsys Reporting System website can be
found at: https://www.trajecsys.com
ï
Students are required to verify that all competencies are entered in
Trajecsys before completing each semester.
TRAJECSYS - DIGITAL CLOCK IN AND OUT
All students must clock in and out each clinical day from a computer with internet
access at the clinical site. It is important that the student selects the correct clinical
location each day. Students must be on site to “clock in” using the hospital computer
located in the main department. IP addresses are recorded in Trajecsys to verify where
a student is located each clinical day.
Some clinical sites may require the use of the Trajecsys GPS personal device/cell
phone feature to record the daily attendance of a student. The GPS, or Geolocator
feature may only be utilized if the clinical site does not allow computer access.
Students must be on site and located in the main department to use this feature. The
student may use their personal device/cell phone with the GPS location enabled to

49
clock in/out and to have their location recorded daily. Personal devices should be
stored away during the clinic rotation and is only to be used to access Trajecsys. This
feature can only be utilized if approved by the clinical instructor assigned to the clinical
site. No Exceptions.
CLINICAL ATTENDANCE
Attendance is required for all clinical practicum courses, seminars, and practice.
Students may be asked to attend day and/or evening and weekend clinical
assignments. The Radiography program does not have mandatory evening
assignments, but students may be asked to attend evening assignments at certain
times during their training.
Faculty members may exclude students from the clinical area due to illness, injuries,
lack of preparation for practice, inappropriate attire, and/or any situation deemed
unsafe. The absence may be reflected in the student's grade.
The clinical education sites will follow the attendance policy published in the Program
Handbook and in each clinical course syllabus. These polices follow the 12.5% of total
hours absent as covered in the HCCS Student Handbook.
All students are required to "clock-in" each day upon arrival and "clock-out" upon
departure from the clinical education site. If a clinical site has a different procedure, it
will be explained during the clinical orientation at the beginning of the semester. This
procedure allows the clinical instructor to keep accurate records relating to attendance.
If the clinic begins at 7:30 a.m., any time clocked in after 7:37 a.m. is late. If the 7
minutes grace period is abused, it will be discontinued. Abused, in this paragraph
means a student has violated the grace period 3 times. At 7:30 a.m. each student is
expected to be in their assigned area ready to participate in the daily activities. Even
though a student has clocked in and is in the clinical facility does not constitute being
"on-time".
For example, if a student is found eating breakfast in the cafeteria at 7:50 a.m. this
student would be considered out of their assigned area until he/she is back in their
assigned area, ready to participate in clinical education process. This time will be
reflected on the timesheet as “tardy”, and the appropriate number of minutes will
be deducted.

50
Punctuality and Dependability are essential parts to the Professional Development for
all students in the Health Care Field. It is extremely important that students begin to
learn good professional habits in the clinical education courses. This is very important
so that patients are not kept waiting for personal care and services.
A. Students are expected to report promptly to their clinical instructor or designated
technologist in charge at the time they arrive for their clinical education
assignment, before leaving for a lunch break and before leaving the department
for class or to go home. Students are to remain in their assigned areas for the
entire clinical day. Breaks are given at the discretion of the clinical instructor.
Any student taking unauthorized breaks will be subject to discipline.
B. Lunch periods will not exceed 30 minutes in length and will be assigned by the
clinical instructors or in their absence by the adjunct clinical instructor/supervisor
in charge.
DEFINITIONS
A. TARDY -- A student is tardy when he/she is not present or reported to the clinical
adjunct or instructor at the assigned time on the clinical education schedule.
Point deductions from clinical grades are taken for tardiness.
B. ABSENCE -- The student is required to call the clinical instructor, designated
adjunct clinical personnel, and facility in charge to inform them of their absence.
EARLY DEPARTURE -- A student that leaves early for any reason (appointment, illness,
etc.) will be marked for an early departure. The student must be in clinic for 75% of the day
to be counted present. Point deductions are taken for leaving early in the same fashion as
they are for arriving late. The student may leave 2 hours early and still be counted present
with 5 percentage points being taken off their attendance grade for each early departure. If
his/her clinic is scheduled for ½ day, then he/she may leave 1 hour early.
C. ABSENCE WITH DISCIPLINE -- An absence with discipline is when the student
does not telephone the clinical instructor or designated adjunct clinical
person/supervisor in charge to inform them or explain the absence. This
includes not calling in during the 30-minute time limit set in the syllabus. In
addition to not being

51
D. JURY DUTY/COURT SUMMONS -- Jury Duty and Court Summons are
considered excused absences but with the following policy: Students who
receive a summons to appear for jury duty or court testimony must inform their
instructor as soon as possible. The student must present to the Program
Director and/or his/her instructor a verification form obtained from the clerk at the
courthouse. This verification form must be the original with the proper signatures
and dates present in court. The verification must be presented on the first day
back to class. Adherence to this procedure will prevent a deduction from the
student's leave days. Traffic violations are not considered court testimony and
are not covered under this policy. An allowed absence day may be used in this
instance.
E. ALLOWED ABSENCES -- Each semester the clinic course syllabus will identify
the number of days a student may be absent without being penalized. A medical
excuse does not preclude being counted absent.
PERSONAL INSURANCE
Students must utilize his/her personal Accidental Insurance policy for injuries that may
occur during the time when assigned to clinical education. The clinical instructor/
preceptor must be notified immediately of any injury. The student is responsible for all
costs associated with the injury.
CLINICAL CODE OF CONDUCT
A student shall:
1. Always provide safe and professional patient care and implement measures to
promote a safe environment for each patient.
2. Comply with policies, procedures, and rules related to academic and clinical
performance that are issued by Coleman College, by a Coleman health science
program, by HCCS, or by any clinical agency.
3. Not commit acts of omission or commission that cause or are likely to cause harm to
patients/clients.
4. Not attempt care/activities without adequate orientation, theoretical preparation,
assistance, or supervision.
5. Maintain patient/client confidentiality.
6. Take appropriate action to assure the safety of patients/clients, self, and others.
7. Provide care for the patient/client in a timely, compassionate, and professional
manner.

52
8. Communicate with patient/client and healthcare team in a truthful, timely, and
accurate manner.
9. Actively promote the highest level of moral and ethical principles and accept
responsibility for his/her actions.
10. Treat others with respect and promote an academic and clinical environment that
respects human rights, values, and choice of cultural and spiritual beliefs.
11. Collaborate and cooperate in every reasonable manner with the academic faculty
and clinical staff to assure the highest quality of patient/client care.
12. Abstain from the use of substances that impair judgment.
13. Report and document all patient/client assessments or observations, the care/
practice provided by the student for the patient/client, and the patient’s client's
response to that care/practice.
14. Accurately and timely report to the appropriate practitioner errors in or deviations
from the prescribed regimen of care/practice.
15. Not falsify any patient/client record or any other document prepared or utilized
during, or in conjunction with patient/client care/practice.
16. Delineate, establish, and maintain professional boundaries with each patient/ client.
When providing direct patient/client care, the student shall provide privacy during
treatment and care/practice and shall treat each patient/client with courtesy, respect,
and with full recognition of dignity and individuality.
17. Not engage in behavior that causes or may cause physical, verbal, mental or
emotional abuse to a patient/client; or engage in behavior toward patient/client that
may reasonably be interpreted as physical, verbal, mental or emotional abuse.
18. Not misappropriate a patient/client's property or engage in behavior to seek or
obtain personal gain at the patient/client’s expense; engage in behavior that may
reasonably be interpreted as behavior to seek or obtain personal gain at the
patient/client’s expense; engage in behavior that constitutes inappropriate
involvement in or interference with the patient/client’s personal relationships; or
engage in behavior that may reasonably be interpreted as inappropriate involvement
in the patient/client’s personal relationships. For the purpose of this paragraph, the
patient/client is always presumed incapable of giving free, full or informed consent to
the behaviors by the student set forth in this paragraph.
19. Not engage in sexual contact or romantic relationships with a patient/client; engage
in conduct that may be reasonably interpreted as sexual or romantic; engage in any
verbal behavior that is seductive or sexually demeaning to a patient/client; or
engage in verbal behavior that may reasonably be interpreted as seductive or
sexually demeaning to a patient/client. For the purpose of this paragraph, the
patient/client is always presumed incapable of giving free, full or informed consent to
sexual or romantic activity with the student.
UNSAFE OR UNPROFESSIONAL PRACTICE
A student whose clinical practice is judged unsafe or unprofessional may be removed
from the clinical experience.
To be eligible to resume the clinical experience, the student who has been

53
removed must comply with stipulations prescribed by the faculty for readmission to the
clinical experience.
The faculty responsible for the clinical experience will review the clinical care/practice of
a student who exhibits weaknesses that may lead to unsafe or unprofessional practice.
The faculty, with appropriate input from the student, will develop a set of expectations
that the student is to attain to remedy those weaknesses in the current and subsequent
semesters.
Rationale:
Faculty have a legal and professional responsibility to assure for the public, other
students, Coleman College, and the Radiologic Technology (Radiography) program that
students can practice safely and professionally in their various clinical duties.
A student shall always provide safe and professional patient care. Performance that will
result in disciplinary action by the Radiography Program include, but is not limited to,
the following:
1. Does not meet the practice standards for Radiography as published on the American
Society of Radiologic Technologists website at http://www.asrt.org ,
2. Does not comply with the Standards of Ethics as published on the American
Registry of Radiologic Technologists website at http://arrt.org
3. Does not comply with HCCS Policy
4. Does not comply with Radiography Program Policy
Depending upon the degree of actual or potential harm a patient may suffer a onetime
deviation from safe practice may be sufficient to judge a student unsafe.
Examples of unsafe, unprofessional, or unacceptable practice include, but are not
limited to, the following and will result in the stated consequences.
The following behaviors will result in immediate dismissal from the HCCS
Radiography program:
1. Bring or carry a weapon into the clinic
2. Being under the influence of drugs or alcohol
3. Theft of hospital or college property
4. Students who engage in sexual activity during clinic hours
Falsification of attendance, competencies, evaluations, or any other program
documentation (including clocking in for other students in Trajecsys) will result in a
drop of one letter grade for the 1
st
offense. Any subsequent offense will result in
dismissal from the program.
Altercations, physical or verbal, will result in immediate removal from clinic until the matter
is resolved. Punishment can range from reduction of the clinic grade, up to dismissal from
the program. The time out of clinic will be deducted from the student’s attendance.

54
The following behaviors will result in a reduction of the final clinic grade by one letter for
each offense:
1. Failure to stay in assigned clinic area. This includes not being able to locate a
student in 15 minutes.
2. Leaving the assigned work area in clinic without permission, or notifying the Clinical
Instructor or Adjunct Faculty.
3. Cell phones and smart watches will not be worn or used by students during clinic
hours. Phones brought to clinic must be stored and turned off. A student may
use their cell phone during lunch in a non-patient care area only. If there is an
emergency, and a student needs to be contacted while in the clinical setting, the
phone call must go through the clinical instructor or adjunct faculty. Students are
urged to inform family, friends, employers not to contact them during clinical
hours unless it is an emergency.
4. Use abusive or foul language.
5. Sleeping or the appearance of sleeping while on clinic hours.
6. Lack of professional respect for authority, i.e., the C.I. or clinical staff.
Any behavior that is considered unprofessional or reflects negatively on the college,
program, or clinic will be viewed as unacceptable. DOCUMENTED VIOLATION OF
ANY OF THESE POLICIES WILL RESULT IN THE ACTION(S) INDICATED. The
student has the right to Due Process, i.e., the student can, in writing; submit their side of
the event to the Program Director, within 3 days of the documented violation. The
Program Director will follow up within 5 business days. The Program Director may call
in the student and others who can give information. A decision will be made within 2
days of the final meeting.
CLINICAL SUPERVISION POLICY
Students (First or Second year) shall not take the responsibility or place of qualified staff
radiographers. All students enrolled in this course are part of the HCCS Radiography
Program Competency Based Clinical Education Plan (CBCE).
The following operational policies are to be implemented by the Clinical Instructor:
Until a student achieves the prescribed competency level (documented in file) he/she
will carry out assignments under the direct supervision of a qualified radiographer.
DOCUMENTED VIOLATION OF ANY OF THESE POLICIES WILL RESULT IN A
MEETING WITH THE CLINICAL COORDINATOR AND/OR THE PROGRAM
DIRECTOR FOLLOWED BY DISCIPLINE, IF SUBSTANTIATED.

55
The JRCERT defines direct supervision as student supervision by a qualified radiographer who:
ï
reviews the procedure in relation to the student’s achievement,
ï
evaluates the condition of the patient in relation to the student’s knowledge,
ï
is physically present during the conduct of the procedure, and
ï
reviews and approves the procedure and/or image.
Students must be directly supervised until competency is achieved. Once students have
achieved competency, they may work under indirect supervision. The JRCERT defines
indirect supervision as student supervision provided by a qualified radiographer who is
immediately available to assist students regardless of the level of student achievement.
Repeat images must be completed under direct supervision. The presence of a qualified
radiographer during the repeat of an unsatisfactory image assures patient safety and proper
educational practices.
Students must be directly supervised during surgical and all mobile, including mobile fluoroscopy,
procedures regardless of the level of competency.
Failure to comply with this policy may be grounds for suspension or termination.
Direct Supervision: The radiographer evaluates the requisition, the patient's condition
and especially the student's competency relating to the condition of the patient,
observes the student's work and reviews the radiographs with the student following the
procedure.
Once the student has achieved documented competencies, he/she may
complete assignments under indirect supervision.
Indirect Supervision: Means that a qualified radiographer must be in the immediate
area to assist the student regardless of the competency level of the student. Under no
circumstances should a student be assigned alone to an area. A qualified radiographer
must review all images with student before the images(s) are sent to the radiologist or
referring physician.
Repeat Radiographic Images: Unsatisfactory or unacceptable radiographic images
may be repeated by a student only in the presence of a qualified radiographer (includes
portable images).
JRCERT Objective 5.4 -Assures that medical imaging procedures are performed under
the appropriate supervision of a qualified radiographer.

56
CLINICAL OBJECTIVES
Students must demonstrate the ability to perform the following tasks under direct or
indirect supervision of the registered radiologic technologists or radiologists:
General Clinical Objectives
ï
Provide proper patient care and communicate effectively
ï
Protect patient, personnel, and self from unnecessary exposure to ionizing radiation
ï
Correctly process radiographic images for diagnostic purposes
ï
Properly position patient for the purpose of performing authorized diagnostic examinations
ï
Assist in the maintaining of appropriate files pertaining to radiology records
ï
Assist in the maintenance and troubleshooting of radiological equipment and maintain
supplies, cleanliness, and order in the radiographic room
ï
Manipulate and operate equipment properly in the radiology department, surgical suite,
emergency room and at the patient’s bedside
ï
Critique images for the purpose of evaluating techniques, positioning, and other pertinent
technical qualities
ï
Provide care and comfort to the patient, demonstrate aseptic technique, and assist the
radiologist or other physician(s) with procedures requiring the use of ionizing radiation
contrast media or sterile techniques
ï
Select exposure factors to achieve optimum radiographic technique with minimal radiation to
the patient, personnel, and self
ï
Become familiar with the various types of radiographic cand fluoroscopic machines, mobile
units, contrast agents, emergency protocols and equipment
ï
Produce images of any given anatomical region with optimum diagnostic quality
ï
Perform necessary diagnostic procedure with a minimum discomfort to the patient and utilize
the best possible radiation protection measures which are appropriate for the examination
ï
Apply the academic material in the clinical setting under the direction and guidance of a
registered technologist
ï
Maintain a positioning and/or technique pocket notebook
ï
Develop professional standards, attitudes, and ethical conduct
ï
Identify and explain the following items that may be required by the individual clinical
affiliates:
o Radiographic examination routine
o Radiographic room preparation
o Contrast media preparation
o Patient instruction for specific radiological exams
o Interpretation of radiologic examination request form

57
PROFESSIONAL BEHAVIOR
When in a clinical/hospital setting, students will be expected to:
1. Knock prior to entering a room
2. Refrain from congregating in patient care areas. Students must have CI permission
to be out of their assigned area (students are not assigned breaks). Students cannot
sit, rest, or recline in public areas such as the reception area. Idle time should be
used for practice and study.
3. Keep all information about patients or other department personnel confidential;
information must not be discussed in any public area and charts must be kept out of
reach of unauthorized persons including patients. Radiographic images are the
property of the hospital.
4. Discuss matters pertaining to the Radiology Department in private areas only, not in
elevators, corridors, or any public area in the hospital or college campus. No
conversation should take place within a patient's hearing range that is not intended
for him/her to hear.
5. Consume beverages and food in the lounge area only and with permission of the CI.
6. Refrain from chewing gum.
7. Demonstrate professional behavior in all aspects of clinical education specially to include
the consideration of the rights of other students in the program. Harassment of students
by peers is unacceptable and will result in disciplinary action by the program faculty.
8. Wear student I.D. and dosimeter always for clinical education classes

58
PROBATION GUIDELINES FOR CLINIC
When a student is placed on probation in a clinic course the following guidelines will be
followed:
1. The student will always work under direct supervision.
2. The student will be assigned to work with one (1) technologist, not an area of the
department.
3. The student must be assigned to the main department of the Radiology Department
until assignment to another area (i.e., surgery, portables, etc.) is approved by the
Clinic Instructor and the Clinic Coordinator.
4. Any documented infraction of Program Policy can result in further discipline up to
immediate removal of the student on probation from the clinic and the Radiography
Program. These infractions include, but are not limited to:
Failure to always wear film badge/dosimeter while in the clinic
Failure to always wear the approved photo identification badge while in
the clinic
Failure to follow Program and clinic policies as identified in the Program
Handbook and the clinic syllabus
Insubordination
5. The student will have the right to continue competency testing in the approved
manner as outlined in the Program Handbook and the clinic syllabus.
6. The student must competency test with the Clinic Instructor until the Clinic
Coordinator approves testing by a designated technologist.
7. The Clinic Instructor will make weekly written reports to the Clinic Coordinator to
document the progress of the probationer. The probationer will read and sign this
weekly report. The student’s signature indicates the student has read the report
only. It does not indicate agreement with the statements made in the report. The
probationer will have the opportunity to address, in writing, anything with which they
do not agree
8. The length of probation will be to the end of the semester in which the incident(s)
occurred. The period of probation may be extended beyond the current semester,
with cause, at the discretion of the Program Director and the Clinic Coordinator.
Should a clinical education center ask for a student to be removed from that clinic due
to unsafe practices/unprofessional behavior, the student can be penalized up to
dismissal from the program. The student has the right to due process. The clinical
coordinator will assess the information regarding the infraction and with the instructor
and program director, a decision will be made regarding whether the student will be
dismissed from the program. If the gravity of the student behavior is found to be
questionable, the student will be counseled and put on probation. Any additional
incidents involving unsafe practices/poor patient care/unprofessional behavior would
result in dismissal from the HCCS Radiography Program.

59
Clinical instructors can evaluate students for inappropriate or unprofessional behavior
on the Faculty Evaluation Form. A “Faculty Evaluation Form” can be entirely devoted to
evaluating a student’s behavior or other professional concern. This is in addition to
other penalties that may apply.
ENTRY INTO CLINICAL COURSES
All health profession students must present evidence of having met specific health and
legal requirements prior to engaging in clinical experiences. The evidence must be
submitted by the date published. Failure to comply with the requirements by the defined
deadline will result in prevention of enrollment or administrative withdrawal from clinical
courses. The requirements are mandated by the clinical agencies used by Coleman
College for clinical experiences.
All requirements apply unless medically contraindicated by physician documentation.
Additional testing, evaluation, and documentation may be required in individual cases.
All records are considered confidential material and will not be released to anyone
without a student’s written permission.
Satisfactory physical and mental health must be maintained for continuance in the
program. Applicants must be free of any physical and/or mental condition that might
adversely affect their acceptance or performances in the program. The HCCS reserves
the right to require medical examinations to verify continuing compliance. Students with
existing physical and/or mental conditions which might adversely affect performance in
the program, who do not self-disclose this information are subject to dismissal from the
program.
HEALTH RECORDS REQUIREMENT
Each student is required to maintain all immunizations. It is the responsibility of each
student to provide proof of immunizations upon entry into the program and maintain
currency of immunizations during the program. Students will be asked to provide proof
of immunizations during the program.
Each student is required to provide proof of annual TB testing and influenza
immunization. This proof is required upon entry into the program and again each
calendar year during the program. Failure to provide proof will result in the student not
being to attend clinic until proof is provided. Students will receive an absence for each
day excluded from clinical due to immunization status (documentation must be
uploaded to CastleBranch).
COVID Policy
To provide students with the most robust clinical educational experience and to
ensure that students progress and graduate as scheduled, it is highly recommended
that applicants weigh all of their options before agreeing to a conditional acceptance
into their desired health science program. In order to facilitate this decision-making,
students should understand all of the requirements of their program, including clinical
education.
60
To be placed in a clinical educational experience, students must comply with the
guidelines and requirements of HCC clinical sites, including health and wellness
directives. Most clinical sites require background checks, health testing, drug screens
and immunizations, including proof of COVID-19 vaccination.
Students are required to provide to HCC proof that students meet all clinical
requirements, with the exception of their COVID-19 vaccination status. Consistent
with state law, HCC does not mandate the COVID-19 vaccination. Students have the
choice to voluntarily disclose or not disclose their COVID-19 vaccination status
through their HCC Castlebranch account.
However, most healthcare facilities do require the vaccine as a condition of
employment, volunteering, or student clinical placement. If a student chooses not to
disclose their COVID-19 vaccination status or is not vaccinated, HCC may not be able
to place the student in clinical rotations. HCC will work to place such students into a
clinical site that does not require the vaccine, provided such a site is available and
HCC has an active affiliation agreement in place that meets the necessary conditions
to provide an appropriate learning opportunity for the student. However, HCC cannot
guarantee that clinical sites that do not require the COVID vaccine will be available at
the time the student requires placement. At this time, many healthcare facilities are
not accepting religious or medical exemptions for the COVID-19 vaccine for clinical
students.
If a student chooses not to receive or to provide proof of COVID-19 vaccination and
no clinical sites are available to accept the student that do not require the COVID-19
vaccination, the student’s progression in the program and graduation will be delayed
or stopped all together. If a student cannot be timely placed in a qualifying clinical site,
a student may not be able to complete the program. Our affiliate partners’
expectations are the same for our students as they would be when our students
ultimately become employees in their chosen field.
Students with questions about clinical requirements and placement may contact the
program director of their program of interest.
61
CPR REQUIREMENT
All students must submit evidence of current Basic Life Support (BLS) certification compliant
with the American Heart Association (AHA) and the certification must be good for 2 years.
DRESS CODE AND UNIFORM
A strict dress code is required in the clinical setting. Each student assumes the cost for
his/her uniform. Uniforms are worn to protect the patient and student. Students who
appear in clinic without the proper uniform will be sent home.
Your standards of personal care and dress represent you as an individual, Coleman
College, and the profession of Radiography. Professional people set examples for
others and students are expected to be neat clean, and well-groomed which includes
the following:
Nails
Nails will be clean, short, and smooth to ensure patient and student safety.
Artificial nails are prohibited.
Natural nail tips must be less than 1/4 inch.
Colored Nail polish, nail jewelry or ornamental accents are prohibited.
Clear nail polish is acceptable.
Hair
Hair is controlled so that asepsis is maintained for the student, patient, and client.
Plain barrettes, bobby pins or elastic bands may be used for this purpose.
Hair must be kept in such a manner that it does not hang/dangle/fall on a patient
in any way while you are doing an exam.
Hair needs to be styled in an appropriate manner for a professional setting - clean and
well kept.
Facial Hair must be well groomed.
Scrubs
The scrub top must be neatly tucked into the pants, except for the 2 pocket,
vented top. Scrub pants must be hemmed and not touching the floor.
Plain white or black shirts, either short or long sleeves may be worn under the
scrubs.
Coleman College Logo must be permanently adhered to the Scrub top on upper
left (front).

62
Do not wear scrubs prior to approval, if they are not the correct color they will not
be approved.
Lab Jacket
Lab jackets are optional. Some of the clinical sites prefer students to enter and
exit their department with a lab jacket. While working the lab coat may be
removed. Some other clinical sites do not allow students to wear a lab jacket at
any time. Check with your clinical instructor for the clinic requirements where you
are assigned for each semester. No other jackets are to be worn during clinic.
The jacket can be hip length or knee length. The lab jacket must always be
clean, neat, pressed, and free of stains. All rips must be repaired.
The lab jacket must have a Coleman College Logo permanently adhered to the
left sleeve, approximately 2” below the level of the shoulder.
Jewelry
For asepsis and safety, excessive jewelry is not permitted.
A non-smart watch and a ring may be worn.
No large or hoop earrings may be worn (colorful and ornamental earrings are
unacceptable).
No more than two small post earrings may be worn in each ear and only then if
the ears are pierced.
No necklaces are to be worn, except for medical alert tags.
Shoes
Shoes must provide good support.
Shoes and shoestrings must be clean and in good repair.
Only black or white leather athletic shoes may be worn. No other color shoes, or
shoes with fluorescent/bright colors are acceptable
Shoes cannot have holes (professionally or non-professionally manufactured, nor
toe can be out). Clogs must have a strap on the back.
Shoes must be kept clean and free from noticeable scuff marks.
Socks
Socks need to be white or black, at least ankle length and clean.
Clothing must be loose enough to provide ease of movement in clinical activities.
Appropriate undergarments are required.
Colognes
Colognes, perfumes, and any other scent must be non- existent or lightly applied
63
Makeup
Makeup must be minimal; heavy makeup and eye shadow will not be acceptable.
Personal hygiene is very important. Make daily use of baths/showers, soap,
deodorant, lotion, toothpaste, mouthwash, mints (not gum) and anything else that
reduces or keeps mouth and body odor under control.
Tattoos
Tattoos must not be visible and must be covered by long sleeves or any
other appropriate concealment.
ID BADGES
The HCCS student name badge with photo must always be worn on campus.
All students must wear their HCC identification or clinical affiliate issued badge during
clinical rotation.
STUDENT SAFETY
Students are expected to assume responsibility for their own safety by adhering to the
guidelines listed below and discussing with the faculty situations, which the student
believes to be unsafe prior to exposing him/herself to risk.
▪
Student leaving clinical experiences after dark should travel in groups or obtain
escort services from security guards in the agency.
▪
Students who use cars should always lock their doors and park in well-lighted
areas.
▪
Students should carry a minimum amount of money and valuables. Be sure to have
correct change for a phone call and know emergency numbers.
▪
Students should be alert and observant for risks so that suspicious situations can be
avoided. Do not enter a suspicious area - for example, where loitering, fighting or
drunkenness is occurring or in a dark hallway or basement. If the student observes
a suspicious situation, the student should leave immediately.
TRANSPORTATION
Students must provide their own transportation to clinical assignments and costs
incurred during their clinical experiences, including all off-campus expenses. Students
must be able to attend a clinical assignment at any of the clinical affiliates used by the
HCC Radiography Program. Students are responsible for appropriate automobile
insurance coverage. Students are not required to produce evidence of automobile
insurance. However, students are reminded that mandatory auto insurance is a
requirement of the State of Texas.
WEATHER EMERGENCIES
In case of weather conditions that render traveling hazardous, students and faculty
members are urged to exercise their best judgment in determining whether to attend
clinical assignments. The clinical area must be notified promptly by the appropriate

64
person if students or faculty members are going to be absent or late. Information about
changes in HCCS schedules in case of a natural disaster or environmental accident can
be obtained by listening to television news reports.
Students are expected to use their best judgement as to the safety of travel to clinical
especially in cases of inclement weather.
CLINICAL EDUCATION ASSIGNMENTS
The clinical education assignments are assigned by the Department Chair and/or
Clinical Coordinator. Students are not allowed to "switch" with other students after
receiving their clinic assignments. At the end of the semester, the clinical coordinator
will distribute the clinical rotation assignments for the following semester.
Students must have a reliable form of transportation that will enable them to travel to all
the clinical affiliates. Students are required to become familiar with travel and parking
arrangements at the new clinic location before the new assignment begins.
All students must continue to be acceptable to each of the centers.
Some clinical affiliates require that students attend an orientation to learn about their
institution’s mission and policies. If this is a requirement of the clinical site, the student
will be notified in advance and must attend the session prior to starting the clinical
rotation. The student must contact the instructor prior to making any arrangements that
would cause conflicts preventing non-attendance. Documentation will be required.
Students who are removed from clinical education centers for alleged unprofessional
and unethical actions will have a meeting with the Department Chair and Clinical
Coordinator and the Grievance Process will be started. They will not return to clinic until
decisions have been reached regarding the situation. Penalties for removal up to and
including expulsion from the program can occur. The student has the right to Due
Process in these instances.
LEAD MARKERS
Lead (R) and (L) markers are purchased by the student prior to the start of the first
clinical rotation. Students must always have their own lead markers to mark the images
they produce. Sharing or borrowing other student’s markers is not allowed. If markers
are lost or misplaced, they must immediately make efforts to purchase another set.
Students who consistently do not carry their markers will be penalized by not being
allowed to competency test or perform procedures in the clinic or laboratory.
DOSIMETER
The purpose of the dosimeter is to record the amount of radiation received by the body
in a quarterly period. It must be worn whenever a student is in clinic. It is to be worn so
that the name is readable and is to be worn on the collar. Declared pregnant students
wear two devices, one at neck level and one at waist level. When a pregnant student
is assigned to fluoroscopy the waist level device is to be worn under the lead apron
(i.e., in between you and the lead apron) and still at waist level.

65
The program uses the standard clip-on dosimeter. They are provided by Landauer and
distributed by the RSO. Dosimeters are to be turned in or distributed by the fifth of each
new quarter. Dosimeters are not to be lost, left in the sun, left near TV’s or microwaves,
washed, or mutilated in any way. However, if some mishap should occur to your
dosimeter notify the clinical instructor immediately. Dosimeters should remain at the
clinical site near your timecard. If a student, for some reason, fails to have his/her
dosimeter with them they will be assigned to a non-radiation area or be instructed to go
and get it. They will also be penalized for not having it. (See Radiation Safety and
Monitor Policy)
Dosimeter readings will be reviewed and initialed by students while on campus at the
end of each quarter. Reports are kept by the Radiation Safety Officer in a secure
location.
MRI SAFETY
The program requires all active students to review an MRI Safety Screening Protocol in
the first semester. The protocol will include an MRI Safety video, and a patient
screening checklist in the course shown in the didactic course RADR 1301.
PREGNANCY
After a student voluntarily declares pregnancy, she will receive a fetal monitor. The normal
clinic schedule will be followed in accordance with the clinic course syllabus. If the student
feels she cannot meet the objectives for the semester she should speak with the Program
Director about her options. (See Student Pregnancy Policy)
INJURY/SURGERY/ILLNESS
Should a student experience an acute injury/surgery/illness during the Radiography
Program, a release from the student's physician is required before the student may
return to clinic. The release must state the student is able to fully participate in all
the activities stated in the course syllabus without any restrictions.
COMPETENCIES
During each semester each student must demonstrate competency in a specified
number of procedures in the competency-based clinical education plan.
Before a student can competency test (CT) on an exam they must practice that exam,
at least, three times* on actual patients. When the student is prepared, he/she can CT
on the exams practiced if the student achieves 90% or above, they pass the CT. If a
student score below 90% the test will be counted as an attempt** and later, after
practicing on actual exams, the student can retest over that exam.
If a student does not complete the required number of exams in each semester, he/she
must show documentation of "attempting" the required number. Failure to do this will
result in an "F" in clinic. If documentation is satisfied, the student will receive an
incomplete "I" in the course. If this "I" is not corrected, i.e., a grade earned, by the end

66
of the following semester that "I" will become an "F". The clinical instructor (CI) is not
responsible for students who wait until close to the end of the semester to "test out" on
exams that the student could have achieved during the semester. The CI may be out of
the clinic due to meetings, etc. Thus, testing must begin early in the semester. If little
initiative is shown by the student to test out during the semester, this will be noted, and
the student will be in hazard of failing clinic.
*At the discretion of the CI.
TESTING
The majority of a student’s clinical competency testing should be completed with the
clinic instructor. This should be required in most circumstances to allow the clinic
instructor a reasonable amount of certainty about the validity of the student’s
performance on their competency testing.
Each competency test requires the student to answer the instructor’s questions about
anatomy, positioning, pathology, etc., which appears on the images produced during
the competency test. As a result of the patient load and scheduling in the clinics, it is
not always possible for the instructor to complete the film I.D. portion of the test at the
time the test is performed. In circumstances where the film I.D. portion of a
competency test cannot be completed at the time of the test, the student shall be
informed the test must be completed within 5 clinic days or the test will be counted as
an attempt. It is the instructor’s responsibility to monitor this situation and ensure the
test is completed within the 5 clinic days. It is the responsibility of the student to be
prepared, at the time of the test, to answer the instructor’s questions concerning the
anatomy, positioning and other image related questions covered under the film I.D.
portion of the competency test form. It is also the student’s responsibility to ensure the
film I.D. portion of the competency test form is completed within 5 clinic days.
REVIEWING TRAJECSYS
Each student will be expected to make regular appointments with the clinical instructor
concerning progress in clinic. Students must acknowledge all evaluations and competency
exams by electronic signature on Trajecsys weekly. Entering exams and repeated images
is a requirement of each student for all clinical affiliates.
**ATTEMPTS - Only 1 attempt per exam can be documented towards the total number
of attempts tried. To adequately assess a student’s clinical ability, for EACH failed
attempt of a competency examination, a penalty of 10 points will be subtracted from the
raw score of the passed competency exam.

67
READMITTED AND TRANSFER STUDENTS’ COMPETENCY TESTING
Students who are readmitted into the program after being out for 2 semesters must
begin the clinical competency testing from the beginning and must complete the entire
testing process in the time frame they have remaining in the program.
Students who are eligible for transferring into the program will have their
competency exams assessed and approved by the clinical coordinator upon
being assigned to clinic. Competencies counted will be in alignment with students
currently enrolled in that semester
.
RADIOGRAPHY
DIDACTIC AND CLINICAL COMPETENCY REQUIREMENTS
Radiography
1. Introduction
ARRT BOARD APPROVED: JANUARY 2021
EFFECTIVE: JANUARY 2022
Candidates applying for certification and registration under the primary eligibility pathway are required
to meet the Professional Education Requirements specified in the ARRT Rules and Regulations.
ARRT’s Radiography Didactic and Clinical Competency Requirements are one component of the
Professional Education Requirements.
The requirements are periodically updated based upon a practice analysis which is a systematic
process to delineate the job responsibilities typically required of radiographers. The result of this
process is a task inventory which is used to develop the clinical competency requirements (see section
4 below) and the content specifications which serve as the foundation for the didactic competency
requirements (see section 3 below) and the examination.
2. Documentation of Compliance
Verification of program completion, including Didactic and Clinical Competency Requirements and all
degree-related requirements including conferment of the degree, will be completed on the Program
Completion Verification Form on the ARRT Educator Website after the student has completed the
Application for Certification and Registration.
Candidates who complete their educational program during 2022 or 2023 may use either the 2017
Didactic and Clinical Competency Requirements or the 2022 requirements. Candidates who complete
their educational program after December 31, 2023 must use the 2022 requirements.
3. Didactic Competency Requirements
The purpose of the didactic competency requirements is to verify that individuals had the opportunity to
develop fundamental knowledge, integrate theory into practice and hone affective and critical thinking
skills required to demonstrate professional competence. Candidates must successfully complete
coursework addressing the topics listed in the ARRT Content Specifications for the Radiography
Examination. These topics would typically be covered in a nationally-recognized curriculum such as the
ASRT Radiography Curriculum. Educational programs accredited by a mechanism acceptable to ARRT
generally offer education and experience beyond the minimum requirements specified in the content
specifications and clinical competency documents.
4. Clinical Competency Requirements
The purpose of the clinical competency requirements is to verify that individuals certified by the ARRT
have demonstrated competence performing the clinical activities fundamental to a particular discipline.
Competent performance of these fundamental activities, in conjunction with mastery of the cognitive
knowledge and skills covered by the certification examination, provides the basis for the acquisition of
the full range of procedures typically required in a variety of settings. Demonstration of clinical
competence means that the candidate has performed the procedure independently, consistently, and
effectively during the course of his or her formal education. The following pages identify the specific
procedures for the clinical competency requirements. Candidates may wish to use these pages, or their
equivalent, to record completion of the requirements. The pages do NOT need to be sent to the ARRT.
67

RADIOGRAPHY
DIDACTIC AND CLINICAL COMPETENCY REQUIREMENTS
ARRT BOARD APPROVED: JANUARY 2021
EFFECTIVE: JANUARY 2022
4.1
General Performance Considerations
4.1.1
Patient Diversity
Demonstration of competence should include variations in patient characteristics such as age,
gender, and medical condition.
4.1.2
Elements of Competence
Demonstration of clinical competence requires that the program director or the program
director’s designee has observed the candidate performing the procedure independently,
consistently, and effectively during the course of the candidate’s formal educational program.
4.1.3
Simulated Performance
ARRT defines simulation of a clinical procedure routinely performed on a patient as the
candidate completing all possible hands-on tasks of the procedure on a live human being
using the same level of cognitive, psychomotor, and affective skills required for performing
the procedure on a patient.
ARRT requires that competencies performed as a simulation must meet the same criteria as
competencies demonstrated on patients. For example, the competency must be performed
under the direct observation of the program director or program director’s designee and be
performed independently, consistently, and effectively.
Simulated performance must meet the following criteria:
ï
Simulation of imaging procedures requires the use of proper radiographic equipment
without activating the x-ray beam.
ï
A total of ten imaging procedures may be simulated. Imaging procedures eligible for
simulation are noted within the chart (see section 4.2.2).
ï
If applicable, the candidate must evaluate related images.
ï
Some simulations are acceptable for General Patient Care (see section 4.2.1). These
do not count toward the ten imaging procedures that can be simulated.
4.2
Radiography-Specific Requirements
As part of the education program, candidates must demonstrate competence in the clinical
procedures identified below. These clinical procedures are listed in more detail in the following
sections:
ï
Ten mandatory general patient care procedures;
ï
36 mandatory imaging procedures;
ï
15 elective imaging procedures selected from a list of 34 procedures;
ï
One of the 15 elective imaging procedures must be selected from the head section; and
ï
Two of the 15 elective imaging procedures must be selected from the fluoroscopy studies
section.
One patient may be used to document more than one competency. However, each individual
procedure may be used for only one competency (e.g., a portable femur can only be used for
a portable extremity or a femur but not both).
68

RADIOGRAPHY
DIDACTIC AND CLINICAL COMPETENCY REQUIREMENTS
4.2.1
General Patient Care Procedures
ARRT BOARD APPROVED: JANUARY 2021
EFFECTIVE: JANUARY 2022
Candidates must be CPR/BLS certified and have demonstrated competence in the remaining
nine patient care procedures listed below. The procedures should be performed on patients
whenever possible, but simulation is acceptable if state regulations or institutional practice
prohibits candidates from performing the procedures on patients.
General Patient Care Procedures
Date
Completed
Competence
Verified By
CPR/BLS Certified
Vital Signs – Blood Pressure
Vital Signs – Temperature
Vital Signs – Pulse
Vital Signs – Respiration
Vital Signs – Pulse Oximetry
Sterile and Medical Aseptic Technique
Venipuncture*
Assisted Patient Transfer (e.g., Slider Board, Mechanical Lift,
Gait Belt)
Care of Patient Medical Equipment (e.g., Oxygen Tank,
IV Tubing)
*Venipuncture can be simulated by demonstrating aseptic technique on another person, but then
inserting the needle into an artificial forearm or suitable device.
4.2.2
Imaging Procedures
Institutional protocol will determine the positions and projections used for each procedure.
When performing imaging procedures, the candidate must independently demonstrate
appropriate:
ï
patient identity verification;
ï
examination order verification;
ï
patient assessment;
ï
room preparation;
ï
patient management;
ï
equipment operation;
ï
technique selection;
ï
patient positioning;
ï
radiation safety;
ï
image processing; and
ï
image evaluation.
ï
69

RADIOGRAPHY
DIDACTIC AND CLINICAL COMPETENCY REQUIREMENTS
4.2.2 Imaging Procedures (continued)
ARRT BOARD APPROVED: JANUARY 2021
EFFECTIVE: JANUARY 2022
Imaging Procedures
Mandatory or Elective
Eligible
for
Simulation
Date
Completed
Competence
Verified By
Mandatory
Elective
Chest and Thorax
Chest Routine
✓
Chest AP (Wheelchair or Stretcher)
✓
Ribs
✓
✓
Chest Lateral Decubitus
✓
✓
Sternum
✓
✓
Upper Airway (Soft-Tissue Neck)
✓
✓
Sternoclavicular Joints
✓
✓
Upper Extremity
Thumb or Finger
✓
✓
Hand
✓
Wrist
✓
Forearm
✓
Elbow
✓
Humerus
✓
✓
Shoulder
✓
Clavicle
✓
✓
Scapula
✓
✓
AC Joints
✓
✓
Trauma: Shoulder or Humerus
(Scapular Y, Transthoracic or Axial)*
✓
Trauma: Upper Extremity (Non-Shoulder)*
✓
Lower Extremity
Toes
✓
✓
Foot
✓
Ankle
✓
Knee
✓
Tibia-Fibula
✓
✓
Femur
✓
✓
Patella
✓
✓
Calcaneus
✓
✓
Trauma: Lower Extremity*
✓
* Trauma requires modifications in positioning due to injury with monitoring of the patient’s condition.
70

RADIOGRAPHY
DIDACTIC AND CLINICAL COMPETENCY REQUIREMENTS
4.2.2 Imaging Procedures (continued)
ARRT BOARD APPROVED: JANUARY 2021
EFFECTIVE: JANUARY 2022
Imaging Procedures
Mandatory or Elective
Eligible
for
Simulation
Date
Completed
Competence
Verified By
Mandatory
Elective
Head – Candidates must select at least one
elective procedure from this section.
Skull
✓
✓
Facial Bones
✓
✓
Mandible
✓
✓
Temporomandibular Joints
✓
✓
Nasal Bones
✓
✓
Orbits
✓
✓
Paranasal Sinuses
✓
✓
Spine and Pelvis
Cervical Spine
✓
Thoracic Spine
✓
✓
Lumbar Spine
✓
Cross-Table (Horizontal Beam)
Lateral Spine (Patient Recumbent)
✓
✓
Pelvis
✓
Hip
✓
Cross-Table (Horizontal Beam)
Lateral Hip (Patient Recumbent)
✓
✓
Sacrum and/or Coccyx
✓
✓
Scoliosis Series
✓
✓
Sacroiliac Joints
✓
✓
Abdomen
Abdomen Supine
✓
Abdomen Upright
✓
✓
Abdomen Decubitus
✓
✓
Intravenous Urography
✓

6
V 2021.05.03
RADIOGRAPHY
DIDACTIC AND CLINICAL COMPETENCY REQUIREMENTS
4.2.2 Imaging Procedures (continued)
ARRT BOARD APPROVED: JANUARY 2021
EFFECTIVE: JANUARY 2022
Imaging Procedures
Mandatory or Elective
Eligible
for
Simulation
Date
Completed
Competence
Verified By
Mandatory
Elective
Fluoroscopy Studies – Candidates must
select two procedures from this section and
perform per site protocol.
Upper GI Series, Single or Double
Contrast
✓
Contrast Enema, Single or Double
Contrast
✓
Small Bowel Series
✓
Esophagus (NOT Swallowing Dysfunction
Study)
✓
Cystography/Cystourethrography
✓
ERCP
✓
Myelography
✓
Arthrography
✓
Hysterosalpingography
✓
Mobile C-Arm Studies
C-Arm Procedure (Requiring Manipulation
to Obtain More Than One Projection)
✓
✓
Surgical C-Arm Procedure (Requiring
Manipulation Around a Sterile Field)
✓
✓
Mobile Radiographic Studies
Chest
✓
Abdomen
✓
Upper or Lower Extremity
✓
Pediatric Patient (Age 6 or Younger)
Chest Routine
✓
✓
Upper or Lower Extremity
✓
✓
Abdomen
✓
✓
Mobile Study
✓
✓
Geriatric Patient (At Least 65 Years Old and
Physically or Cognitively Impaired as a Result of
Aging)
Chest Routine
✓
Upper or Lower Extremity
✓
Hip or Spine
✓
Subtotal
Total Mandatory exams required
36
Total Elective exams required
15
Total number of simulations allowed
10

73
APPENDIX A
APPLICATION FOR RE-ADMISSION TO
THE RADIOGRAPHY PROGRAM
74
APPLICATION FOR READMISSION TO THE RADIOGRAPHY PROGRAM
HOUSTON COMMUNITY COLLEGE SYSTEM
1900 Pressler St.
Houston, Texas 77030
(713) 718-7588
PLEASE COMPLETE THIS APPLICATION AND SUBMIT DIRECTLY TO THE
RADIOGRAPHY PROGRAM.
NAME:
(Last) (First) (M.I./Maiden)
SOCIAL SECURITY NO.
CURRENT MAILING ADDRESS:
(Street) (Apt. #)
(City) (State) (Zip)
TELEPHONE: (Home) (Work)
EMAIL ADDRESS:
YEAR AND SEMESTER ORIGINALLY ENROLLED:
YEAR AND SEMESTER STUDENT WITHDREW/STOPPED OUT/FAILED OUT:
APPLYING TO REENTER: YEAR:
SEMESTER: Fall Spring Summer
For Office Use Only:
Date
Rec.
Prog.
Code:

75
Page 2- APPLICATION FOR READMISSION
This Form Must Be Completed in Order to Be Considered for Readmission
Name: Date:
1. Please Check the Appropriate Reason for Withdrawal from The Radiography
Program
Academic Failure Personal Financial Not for me
2. Check those problems or weaknesses that prevented you from being successful
in the program.
Study Skills Job Family Other
If you checked “Other”, please explain.
3 List actions that you took from the recommendations given to you during your exit
interview.
Important Note:
I certify that all the information provided in this application and attachments as
complete and accurate. I understand the submission of this application does not
guarantee my readmission to the program.
Signature Date

76
APPENDIX B
NRC PUBLICATION
77
U.S. Nuclear Regulatory Commission
Regulatory Guide 8.13 -Instruction
Concerning Prenatal RadiationExposure
(Draft was issued as DG-8014)
Revision 3
June 1999
Availability Notice
A. INTRODUCTION
The Code of Federal Regulations in 10 CFR Part 19, "Notices, Instructions and Reports to
Workers: Inspection and Investigations," in Section 19.12, "Instructions to Workers," requires
instruction in "the health protection problems associated with exposure to radiation and/or
radioactive material, in precautions or procedures to minimize exposure, and in the purposes and
functions of protective devices employed." The instructions must be "commensurate with potential
radiological health protection problems present in the workplace."
The Nuclear Regulatory Commission's (NRC's) regulations on radiation protection are specified in
10 CFR Part 20, "Standards for Protection against Radiation"; and Section 20.1208, "Dose to an
Embryo/Fetus," requires licensees to "ensure that the dose to an embryo/fetus during the entire
pregnancy, due to occupational exposure of a declared pregnant woman, does not exceed 0.5
rem (5 mSv)." Section 20.1208 also requires licensees to "make efforts to avoid substantial
variation above a uniform monthly exposure rate to a declared pregnant woman." A declared
pregnant woman is defined in 10 CFR 20.1003 as a woman who has voluntarily informed her
employer, in writing, of her pregnancy and the estimated date of conception.
This regulatory guide is intended to provide information to pregnant women, and other personnel,
to help them make decisions regarding radiation exposure during pregnancy. This Regulatory
Guide 8.13 supplements Regulatory Guide 8.29, "Instruction Concerning Risks from Occupational
Radiation Exposure" (Ref. 1), which contains a broad discussion of the risks from exposure to
ionizing radiation.
Other sections of the NRC's regulations also specify requirements for monitoring external and
internal occupational dose to a declared pregnant woman. In 10 CFR 20.1502, "Conditions
Requiring Individual Monitoring of External and Internal Occupational Dose," licensees are
78
required to monitor the occupational dose to a declared pregnant woman, using an individual
monitoring device, if it is likely that the declared pregnant woman will receive, from external
sources, a deep dose equivalent more than 0.1 rem (1 mSv). According to Paragraph (e) of 10
CFR 20.2106, "Records of Individual Monitoring Results," the licensee must maintain records of
dose to an embryo/fetus if monitoring was required, and the records of dose to the embryo/fetus
must be kept with the records of dose to the declared pregnant woman. The declaration of
pregnancy must be kept on file but may be maintained separately from the dose records. The
licensee must retain the required form or record until the Commission terminates each pertinent
license requiring the record.
The information collections in this regulatory guide are covered by the requirements of 10 CFR
Parts 19 or 20, which were approved by the Office of Management and Budget, approval
numbers 3150-0044 and 3150-0014, respectively. The NRC may not conduct or sponsor, and a
person is not required to respond to, a collection of information unless it displays a currently valid
OMB control number.
B. DISCUSSION
As discussed in Regulatory Guide 8.29 (Ref. 1), exposure to any level of radiation is assumed to
carry with it a certain amount of risk. In the absence of scientific certainty regarding the
relationship between low dose exposure and health effects, and as a conservative assumption for
radiation protection purposes, the scientific community generally assumes that any exposure to
ionizing radiation may cause undesirable biological effects and that the likelihood of these effects
increases as the dose increases. At the occupational dose limit for the whole body of 5 rem
(50 mSv) per year, the risk is believed to be very low.
The magnitude of risk of childhood cancer following in utero exposure is uncertain in that both
negative and positive studies have been reported. The data from these studies "are consistent
with a lifetime cancer risk resulting from exposure during gestation which is two to three times
that for the adult" (NCRP Report No. 116, Ref. 2). The NRC has reviewed the available scientific
literature and has concluded that the 0.5 rem (5 mSv) limit specified in 10 CFR 20.1208 provides
an adequate margin of protection for the embryo/fetus. This dose limit reflects the desire to limit
the total lifetime risk of leukemia and other cancers associated with radiation exposure during
pregnancy.
For a pregnant worker to take advantage of the lower exposure limit and dose monitoring
provisions specified in 10 CFR Part 20, the woman must declare her pregnancy in writing to the
licensee. A form letter for declaring pregnancy is provided in this guide or the licensee may use
its own form letter for declaring pregnancy. A separate written declaration should be submitted for
each pregnancy.
C. REGULATORY POSITION
1.
Who Should Receive Instruction?
Female workers who require training under 10 CFR 19.12 should be provided with the
information contained in this guide. In addition to the information contained in Regulatory
Guide 8.29 (Ref. 1), this information may be included as part of the training required
under 10 CFR 19.12.
2.
Providing Instruction
The occupational worker may be given a copy of this guide with its Appendix, an
explanation of the contents of the guide, and an opportunity to ask questions and request
additional information. The information in this guide and Appendix should also be
provided to any worker or supervisor who may be affected by a declaration of pregnancy
or who may have to take some action in response to such a declaration.,
79
Classroom instruction may supplement the written information. If the licensee provides
classroom instruction, the instructor should have some knowledge of the biological
effects of radiation to be able to answer questions that may go beyond the information
provided in this guide. Videotaped presentations may be used for classroom instruction.
Regardless of whether the licensee provides classroom training, the licensee should give
workers the opportunity to ask questions about information contained in this Regulatory
Guide 8.13. The licensee may take credit for instruction that the worker has received
within the past year at other licensed facilities or in other courses or training.
3.
Licensee's Policy on Declared Pregnant Women
The instruction provided should describe the licensee's specific policy on declared
pregnant women, including how those policies may affect a woman's work situation. In
particular, the instruction should include a description of the licensee's policies, if any,
that may affect the declared pregnant woman's work situation after she has filed a written
declaration of pregnancy consistent with 10 CFR 20.1208.
The instruction should also identify who to contact for additional information as well as
identify who should receive the written declaration of pregnancy. The recipient of the
woman's declaration may be identified by name (e.g., John Smith), position (e.g.,
immediate supervisor, the radiation safety officer), or department (e.g., the personnel
department).
4.
Duration of Lower Dose Limits for the Embryo/Fetus
The lower dose limit for the embryo/fetus should remain in effect until the woman
withdraws the declaration in writing or the woman is no longer pregnant. If a declaration
of pregnancy is withdrawn, the dose limit for the embryo/fetus would apply only to the
time from the estimated date of conception until the time the declaration is withdrawn. If
the declaration is not withdrawn, the written declaration may be considered expired one
year after submission.
5.
Substantial Variations Above a Uniform Monthly Dose Rate
According to 10 CFR 20.1208(b), "The licensee shall make efforts to avoid substantial
variation above a uniform monthly exposure rate to a declared pregnant woman so as to
satisfy the limit in paragraph (a) of this section," that is, 0.5 rem (5 mSv) to the
embryo/fetus. The National Council on Radiation Protection and Measurements (NCRP)
recommends a monthly equivalent dose limit of 0.05 rem (0.5 mSv) to the embryo/fetus
once the pregnancy is known (Ref. 2). In view of the NCRP recommendation, any
monthly dose of less than 0.1 rem (1 mSv) may be considered as not a substantial
variation above a uniform monthly dose rate and as such will not require licensee
justification. However, a monthly dose greater than 0.1 rem (1 mSv) should be justified by
the licensee.
D. IMPLEMENTATION
The purpose of this section is to provide information to licensees and applicants regarding the
NRC staff's plans for using this regulatory guide.
Unless a licensee or an applicant proposes an acceptable alternative method for complying with
the specified portions of the NRC's regulations, the methods described in this guide will be used
80
by the NRC staff in the evaluation of instructions to workers on the radiation exposure of pregnant
women.
REFERENCES
1.
USNRC, "Instruction Concerning Risks from Occupational Radiation Exposure,"
Regulatory Guide 8.29, Revision 1, February 1996.
2.
National Council on Radiation Protection and Measurements, Limitation of
Exposure to Ionizing Radiation, NCRP Report No. 116, Bethesda, MD, 1993.
APPENDIX: QUESTIONS AND ANSWERS
CONCERNING PRENATAL RADIATION
EXPOSURE
1. Why am I receiving this information?
The NRC's regulations (in 10 CFR 19.12, "Instructions to Workers") require that licensees
instruct individuals working with licensed radioactive materials in radiation protection as
appropriate for the situation. The instruction below describes information that occupational
workers and their supervisors should know about the radiation exposure of the embryo/fetus
of pregnant women.
The regulations allow a pregnant woman to decide whether she wants to formally declare her
pregnancy to take advantage of lower dose limits for the embryo/fetus. This instruction
provides information to help women make an informed decision whether to declare a
pregnancy.
2. If I become pregnant, am I required to declare my pregnancy?
No. The choice whether to declare your pregnancy is completely voluntary. If you choose to
declare your pregnancy, you must do so in writing and a lower radiation dose limit will apply
to your embryo/fetus. If you choose not to declare your pregnancy, you and your
embryo/fetus will continue to be subject to the same radiation dose limits that apply to other
occupational workers.
3. If I declare my pregnancy in writing, what happens?
If you choose to declare your pregnancy in writing, the licensee must take measures to limit
the dose to your embryo/fetus to 0.5 rem (5 millisievert) during the entire pregnancy. This is
one-tenth of the dose that an occupational worker may receive in a year. If you have already
received a dose exceeding 0.5 rem (5 mSv) in the period between conception and the
declaration of your pregnancy, an additional dose of 0.05 rem (0.5 mSv) is allowed during the
remainder of the pregnancy. In addition, 10 CFR 20.1208, "Dose to an Embryo/Fetus,"
requires licensees to make efforts to avoid substantial variation above a uniform monthly
dose rate so that all the 0.5 rem (5 mSv) allowed dose does not occur in a short period during
the pregnancy.
This may mean that, if you declare your pregnancy, the licensee may not permit you to do
some of your normal job functions if those functions would have allowed you to receive more
than 0.5 rem, and you may not be able to have some emergency response responsibilities.
Why do the regulations have a lower dose limit for the embryo/fetus of a declared pregnant?
4. woman than for a pregnant worker who has not declared.
81
A lower dose limit for the embryo/fetus of a declared pregnant woman is based on a
consideration of greater sensitivity to radiation of the embryo/fetus and the involuntary nature
of the exposure. Several scientific advisory groups have recommended (References 1 and 2)
that the dose to the embryo/fetus be limited to a fraction of the occupational dose limit.
5. What are the potentially harmful effects of radiation exposure to my embryo/fetus?
The occurrence and severity of health effects caused by ionizing radiation are dependent
upon the type and total dose of radiation received, as well as the time over which the
exposure was received. See Regulatory Guide 8.29, "Instruction Concerning Risks from
Occupational Exposure" (Ref. 3), for more information. The main concern is embryo/fetal
susceptibility to the harmful effects of radiation such as cancer.
6. Are there any risks of genetic defects?
Although radiation injury has been induced experimentally in rodents and insects, and in the
experiments was transmitted and became manifest as hereditary disorders in their offspring,
radiation has not been identified as a cause of such effect in humans. Therefore, the risk of
genetic effects attributable to radiation exposure is speculative. For example, no genetic
effects have been documented in any of the Japanese atomic bomb survivors, their children,
or their grandchildren.
7. What if I decide that I do not want any radiation exposure at all during my pregnancy?
You may ask your employer for a job that does not involve any exposure at all to
occupational radiation dose, but your employer is not obligated to provide you with a job
involving no radiation exposure. Even if you receive no occupational exposure at all, your
embryo/fetus will receive some radiation dose (on average 75 mrem (0.75 mSv)) during your
pregnancy from natural background radiation.
The NRC has reviewed the available scientific literature and concluded that the 0.5 rem (5
mSv) limit provides an adequate margin of protection for the embryo/fetus. This dose limit
reflects the desire to limit the total lifetime risk of leukemia and other cancers. If this dose limit
is exceeded, the total lifetime risk of cancer to the embryo/fetus may increase incrementally.
However, the decision on what level of risk to accept is yours. More detailed information on
potential risk to the embryo/fetus from radiation exposure can be found in References 2-10.
8. What effect will formally declaring my pregnancy have on my job status?
Only the licensee can tell you what effect a written declaration of pregnancy will have on your
job status. As part of your radiation safety training, the licensee should tell you the company's
policies with respect to the job status of declared pregnant women. In addition, before you
declare your pregnancy, you may want to talk to your supervisor or your radiation safety
officer and ask what a declaration of pregnancy would mean specifically for you and your job
status.
82
In many cases you can continue in your present job with no change and still meet the dose
limit for the embryo/fetus. For example, most commercial power reactor workers
(approximately 93%) receive, in 12 months, occupational radiation doses that are less than
0.5 rem (5 mSv) (Ref. 11). The licensee may also consider the likelihood of increased
radiation exposures from accidents and abnormal events before deciding to allow you to
continue in your present job.
If your current work might cause the dose to your embryo/fetus to exceed 0.5 rem (5 mSv),
the licensee has various options. It is possible that the licensee can and will make a
reasonable accommodation that will allow you to continue performing your current job, for
example, by having another qualified employee do a small part of the job that accounts for
some of your radiation exposure.
9. What information must I provide in my written declaration of pregnancy?
You should provide, in writing, your name, a declaration that you are pregnant, the estimated
date of conception (only the month and year need be given), and the date that you give the
letter to the licensee. A form letter that you can use is included at the end of these questions
and answers. You may use that letter, use a form letter the licensee has provided to you, or
write your own letter.
10.
To declare my pregnancy, do I have to have documented medical proof that I am pregnant?
NRC regulations do not require that you provide medical proof of your pregnancy. However,
NRC regulations do not preclude the licensee from requesting medical documentation of your
pregnancy, especially if a change in your duties is necessary to comply with the 0.5 rem (5
mSv) dose limit.
11. Can I tell the licensee orally rather than in writing that I am pregnant?
No. The regulations require that the declaration must be in writing.
12. If I have not declared my pregnancy in writing, but the licensee suspects that I am pregnant,
do the lower dose limits apply?
No. The lower dose limits for pregnant women apply only if you have declared your
pregnancy in writing. The United States Supreme Court has ruled (in United Automobile
Workers International Union v. Johnson Controls, Inc., 1991) that "Decisions about the
welfare of future children must be left to the parents who conceive, bear, support, and raise
them rather than to the employers who hire those parents" (Reference 7). The Supreme
Court also ruled that your employer may not restrict you from a specific job "because of
concerns about the next generation." Thus, the lower limits apply only if you choose to
declare your pregnancy in writing.
If I am planning to become pregnant but am not yet pregnant and I inform the licensee of that
13. in writing, do the lower dose limits apply?
No. The requirement for lower limits applies only if you declare in writing that you are already
pregnant.
14. What if I have a miscarriage or find out that I am not pregnant?
83
If you have declared your pregnancy in writing, you should promptly inform the licensee in
writing that you are no longer pregnant. However, if you have not formally declared your
pregnancy in writing, you need not inform the licensee of your non-pregnant status.
15. How long is the lower dose limit in effect?
The dose to the embryo/fetus must be limited until you withdraw your declaration in writing, or
you inform the licensee in writing that you are no longer pregnant. If the declaration is not
withdrawn, the written declaration may be considered expired one year after submission.
If I have declared my pregnancy in writing, can I revoke my declaration of pregnancy even if I
16. am still pregnant?
Yes, you may. The choice is entirely yours. If you revoke your declaration of pregnancy, the
lower dose limit for the embryo/fetus no longer applies.
17. What if I work under contract at a licensed facility?
The regulations state that you should formally declare your pregnancy to the licensee in
writing. The licensee has the responsibility to limit the dose to the embryo/fetus.
18. Where can I get additional information?
The references to this Appendix contain helpful information, especially Reference 3, NRC's
Regulatory Guide 8.29, and “Instruction Concerning Risks from Occupational Radiation
Exposure," for general information on radiation risks. The licensee should be able to give this
document to you.
For information on legal aspects, see Reference 7, "The Rock and the Hard Place: Employer
Liability to Fertile or Pregnant Employees and Their Unborn Children--What Can the Employer
Do?" which is an article in the journal Radiation Protection Management.
You may telephone the NRC Headquarters at (301) 415-7000. Legal questions should be
directed to the Office of the General Counsel, and technical questions should be directed to the
Division of Industrial and Medical Nuclear Safety.
You may also telephone the NRC Regional Offices at the following numbers: Region I, (610) 337-
5000; Region II, (404) 562-4400; Region III, (630) 829-9500; and Region IV, (817) 860-8100.
Legal questions should be directed to the Regional Counsel, and technical questions should be
directed to the Division of Nuclear Materials Safety.
REFERENCES FOR APPENDIX
A. National Council on Radiation Protection and Measurements, Limitation of Exposure to Ionizing
Radiation, NCRP Report No. 116, Bethesda, MD, 1993.
B. International Commission on Radiological Protection, 1990 Recommendations of the International
Commission on Radiological Protection, ICRP Publication 60, Ann. ICRP 21: No. 1-3, Pergamon
Press, Oxford, UK, 1991.
C. USNRC, "Instruction Concerning Risks from Occupational Radiation Exposure," Regulatory
Guide 8.29, Revision 1, February 1996.
(1)
(Electronically available at
http://www.nrc.gov/reading- rm/doc-collections/reg-guides/)
83
D. Committee on the Biological Effects of Ionizing Radiations, National
Research Council, Health Effects of Exposure to Low Levels of Ionizing
Radiation (BEIR V), National Academy Press, Washington, DC, 1990.
E. United Nations Scientific Committee on the Effects of Atomic Radiation,
Sources and Effects of Ionizing Radiation, United Nations, New York,
1993.
F. R. Doll and R. Wakeford, "Risk of Childhood Cancer from Fetal
Irradiation," The British Journal of Radiology, 70, 130-139, 1997.
G. David Wiedis, Donald E. Jose, and Timm O. Phoebe, "The Rock and the
Hard Place: Employer Liability to Fertile or Pregnant Employees and Their
Unborn Children--What Can the Employer Do?" Radiation Protection
Management, 11, 41-49, January/February 1994.
H. National Council on Radiation Protection and Measurements,
Considerations Regarding the Unintended Radiation Exposure of the
Embryo, Fetus, or Nursing Child, NCRP Commentary No. 9, Bethesda,
MD, 1994.
I. National Council on Radiation Protection and Measurements, Risk
Estimates for Radiation Protection, NCRP Report No. 115, Bethesda, MD,
1993.
J. National Radiological Protection Board, Advice on Exposure to Ionizing
Radiation During Pregnancy, National Radiological Protection Board,
Chilton, Didcot, UK, 1998.
REGULATORY ANALYSIS
A separate regulatory analysis was not prepared for this regulatory guide. A regulatory
analysis prepared for 10 CFR Part 20, "Standards for Protection Against Radiation" (56
FR 23360), provides the regulatory basis for this guide and examines the costs and
benefits of the rule as implemented by the guide. A copy of the "Regulatory Analysis for
the Revision of 10 CFR Part 20" (PNL-6712, November 1988) is available for inspection
and copying for a fee at the NRC Public Document Room, 2120 L Street NW,
Washington, DC, as an enclosure to Part 20 (56 FR 23360).
1. Single copies of regulatory guides, both active and draft, and draft NUREG documents may be
obtained free of charge by writing the Reproduction and Distribution Services Section, OCIO,
USNRC, Washington, DC 20555-0001, or by fax to (301)415-2289, or by email to
(DISTRIBUTION@NRC.GOV). Active guides may also be purchased from the National Technical
Information Service on a standing order basis. Details on this service may be obtained by writing
NTIS, 5285 Port Royal Road, Springfield, VA 22161. Copies of active and draft guides are
available for inspection or copying for a fee from the NRC Public Document Room at 2120 L
Street NW., Washington, DC; the PDR's mailing address is Mail Stop LL-6, Washington, DC
20555; telephone (202)634-3273; fax (202)634-3343.
2. Copies are available at current rates from the U.S. Government Printing Office, P.O. Box
37082, Washington, DC 20402-9328 (telephone (202)512-1800); or from the National Technical
Information Service by writing NTIS at 5285 Port Royal Road, Springfield, VA 22161. Copies are
available for inspection or copying for a fee from the NRC Public Document Room at 2120 L
Street NW., Washington, DC; the PDR's mailing address is Mail Stop LL-6, Washington, DC
20555; telephone (202)634-3273; fax (202)634-3343

84
APPENDIX C
FORM LETTER FOR VOLUNTARILY DECLARING
PREGNANCY
This form is provided for your convenience. To make your written declaration of pregnancy,
you may fill in the blanks in this form letter, or you may write your own letter.
VOLUNTARY DECLARATION OF PREGNANCY
To: ,
In accordance with the NRC's regulations at 10 CFR 20.1208, "Dose to an Embryo/Fetus," I am
voluntarily declaring that I am pregnant. I believe I became pregnant in (only the month
and year need be provided).
I understand the radiation dose to my embryo/fetus during my entire pregnancy will not be
allowed to exceed 0.5 rem (5 millisievert) (unless that dose has already been exceeded between
the time of conception and submitting this letter). I also understand that meeting the lower dose
limit may require a change in job or job responsibilities during my pregnancy.
Printed Name: Signature: Date: _ _
(Student Technologist)
Printed Name: Signature: Date: _ _
(Radiation Safety Officer)
Printed Name: Signature: Date: _ _
(Program Director)

85
APPENDIX C
FORM LETTER FOR PREGNANCY DECLARATION
WITHDRAWAL
This form letter is provided for your convenience. To make your written declaration of
pregnancy void, you may fill in the blanks in this form letter.
WITHDRAWAL OF DECLARATION OF PREGNANCY
To: ,
I am withdrawing my previous declaration of pregnancy in writing. I understand that by
submitting this form I agree to the removal of additional dosimeters and any pregnancy related
responsibilities to the radiography program.
Printed Name: Signature: Date: _ _
(Student Technologist)
Printed Name: Signature: Date: _ _
(Radiation Safety Officer)
Printed Name: Signature: Date: _ _
(Program Director)

86
APPENDIX D
GRADE APPEAL PROCESS
87
PURPOSE
The purpose of the Course Grade Appeal Process is to provide students a
safeguard against receiving an unfair final course grade while also respecting the
academic responsibility of the instructor and academic standards of Houston
Community College. The College must follow clear and consistent guidelines for
all grade appeals. It is the responsibility of all HCC faculty to evaluate each
student’s work fairly and to assign a grade which is an impartial measure of the
student’s achievement in the course. In the event of a dispute over an assigned
final course grade, students should be provided the opportunity, within certain
guidelines outlined in the HCC Course Grade Appeal Process, to formally
present a case and rationale for a grade appeal which will be evaluated using a
fair and consistent review process.
This process is in accordance with the following SACSCOC Federal
Requirements:
“4.3 The institution makes available to students and the public current academic
calendars, grading policies, and refund policies.”
“4.5 The institution has adequate procedures for addressing written student
complaints and is responsible for demonstrating that it follows those procedures
when resolving student complaints.”
APPLICABILITY
The Course Grade Appeal Process applies to all programs throughout the HCC district.
DEFINITIONS
Bias: A particular tendency, trend, inclination, feeling, or opinion, especially one that is
preconceived or unreasoned. An unfair personal opinion that influences one’s judgment.
Caprice: a tendency to change one’s mind without apparent or adequate motive.
Business days: Every official working day of the week at HCC. Typically, they include days
between Monday and Friday and do not include HCC-approved holidays or weekends.
Communication: For the purposes of this process, communicate in writing between the
student, instructor, panel chair, or department chair/dean/COE dean via HCC email account
and/or the student contact information provided on the Grade Appeal Form).
88
Retention period: the minimum time that a local government record must be retained as
established on a records retention schedule accepted for filing by the Texas State Library and
Archives Commission.
PROCEDURES
Introduction
Grade determination and awarding of all grades in a course is the responsibility of the
instructor. If a student believes a grade was awarded on an assessment in a capricious or
arbitrary manner while a course is in progress, the student should discuss the matter with the
instructor. This Course Grade Appeal Process only applies to final course grades. A student’s
final course grade can be changed only at the discretion of the instructor or as a result of this
Course Grade Appeal Process. A student may appeal a final course grade if he/she is able to
demonstrate that an inappropriate grade was assigned as a result of:
Bias
Caprice
Or other improper conditions such as computational error.
Other reasons for changing final grades will not constitute a valid appeal. The burden of proof
is on the student to justify the basis for changing the grade.
Note: In cases of a grade dispute regarding alleged academic dishonesty, a separate process
will be followed (see Academic Dishonesty section of the Student Handbook).
The Grade Appeal Process is comprised of the following progressive levels to provide due
process for the student:
Informal Resolution
Formal Appeal
Grade Appeals Panel
Appealing the Panel’s Decision
Resolution may be reached at various points throughout the
process outlined below:
Level 1: Informal Resolution
Whenever possible, students should attempt to resolve grade disputes informally with the
instructor as this allows for the potential of immediate resolution.
After meeting with the instructor, if the student remains dissatisfied, the student should notify
89
the appropriate department chair of the grade dispute. If there is no chair assigned to that
program, the appeal should be made to the appropriate dean. The chair/dean/COE dean shall
attempt to resolve the matter informally through consultation with the instructor. If informal
resolution is not obtained through mediation at that level, the grade dispute is consigned to the
process of a formal appeal.
Level 2: Formal Appeal
Student grievances which are consigned to a formal appeal must be specified in writing using
the Student Course Grade Appeal Form. It is recommended that the Authorization to Release
Information for Course Grade Appeal FERPA Release Form also be submitted at the same
time by the student filing the appeal.
These forms must be submitted to the department chair/dean/COE dean no later than fifteen
(15) business days from the day the grade was officially posted by HCC.
The department chair/dean/COE dean will review the student grievant’s appeal to determine if
appeal criteria have or have not been met. Again, the student must demonstrate that an
inappropriate grade was assigned as a result of bias, caprice, or other improper conditions
such as computational error. The instructor may submit a written response to the appeal. The
decision of the department chair/dean/COE dean will be communicated in writing to the
student (via their HCC email account and/or the contact information provided on the Grade
Appeal Form submitted) and to the instructor within ten (10) business days of receipt of these
forms. The email will notify the student grievant whether or not the department chair/dean/COE
dean finds grounds for a grade appeal. That email will also notify the student that, if they do
not accept the decision of the department chair/dean/COE dean, then he/she has five (5)
business days from that notification to request a Grade Appeals Panel to review the case. If
no response is received from the student within five (5) business days, the appeal is closed.
Level 3: Grade Appeals Panel
If the student requests a Grade Appeals Panel, the Panel will render its decision no later than
twenty (20) business days following receipt of that request. In rare cases, such as when
faculty are not on contract, no more than twenty (20) additional business days may be allotted.
A Grade Appeals Panel consists of at least two full-time instructors from the instructional area
involved or a related instructional program as well as one student panelist independent of the
class or program associated with the appeal. The entire Grade Appeals Panel, including the
student panelist, will be selected by the department chair/dean/COE dean. The student
panelist will be selected from the current Student Government Association leadership, or
membership if an elected SGA leader is not available.
All proceedings and information discussed in the Grade Appeal Process are confidential.
The Grade Appeals Panel will select a chair. The student panelist cannot serve as chair.
Upon appointment, the student panelist is required to sign the Acknowledgement of
Confidentiality and Non-Disclosure of Protected Student Information - HERE Panel members
shall neither engage in any independent investigation outside of the hearing nor consider any
information obtained outside of the panel’s deliberations or hearings. The instructor who
assigned the disputed grade cannot serve as a member of the Grade Appeals Panel, however,
90
may submit a written response to the appeal. Both the student grievant and the instructor
have the right to appear in person before the Grade Appeals Panel. The student grievant and
instructor shall represent him/herself, but either may be accompanied by another individual,
who must be identified in advance of the panel hearing. Neither additional individual is
permitted to address the panel. The panel can interview others who they determine may have
relevant information. When both student and instructor appear before the panel, they should
be afforded access to each other’s submitted documentation. Interviews with both the student
and instructor should be conducted separately If neither party appears in person, the panel
should complete its review based on the written materials submitted. The panel shall consider
all aspects of the case before making its decision.
No more than five (5) business days after the hearing, the Grade Appeals Panel will decide
either to let the student’s original grade stand or to change the grade. The Grade Appeals
Panel chair will prepare a written report stating the panel’s decision along with the justification
for that decision. A copy of that report will be emailed to the student (using the student’s HCC
email account and/or the contact information the student indicated on the Grade Appeal Form),
the instructor, the instructional supervisor, and/or the dean/COE dean. If the Grade Appeals
Panel determines that the student’s grade is to be changed, then the instructor’s supervisor will
prepare and submit a Change of Grade Form. The decision of the Grade Appeals Panel is
final, except in cases of procedural error as specified below.
Level 4: Appealing the Panel’s Decision
A student grievant’s appeal of the Grade Appeal Panel’s final decision can only be based on
procedural errors that compromised the fundamental fairness of the process. If either the
student grievant or instructor who assigned the grade believes that the appeals process was
not properly followed, then he or she may file a written appeal to the Vice Chancellor for
Instructional Services/Chief Academic Officer (VCIS/CAO).
The VCIS/CAO will review the appeal and conduct whatever investigation is appropriate. If the
VCIS/CAO determines that the grade appeal process was not properly followed and that the
failure to follow proper procedures biased the result of the grade appeal, then s/he will vacate
the judgment of the grade appeal panel and direct that the process be repeated with a different
panel using the same deadline restrictions. If the VCIS/CAO rejects the appeal, the decision of
the Grade Appeal Panel is final.
HCC Instructional Leaders: For information regarding the required archiving of records related
to Course Grade Appeals, go to MyHCC > Instructional Services > Faculty Guidelines/Faculty
& Administrative Support > Course Grade

91
Appendix E
GRIEVANCE PROCEDURE

92
https://www.hccs.edu/departments/institutional-equity/
Equal Educational Opportunity Grievance
HCC is committed to providing an educational climate that is conducive to the personal and
professional development of everyone. Students should be aware that discrimination and/or other
harassment based on the race, sex, gender identity and gender expression, national origin,
religion, age, disability, sexual orientation, color, or veteran status is prohibited by HCC Policy
G.1 Discrimination and Harassment and D.1.1 Equal Educational Opportunities. HCC designates
the chancellor or designated representative to coordinate its Equal Employment
Opportunity/Affirmative Action efforts to comply with Title VI of the Civil Rights Act, Title IX of the
Education Amendments of 1972, as amended, and with the Americans with Disabilities Act
(ADA). Students who feel that they have been harassed or discriminated against or who feel that
the college district has not adequately fulfilled its obligations under the provisions above of the
should follow the Grievance Procedures stated below.
Sexual Harassment
HCC will provide an educational, employment and business environment free of sexual
harassment. Sexual harassment is a form of sex discrimination and is not tolerated by HCC. Any
student who feels that he or she is the victim of sexual harassment has the right to file a
grievance. Substantiated accusations may result in disciplinary action against the offender, up to
and including termination of the employee or suspension of the student. In addition, complainants
who make accusations of sexual harassment in bad faith may be subject to appropriate
disciplinary action.
Grievance Procedure
Any student who has a grievance concerning the interpretation, application or claimed violation of
his or her rights as an HCC student or feels he or she has been discriminated against or
harassed based on, race, sex, gender identity and gender expression, national origin, religion,
age, disability, sexual orientation, color, or veteran status including sexual harassment, can seek
resolution of such grievance. This may take place informally, through the mediation of designated
officers of the college, or formally, through an established grievance procedure.
Informal Resolution
A student who feels he or she is a victim of harassment or discrimination or that his or her rights
as a student have been violated may attempt to resolve the matter informally by bringing a
complaint to the college’s Dean of Student Services or to the college’s relevant Instructional Dean
(Academic or Career & Technology Education) for cases involving instructional matters. The
Dean, in coordination with the HCC Office of Institutional Equity, will attempt to resolve the
conflict informally by informing the individual alleged to have caused the grievance that the
complaint has been filed; seek to find out the facts; and, if both parties desire it, arrange a
meeting to try to resolve the differences. If an attempt at informal resolution of the problem is
unsuccessful, or if the complainant deems that informal resolution is undesirable, the college
officer will assist the complainant in filing of a formal complaint with the HCC Office of Institutional
Equity.
Formal Resolution
If a student wishes to initiate a formal complaint against another member of the college
community, the student must submit in writing a formal complaint to the HCC Office of Institutional
Equity, stating in detail, the nature of the complaint, any relevant dates, and the names of any
potential witnesses. An investigation will be initiated to determine whether there is a reasonable
basis for taking action. The Affirmative Action/Compliance Officer or designee must file a written
report with the college’s president. For more information
Report an Incident

93
\
APPENDIX F
EXCEEDING RADIATION DOSE

94
HOUSTON COMMUNITY COLLEGE SYSTEM
COLEMAN COLLEGE FOR HEALTH SCIENCES
RADIOGRAPHY PROGRAM
SUBJECT: Radiation Exposure Level Exceeded
Name:
We routinely investigate when radiation exposure levels are exceeded. The
Radiography Program sets a student threshold dose yearly to be 5 mSv or 500 mrem.
This dose limit is set based on 10% of the annual occupational dose limit.
Any exposure over 125 mrem in a quarter (HCCS uses quarterly dosimeters) would be
over the threshold dose. If a student exceeds the threshold dose in any quarter the
student is required to complete the applicable questions on this questionnaire. Please
reply as quickly as possible so that we can evaluate any factors affecting your
exposure.
1. Was the badge placed or stored near radiation?
2. Did you accidentally expose yourself to a beam of radiation?
3. Did you hold a patient during radiation exposure?
4. Did you work significantly more hours or procedures during this time?
5. Were you involved in procedures requiring unusually high exposure to radiation?
The RSO will discuss with the student about the importance of radiation safety if any of
the above questions were answered in the affirmative. The RSO will meet with the
student again after the next dose report to make sure the students’ dose is within
guidelines.
Please describe any unusual incident or provide any additional information that will help
explain your dose.
Discussion:
Printed name Signature Date
