
January 2022- F
New York Independent Assessor
Process Overview for Initial Assessments
Communication, Notices, Reports & UAS-NY Data
Exchange for the Local Department of Social
Services

2
Webinar Logistics
• All participants will remain muted throughout the presentation.
• Questions during the presentation should be submitted through the Q&A function.
• The presentation portion of the webinar is being recorded and will be posted along with
t
he slides on the Department of Health’s (Department) Independent Assessor (IA)
webpage.
• A question-and-ans
wer period will be held at the end of the presentation. Use the “raise
hand” function in WebEx if you would like to be unmuted to ask a question.
• Questions will be answered as time permits. All questions, including those we are
unab
le to answer during the webinar, will be included in FAQ documents.
• Answers provided to questions submitted during the webinar will be based on current
i
nformation, and thus may not constitute a complete or final answer. FAQ documents
will be posted on the Department’s IA webpage.
• Additional questions may be submitted after the presentation to
independent.assessor@health.ny.gov.
January 2022

3
Operational Series Training Topics
• Process Overview of Initial Assessments for Local Departments of Social
Services
• Process Overview for Initial Assessment Communication, Notices, Reports
(
includes UAS Data Exchange)
• NYIA IRP & Assessment Variance Process
• Fair Hearing Roles & Responsibility
• Process Overview of Reassessments for L
ocal Departments of Social Services
• Process Overview for Reassessment Communication, Notices, Reports (includes
UAS Data Exchange)
January 2022

4
Agenda
Introduction & Overview
Initial Assessment Outcome Notice
Reporting Process
Process Road Map – LDSS Completes POC
UAS-NY Reports
UAS-NY Data Exchange (optional)
Summary
Resources
January 2022

5
Introduction & Overview
January 2022

6
Introduction & Overview
• The New York Independent Assessor (NYIA) program was established for New
York State Medicaid recipients who want to receive personal care and/or Consumer
Directed Personal Assistance Services (CDPAS), and other community based long
term services and supports (CBLTSS).
• NYIA is responsible for sending outcome notices and generating reports for the local
D
epartment of Social Services (LDSS), the Mainstream/Health and Recovery Plan
(HARP)/ Special Needs Plans (SNP) and Managed Long Term Care (MLTC) Plans.
January 2022

7
Introduction & Overview (cont.)
• This presentation provides an overview of how Medicaid Fee for Service (FFS)
individuals, the local LDSS, and the New York Independent Assessor (NYIA) will
interact to communicate the results of the Initial Assessment.
• The communication, notification, and reporting process applies to all individuals who
ar
e scheduled to go through, or have completed, the Initial Assessment process with
NYIA and are not currently enrolled in an MMCO. This also applies to individuals who
are in the process of determining their Medicaid eligibility.
January 2022

8
Initial Assessment
Outcome Notice
January 2022

9
Initial Assessment Outcome Notice
January 2022

10
Initial Assessment Outcome Notices
January 2022
• NYIA is responsible for generating and mailing notices to
individuals informing them of the outcome of their Initial
Assessment.
• Once the Initial Assessment and Clinical Appointment are
finalized, NYIA will mail the Outcome Notice within 2-3 business
days to the individual’s address on file and to the Authorized
Representative’s address, if applicable
• It is very important to reinforce with the individual that the
LDSS has their most up to date address to receive timely
notifications.
• Outcome notices will be generated in English as the default
l
anguage.
• They will also be available in alternate languages
(
Spanish, Chinese, Russian, Haitian Creole, Bengali, or
Korean) based on an individual’s identified preference.
Outcome
Notice

11
The NYIA Initial Assessment Outcome
Notices include the following Sections:
• Introduction
• Your Assessment Showed
• What Happens Next
• Questions? Call Us
• Independent Consumer Advocacy
Network (ICAN)
• All notices that deny either service or MLTC
Plan eligibility will include language about
Conference and Fair Hearing rights.
January 2022
Initial Assessment Outcome Notice

12
Dear <Member Name>
We are writing about your assessment and clinical
exam with the New York Independent Assessor.
Your assessment result was completed on
<Response Date>.
The assessment helps us find out which Medicaid
community based long term services and
supports (CBLTSS) you may need. These
services include personal care or Consumer
Directed Personal Assistant Services (CDPAS).
You must be eligible for Medicaid health benefits
and have certain care needs to get these
services.
The Introduction section informs the
individual the reason for the notice
and the following information:
• The date that their assessment
r
esult was completed. This is the
date that the CHA and CA are
finalized.
• A brief explanation of the reasons
for the assessment.
• A statement on Medicaid eligibility
to be able to receive State
benefits.
January 2022
Initial Assessment – Introduction
13
Initial Assessment – Your Assessment Showed
• The language in the Your assessment showed section varies depending on
the population and the outcome of the initial assessment:
• Personal care, CDPAS and other CBLTSS eligibility
• MLTC Plan Enrollment eligibility, if applicable
• Dual
• Non-dual
• Clinical Assessment Outcome, if appropriate
• Populations included in the Initial assessment process include:
• FFS (Dual and Non-dual) seeking personal care and/or CDPAS and/or enrollment into
a MLTC Plan
• Mainstream/HARP/SNP individuals seeking personal care and/or CDPAS services
only
January 2022

14
Your assessment showed:
You are eligible for Medicaid community based
long term services and supports (CBLTSS),
including personal care and/or CDPAS.
OR
Your assessment showed:
You may be eligible for Medicaid community
based long term services and supports (CBLTSS).
• In the Your assessment
s
howed section, an
individual will be informed if
they are eligible for
CBLTSS, including personal
care and CDPAS.
• This language will be
included, if it is determined
that service cannot be
rendered safely in the
community.
January 2022
Initial Assessment – Your Assessment
Showed - CBLTSS Eligibility

15
Your assessment showed:
You may qualify to receive long term
services and supports through a
Managed Long Term Care (MLTC) Plan.
The MLTC Plan you choose will discuss
your plan of care with you. We can help
you choose a Plan or connect you with
your LDSS if you choose not to join a
Plan at this time.
This language is included when the FFS
individual meets the MLTC Plan enrollment
criteria listed below. MLTC Plans are still
required to determine that the individual
meets other Plan enrollment criteria.
• Dual eligible, age 18 through 20, in need of
community-based long-term care services for
over 120 days and assessed as nursing home
eligible.
• Non-dual eligible age 18 and older assessed
as nursing home eligible and in need of
community-based long-term care services for
over 120 days.
January 2022
Initial Assessment – Your Assessment
Showed – MLTC Plan Enrollment Eligibility

16
Your Assessment Showed:
You may be eligible for Medicaid community based long term services and supports (CBLTSS),
including personal care and/or CDPAS. However, you do not qualify to enroll in a Managed Long
Term Care (MLTC) Plan at this time.
You do not need any of the services listed below for more than 120 days. To get long term services
and supports in an MLTC Plan, you must require one of these services for more than 120 days:
• Nursing services in the home
• Home health aide services
• Private duty nursing
• Personal care services in the home
• Adult day health care
• Consumer Directed Personal Assistance Services (CDPAS)
• Therapies in the home (physical, occupational, respiratory and speech pathology)
• This language is
included when a FFS
individual does not
meet the 120 days
requirement to receive
CBLTSS through a
MLTC Plan.
• However, this does
NOT mean that they
are ineligible for
personal care and/or
CDPAS or other
CBLTSS.
January 2022
Initial Assessment – Your Assessment
Showed – MLTC Plan Enrollment Eligibility

17
Your Assessment Showed:
You have regular Medicaid and you do not need the level of care required
for people with your health coverage to get these services in an MLTC
Plan. To get long term services and supports in an MLTC Plan, you must
require both nursing home level of care and one or more of the services
below for more than 120 days:
• Nursing services in the home
• Home health aide
• Private duty nursing
• Personal care services in the home
• Adult day health care
• Consumer Directed Personal Assistance Services (CDPAS)
• Therapies in the home (physical, occupational, respiratory or speech
pathology)
• This language is included
when a FFS individual
does not meet the MLTC
Plan eligibility
requirement.
• However, this does NOT
mean that they are
ineligible for CBLTSS.
January 2022
Initial Assessment – Your Assessment
Showed – MLTC Plan Enrollment Eligibility

18
Your assessment showed:
Your clinical exam showed your health
condition is not stable enough to get
personal care and/or CDPAS at home.
• This language is only included if the
individual's clinical exam found, and
Practitioner's Order identified, that
their health condition is NOT stable to
receive personal care and/or CDPAS
at home.
January 2022
Initial Assessment – Your Assessment Showed
- Clinical Assessment Outcome

19
Your assessment showed:
You are eligible for Medicaid community based long term
services and supports (CBLTSS).
However, your clinical exam showed your health condition is
not stable enough to get personal care and/or CDPAS at
home.
You may qualify to receive long term services and supports
through a Managed Long Term Care (MLTC) Plan. The MLTC
Plan you choose will discuss your plan of care with you. We
can help you choose a Plan or connect you with your LDSS if
you choose not to join a Plan at this time.
• The notice informs the
individual that they are
eligible for CBLTSS
• This language is added to
the notice ONLY if the
results of the clinical
appointment determine that
the individual
is not stable to receive
services in their home.
• The MLTC language is
included for this population.
January 2022
Example: Your Assessment Showed – FFS

20
• This language informs them of their
eligibility for CBLTSS.
• This language is added to the notice
O
NLY if the results of the clinical
appointment determine that the
individual is not stable to receive
services in their home.
January 2022
Example: Your Assessment Showed –
Mainstream/HARP/SNP
Your assessment showed:
You are eligible for Medicaid community based
long term services and supports (CBLTSS).
However, your clinical exam showed your
health condition is not stable enough to get
personal care and/or CDPAS at home.

21
Your assessment showed:
You may be eligible for Medicaid community based long term services and supports
(CBLTSS). However, you do not qualify to enroll in a Managed Long Term Care (MLTC)
Plan at this time.
You do not need any of the services listed below for more than 120 days. To get long
term services and supports in an MLTC Plan, you must require one of these services
for more than 120 days:
• Nursing services in the home
• Home health aide services
• Private duty nursing
• Personal care services in the home
• Adult day health care
• Consumer Directed Personal Assistance Services (CDPAS)
• Therapies in the home (physical, occupational, respiratory and speech pathology)
• This language is
included when a FFS
individual does not
meet the MLTC Plan
eligibility requirement of
“in need of community-
based long-term care
services for over 120
days”
• However, this does
NOT mean that they are
ineligible for CBLTSS.
January 2022
Initial Assessment – FFS

22
FFS
What happens next:
Call us to learn about the long term
services and supports options that are
available to you. You can call us at 1-
855-222-8350.
Mainstream/HARP/SNP
What happens next:
You can call your Plan to discuss next
steps. Your Plan will review your
assessment results. They will work with
you to evaluate your needs and develop
your plan of care.
One of our counselors can provide you
with your Plan’s phone number.
January 2022
Initial Assessment – What Happens Next
23
Questions? Call Us.
If you have any questions about this letter,
please call us. You can call us at 1-855-222-
8350 (TTY: 1888-329-1541). We can help
you in any language.
Thank you,
New York Independent Assessor
All NYIA Initial Assessment notices
include the "Questions? Call Us."
language.
• NYIA is responsible for answering any
que
stions regarding the outcome
notices and providing the referrals to
the correct entity, including MLTC Plan
options.
January 2022
Initial Assessment – Questions?

24
Information about The Independent
Consumer Advocacy Network
The Independent Consumer Advocacy Network
(ICAN) is the ombudsman program for health plan
members. ICAN can answer your questions and
give you free, independent advice about your
coverage, complaint, and appeal options. To learn
more about ICAN, go to
www.icannys.org, or call
1-844-614-8800. TTY: 711. All services are free.
• Information about The
I
ndependent Consumer
Advocacy Network will be
included in all NYIA Initial
Assessment Outcome
Notices.
January 2022
Initial Assessment – ICAN

25
Dolly is a Dual FFS Medicaid individual and has
requested to be enrolled in an MLTC Plan. NYIA
schedules both of their CHA and Clinical
assessment via in person.
• The outcome of Dolly’s Initial Assessment (CHA
an
d CA) determined that they are:
• Eligible for CBLTSS
• PO Indicates health condition is stable to receive
p
ersonal care and/or CDPAS at home
• Meets the MLTC Plan enrollment criteria
• Upon finalization of the Initial Assessment (CHA
and CA), NYIA will issue an Initial Assessment
Outcome Notice to Dolly within 2-3 business
days.
January 2022
Initial Assessment - Scenario
Outcome
Notice

26
Dear Dolly,
We are writing about your assessment and clinical
exam with the New York Independent Assessor.
Your assessment result was completed on May 15,
2022.
The assessment helps us find out which Medicaid
community based long term services and supports
(CBLTSS) you may need. These services include
personal care or Consumer Directed Personal
Assistant Services (CDPAS). You must be eligible
for Medicaid health benefits and have certain care
needs to get these services.
January 2022
Scenario - Introduction
• Dolly receives an Initial
Assessment Outcome notice.
Outcome
Notice

27
• The outcome of Dolly’s Initial
Assessment (CHA and CA)
determined that Dolly is:
• Eligible for CBLTSS
• PO Indicates health condition is stable
to receive personal care and/or
CDPAS at home
• Meets the MLTC Plan enrollment
criteria
Your assessment showed:
You are eligible for Medicaid community
based long term services and supports
(CBLTSS), including personal care and/or
CDPAS.
You may qualify to receive long term
services and supports through a Managed
Long Term Care (MLTC) Plan. The MLTC
Plan you choose will discuss your plan of
care with you. We can help you choose a
Plan or connect you with your LDSS if you
choose not to join a Plan at this time.
.
January 2022
Scenario – Your Assessment Showed
Outcome
Notice

28
• Dolly is referred to call NYIA in the
What happens next section. This is
based on determination that Dolly met
the MLTC Plan enrollment criteria.
• NYIA is responsible for providing
pr
ogram education, including the
MLTC Plans available in Dolly’s
service area.
What happens next:
Call us to learn about the long term
services and supports options that are
available to you. You can call us at 1-
855-222-8350.
January 2022
Scenario – What Happens Next
Program
Education
Outcome
Notice

29
• All Initial Assessment
Outcome Notices
include the Questions?
Call Us & ICAN
sections. This provides
Dolly reference
numbers, if needed.
Questions? Call Us.
If you have any questions about this letter, please call us. You can
call us at 1-855-222-8350 (TTY: 1888-329-1541). We can help you in
any language.
Thank you,
New York Independent Assessor
Information about The Independent Consumer Advocacy
Network
The Independent Consumer Advocacy Network (ICAN) is the
ombudsman program for health plan members. ICAN can answer
your questions and give you free, independent advice about your
coverage, complaint, and appeal
January 2022
Scenario – Questions? & ICAN
Outcome
Notice

30
• Dolly contacts the NYIA for Plan enrollment
options and decides that they do not want to enroll
into a MLTC Plan at this time.
• Dolly will be referred back to the LDSS for
C
BLTSS.
• LDSS will follow their current process to develop
t
he plan of care.
• Note: There is no impact on current auto
as
signment process from FFS to MLTC Medicaid
Plan, also known as Partial Capitation.
January 2022
Scenario – Plan of Care
Program
Education
LDSS
Completes
POC

31
Reporting Process
January 2022

32
Reports
NYIA has developed 4 new reports for the LDSS regarding initial assessments.
They are:
1. Appointment booking for initial assessments in the next 30 calendar days
2. CHA outcome
3. PO outcome
4. Variance report
T
hese reports will be stored in new folders in your existing folders on MOVEit
January 2022

33
Scheduled Initial Assessment Report
• Name of Report: Consumers Scheduled for Initial Assessments within the next
30 Days
• Frequency report generated: Weekly
• Summary of report: T
he report will provide each LDSS with a list of FFS
individuals who have an initial assessment (including CHA and CA appointments)
scheduled within the next 30 calendar days
• What will LDSS use report for: The report will provide each LDSS with a list of
F
FS individuals in their county who may be contacting them to develop their POC
as the individual has completed the CHA and CA appointments
January 2022

34
Contents of Scheduled Initial Assessment Report
The Initial Assessment Report will contain the following fields:
• CIN (if available)
• Name
• Social Security Number (if available)
• County
• Appointment ID
• Appointment Type
• Appointment Reason
• Appointment Scheduled date
January 2022

35
Sample of Scheduled Initial Assessment Report
January 2022

36
Initial CHA Appointment Outcome Report
• Name of Report: Initial CHA Appointment Outcomes Report
• Frequency report generated: Daily
• Summary of report: T
he report will provide each LDSS a list of FFS individuals
who NYIA completed an Initial Community Health Assessment (CHA)
Appointment.
• What will LDSS use report for: L
DSS will be able to review UAS-NY for the
CHA results and begin to develop their Plan of Care with the Individual
January 2022

37
Contents of Initial CHA Appointment Outcome Report
The CHA Appointment Outcomes Report will contain the following fields:
• CIN (if available)
• Name
• Social Security Number (if available)
• County
• Appointment ID
• Appointment Type
• Appointment Reason
• Appointment Scheduled date
• Assessment Status
• Reason Description
January 2022

38
Sample of Initial CHA Appointment Outcome Report
January 2022

39
Initial PO Outcomes Report
• Name of Report: Initial PO Outcomes Report
• Frequency report generated: Daily
• Summary of report: T
he report will provide each LDSS with a list of FFS
individuals on who NYIA completed the Clinical Appointment and issued a
Practitioner’s Order
• What will LDSS use report for: T
he report will provide each LDSS with a list of
FFS individuals in their county who may be contacting them to develop their POC
as the individual has completed the CHA and CA appointments
January 2022

40
Contents of Initial PO Outcomes Report
The PO Outcomes Report will contain the following fields:
• CIN (if available)
• Name
• Social Security Number (if available)
• County
• Appointment ID
• Appointment Type
• Appointment Reason
• Appointment Scheduled date
• Assessment Outcome
January 2022

41
Sample of Initial PO Outcomes Report
January 2022

42
Variance Report (on completed Initial Assessments)
• Name of Report: Variance Report on completed Initial Assessments
• Frequency report generated: Weekly
• Summary of Report: T
he report provides each LDSS a list of FFS individuals
who the LDSS has requested a variance review on initial assessments and the
status update on those reviews.
• What will LDSS use report for:
• track that NYIA received the variance review request submitted to NYIA and
t
he outcome of the variance review.
• reconcile their internal variance request report and,
• as applicable, initiate modifications to the POC.
N
ote: Additional information on the Variance Review process will be covered in
future training.
January 2022

43
Contents of Variance Report (on completed Initial
Assessments)
The Weekly Variance Report will contain the following fields:
• Creation Date
• CIN (if available)
• Name
• County
• Tracking Number
• Variance Reason
• Status
• Status Date
• New Assessment Date (if applicable)
January 2022

44
Sample of Variance Report (on completed Initial
Assessments)
January 2022

45
Reports
January 2022
• NYIA posts reports to designated folders for each LDSS on its Secure File Transfer
Portal (SFTP) server, also known as
MOVEit.
• NYIA will continue to generate existing reports for FFS individuals to provide to the
LDSS.
• Each LDSS has access to only their location’s folders, files, and reports.
• After the reports have been uploaded to the SFTP, the LDSS contact(s) for that office
w
ill receive an electronic notification that reports are available for them to access.

46
Accessing Reports
January 2022
• The LDSS will log into MOVEit (
https://edi.maximus.com/) to access their reports.
• Each LDSS determines who from their agency will have access to their reports and submits a request
f
or access to NYIA .
• Once NYIA has granted the LDSS user access, they will be provided with written instructions on how to
l
og in and access their reports.
• If the LDSS needs to request access to MOVEit, they will continue to follow existing process and send
an
email to NYDM@Maximus.com to request access. In the email, they will need to include the
following:
• Name
• County
• Program they are requesting access for (i.e., IA, IPP)
• NYIA will notify the LDSS once the new account has been created with instructions on how to create a
pa
ssword.
Note: The account will become inactive if the user fails to log on to MOVEit after 30 days. A new request
will need to be submitted to reactivate the account.

47
New Initial Assessment Report Location on MOVEit
• Click on the file hyperlink to see the
information in the reports
January 2022

48
Process Road Map –
LDSS Completes POC
January 2022

49
LDSS Roles and Responsibilities
Once an individual has received their NYIA Initial Assessment Notice and NYIA
provided program education, NYIA will refer the individual to their LDSS or their
Plan of choice. The LDSS and MMCO Plans are responsible for the following:
• Adding individuals to the UAS-N
Y Organizational Case List
• Developing the Plan of Care
• Adding UAS-N
Y Enrollment records
Notes:
• MLTC Plans are still responsible for submitting the enrollment to NY Medicaid
C
hoice if the individual requests to enroll. (NYIA has no impact on the current
MLTC enrollment process.)
• Plan of Care development m
ay include additional outreach to the individual such
as conducting an in-home visit with the individual to evaluate their home
environment or a review of their informal supports.
January 2022

50
Search for an Individual Record in the UAS-NY
January 2022

51
Consent Prompts
January 2022

52
To review the NYIA
completed CHA and PO, the
LDSS must attest to the
legitimate business need to
access the individual’s UAS-
NY case file.
January 2022
Attestation to Access Case File

53
Develop Plan of Care
• LDSS must utilize the NYIA
Community Health Assessment
(CHA) and Practitioner’s Order (PO)
to develop Plan of Care as
appropriate
• LDSS must follow the current
process to develop the Plan of Care
and offer to the individual
• Note: If POC requires 12+ hours of
c
are, LDSS must follow the
Independent Review Panel process
January 2022

54
Remove Individual from UAS-NY Case List
January 2022
If the individual does not accept the Plan of Care, the
LDSS must remove the individual from their UAS-NY
Organization Case List.

55
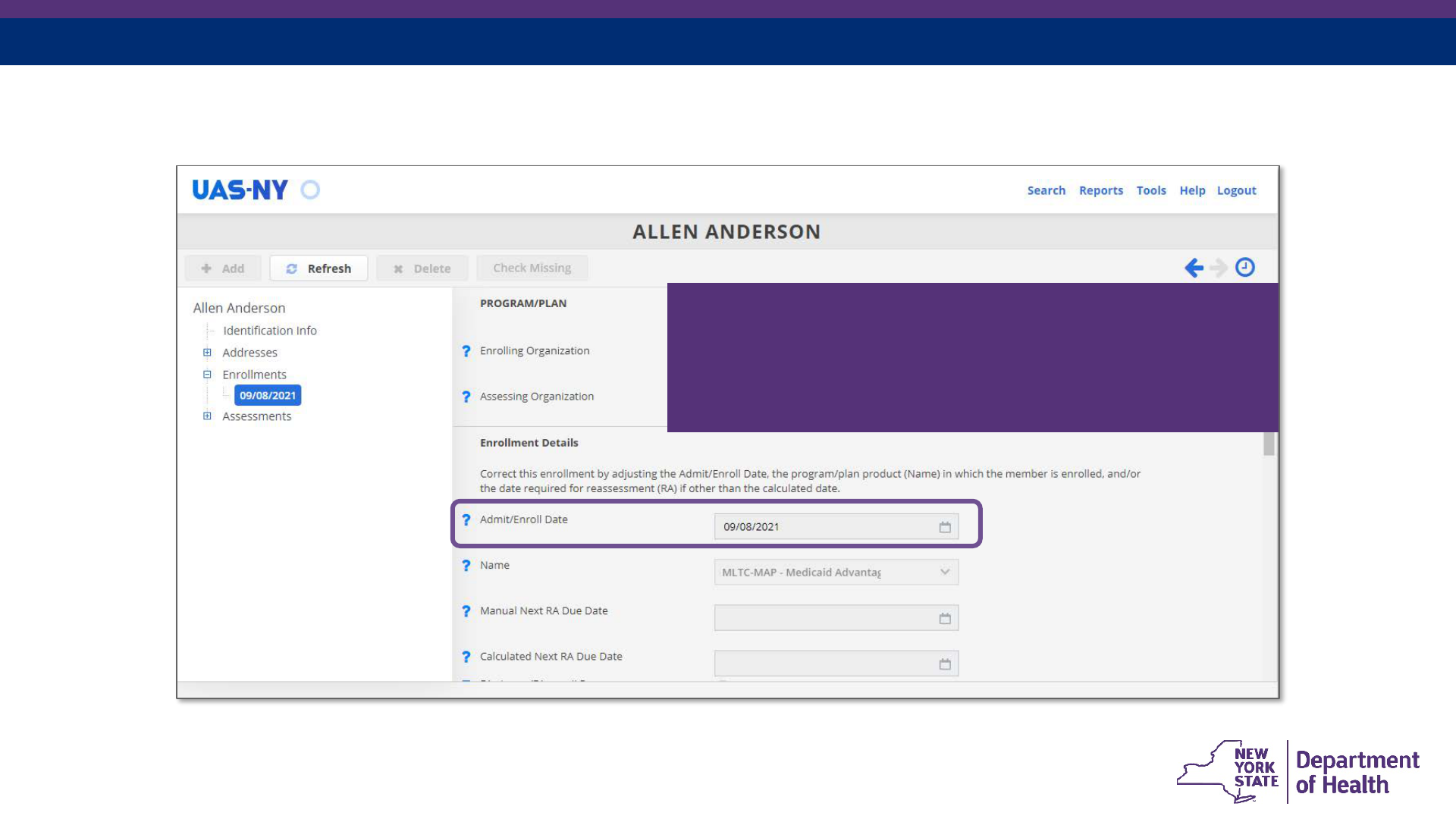
The LDSS must enter an
Enrollment into the
individual’s case file in the
UAS-NY if the individual
accepts the Plan of Care.
Note: The NYIA
reassessment process
depends on accurate
enrollment information in the
UAS-NY.
January 2022
Add UAS Enrollment Record

56
Disenrollment and Removal from Case List
January 2022
A disenrollment in the UAS-
NY should be entered when:
• No longer receiving
services with the LDSS
The Disenrollment
functionality also removes
the individual from the
Organizational Case List.

57
Importance of Enrollments and
the Organization Case List
• NYIA will rely on the enrollment record as it appears in the UAS-NY to determine
who needs to be scheduled for reassessment.
• If an LDSS does not add the enrollment:
• the LDSS will not receive the NYIA assessment in their Data Exchange (initial
or
reassessment), and
• the individual will not be reassessed.
• Maintaining the Organization Case List is both mandatory by policy and critical for
s
mooth operations between the NYIA and the LDSS.
• UAS-N
Y.19.2Organization Case List Management Policy for the UAS-NY
January 2022

58
UAS-NY Reports
January 2022

59
UAS-NY Reports
Reports accessible within the UAS-NY will continue be
available to assist you with:
• Plan of Care development
• UAS-NY Enrollment Management
• Organizational Case List Management
January 2022

60
UAS-NY Comprehensive Assessment Report
January 2022
Full Community
Health Assessment
in PDF format

61
UAS-NY Enrollment Report
January 2022
Shows all case files
with an attestation
and an active
enrollment in the
UAS-NY for your
organization.

62
UAS-NY Missing Dis-Enrollments Report
January 2022
Displays all case
files where your
organization has
enrolled an
individual in the
same
program/product as
another enrolling
organization.

63
UAS-NY Missing Enrollments Report
January 2022
Displays all case
files for which your
organization has
attested a business
need to
access, but for
which you have
not added
an enrollment.

64
UAS-NY Data Exchange
(optional)
January 2022

65
UAS-NY/UPHN Lite Data Exchange
• Definition: The UAS-NY/UPHN Lite Data Exchange is a service designed for the
secure exchange of protected health information with organizations that have
been authorized and approved for such exchanges.
• The UAS-N
Y Data Exchange is a data feed that sends assessment data nightly
to a participating organization.
• Any organization currently pa
rticipating in the Data Exchange will continue to
receive assessment data in the same manner through their current Data
Exchange.
• The rules for the Data Exchange have been updated so organizations can
r
eceive data for NYIA conducted assessments
January 2022

66
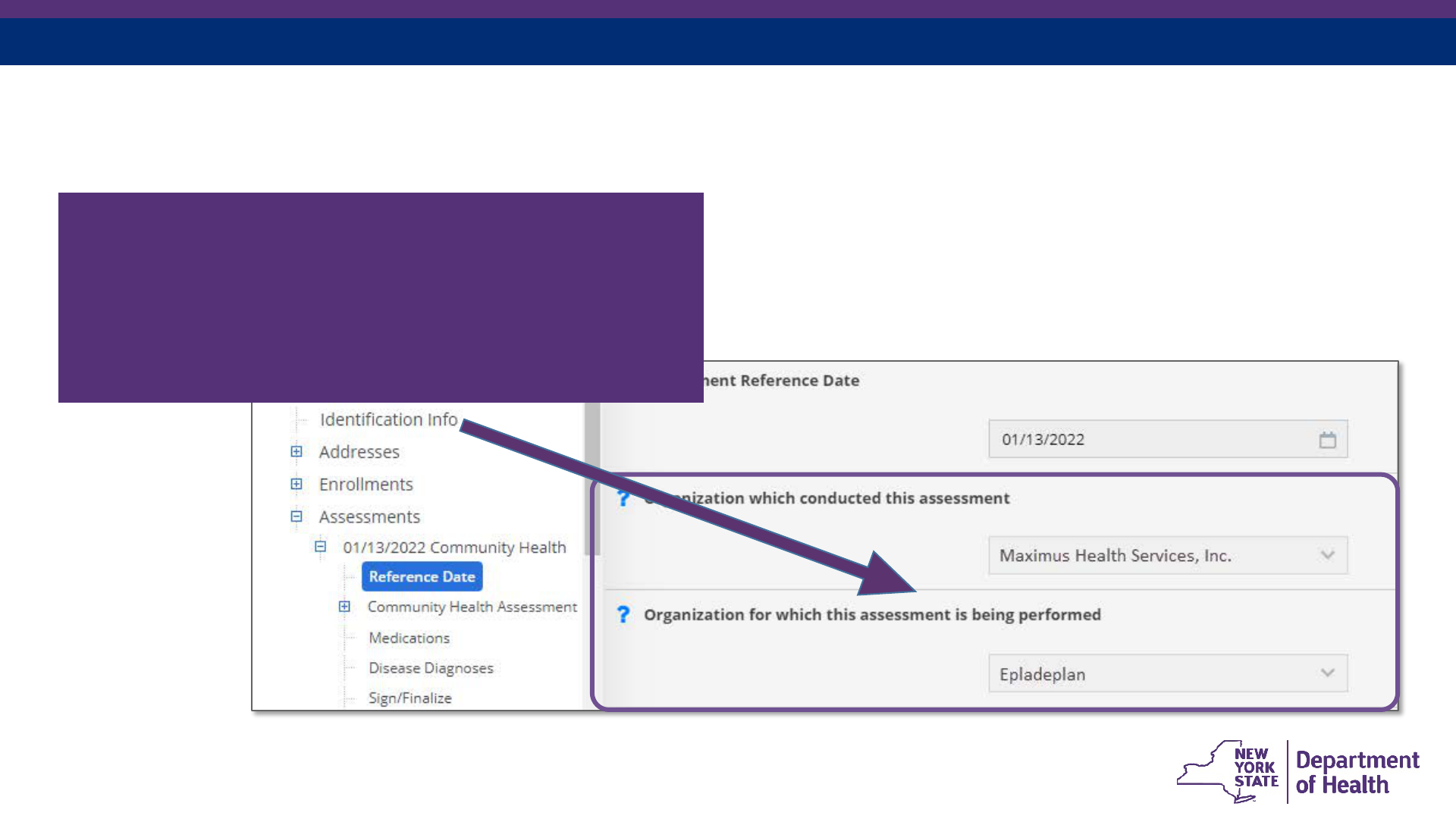
Existing Data Exchange Rules:
• The following conditions must be met. The organization must have:
• Consent from the individual to access the individual’s case file
• Active attestation for the individual
• A current enrollment record in the UAS-
NY
• The signed/finalized assessment must name the enrolling
o
rganization as the “Organization for which this assessment is
being performed”.
January 2022

67
New Data Exchange Rules
(coding already implemented)
• The following conditions must be met. The organization must have:
• Consent from the individual to access the individual’s case file;
• Active attestation for the individual;
• A current enrollment entry in the UAS-
NY;
• The “Organization which conducted this assessment” must be
t
he NYIA;
• The “Organization for which this assessment is being
p
erformed” must be the NYIA; and
• The organization’s enrollment must be for one of the product
t
ypes handled by the NYIA:
• MLTC-
PCP, MLTC-MAP, MMC, HARP, SNP, Personal Care,
CDPAP
January 2022

68
Condition 1 - Consent
January 2022
Organization must
have consent from the
individual to access
the individual’s case
file.

69
Condition 2 – Active Attestation
January 2022
Organization must have an active
attestation for the consumer.
70
Condition 3 – Enrollment Recorded in the UAS-NY
January 2022
Organization must have an enrollment entry
in the UAS-NY that is active the day of
transmission.
71
Condition 4a – Assessment Conducted By/For
(no change)
January 2022
The enrolling organization must be selected
as the “Organization for which this
assessment is being performed”. (current rule)

72
Condition 4b – Assessment Conducted By/For (new)
January 2022
• “Organization which conducted this assessment” must be NYIA,
• “Organization for which this assessment is being performed” must be the
NYIA, and
• Organization’s enrollment must be for one of the product types handled by the
NYIA (MLTC-PCP, MLTC-MAP, MMC, HARP, SNP, Personal Care, CDPAP).
73
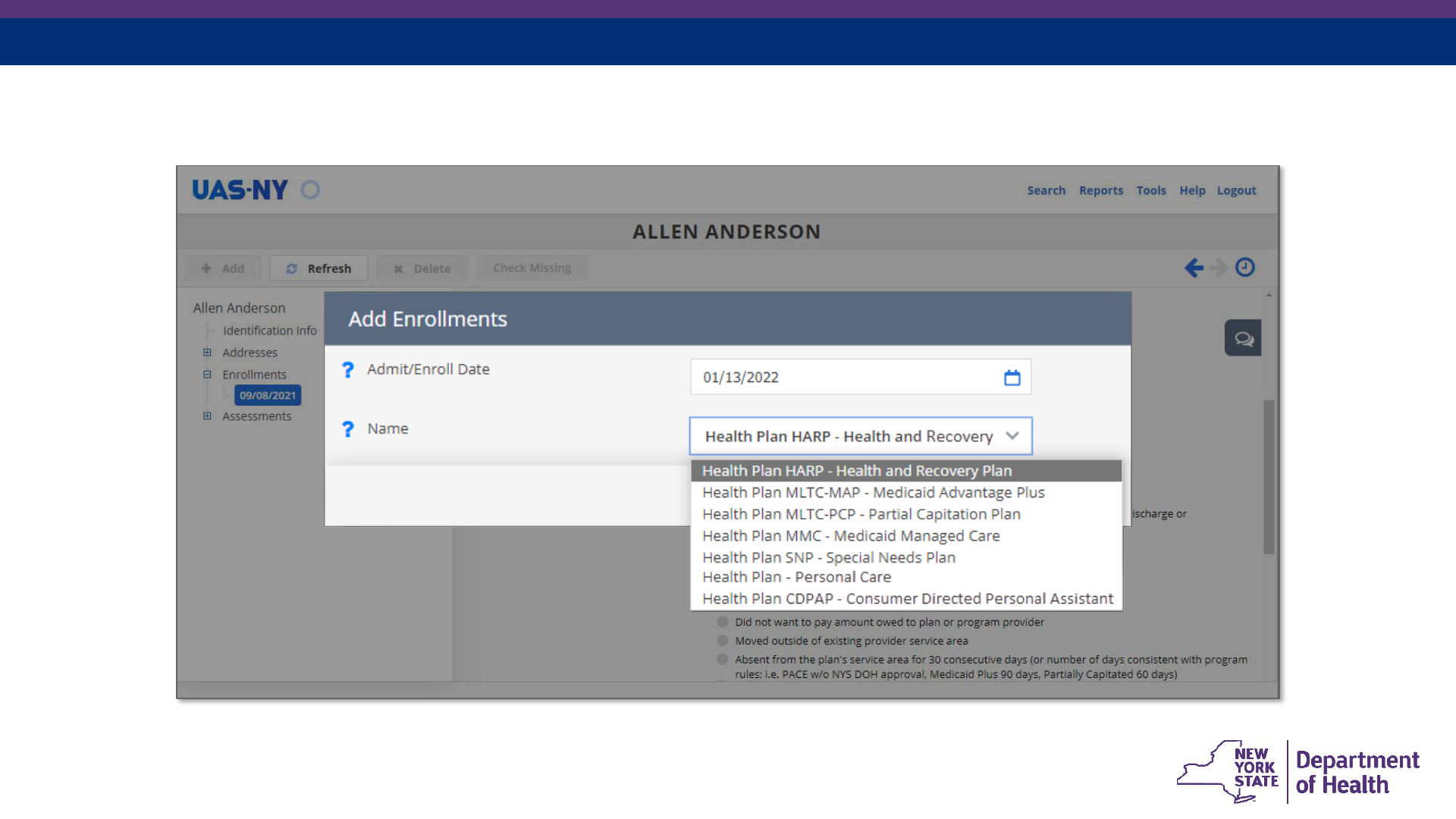
Product types handled by NYIA
January 2022

74
Condition 5 – Sign/Finalize the Assessment
January 2022
Assessment must be
signed/finalized.

75
How to sign up for the Data Exchange
• Contact UAS-NY Support Desk: uasny@health.ny.gov
• Note: The set-up process to begin utilizing the Data Exchange takes a significant
amount of time (usually several weeks).
• Your Organization Case List will need to be accurate prior to initiating the Data
Exchange to ensure accurate data is transmitted.
• Your organization will need to appoint an Organization Security Coordinator (OSC),
who will be responsible for the Data Exchange. This process requires notarized forms
to be mailed to the Health Commerce System (HCS).
• Your organization will need to download the UPHN Lite Client to an appropriately
secure location.
The UAS-NY Support Desk and UPHN Lite teams will be happy to assist your
organization through this process.
January 2022

76
Summary
January 2022

77
Summary
• An outcome notice will be issued to the individual upon the completion of an Initial
Assessment and a Clinical Appointment. The outcome notice informs the
individual:
• If they are eligible for CBLTSS, including personal care and/or CDPAS
• If services cannot be rendered safely in the community
• Their Plan options (if applicable)
• Fair Hearing rights (if applicable)
• Results of the Initial Assessment and Clinical Appointment are available in the
U
AS-NY application.
January 2022

78
Resources
January 2022

79
• Final Regulations can be found at:
• Personal Care Services 505.14
• Consumer Directed Personal Assistance Services 505.28
• DOH/NYIA will be scheduling additional webinars and trainings with LDSS front-line
staff in January 2022. Information on trainings will be posted on the DOH’s website at:
https://www.health.ny.gov/health_care/medicaid/redesign/independent_assessor.htm
• Questions can be sent to independent.assessor@health.ny.gov
January 2022
Resources

80
Questions and Answers
Process Overview for Initial
Assessments: Communication,
Notices, Reports, UAS-Reports &
UAS-NY Data Exchange for the
Local Department of Social
Services
January 2022
