
Evaluation of Worker
Exposures to Peracetic
Acid-Based Sterilant
during Endoscope
Reprocessing
David Sylvain, MS, CIH
John Gibbins, DVM, MPH
Health Hazard Evaluation Report
HETA 2006-0298-3090
Kaleida Health–Buffalo General Hospital
Buffalo, New York
August 2009
DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
Workplace
Safety and Health
National Institute for Occupational
Safety and Health
This Health Hazard Evaluation (HHE) report and any recommendations made herein are for the specific
facility evaluated and may not be universally applicable. Any recommendations made are not to be
considered as final statements of NIOSH policy or of any agency or individual involved. Additional HHE
reports are available at http://www.cdc.gov/niosh/hhe/

The employer shall post a copy of this report
for a period of 30 calendar days at or near
the workplace(s) of affected employees. The
employer shall take steps to insure that the
posted determinations are not altered, defaced,
or covered by other material during such
period. [37 FR 23640, November 7, 1972, as
amended at 45 FR 2653, January 14, 1980].

Page i
Health Hazard Evaluation Report 2006-0298-3090
Re p o R t
Abbreviations .......................................................................ii
Highlights of the NIOSH Health Hazard Evaluation ............ iii
Summary .............................................................................v
Introduction ..........................................................................1
Assessment .........................................................................4
Results .................................................................................5
Discussion ...........................................................................7
Conclusions .........................................................................9
Recommendations .............................................................10
References ........................................................................12
Co n t e n t s
Acknowledgments and Availability of Report .....................15
AC k n o w l e d g m e n t s

Page ii
Health Hazard Evaluation Report 2006-0298-3090
ACGIH® American Conference of Governmental Industrial Hygienists
BGH Buffalo General Hospital
CDRH Center for Devices and Radiological Health
CFR Code of Federal Regulations
FDA United States Food and Drug Administration
HVAC Heating, ventilating, and air-conditioning
HHE Health hazard evaluation
LOD Limit of detection
mL/min milliliters per minute
NAICS North American Industry Classification System
NIOSH National Institute for Occupational Safety and Health
OEL Occupational exposure limit
OPA ortho-Phthalaldehyde
OSHA Occupational Safety and Health Administration
PAA Peracetic acid
PBZ Personal breathing zone
PPE Personal protective equipment
ppm Parts per million
REL Recommended exposure limit
RH Relative humidity
SS1 Steris SYSTEM 1® Processing System
TWA Time-weighted average
Ab b R e v i A t i o n s

Page iii
Health Hazard Evaluation Report 2006-0298-3090
What NIOSH Did
We met with management, employees, and a union ●
representative to discuss employee concerns.
We toured the A2 GI Lab Steris Room and observed staff at ●
work.
We collected area and personal air samples for acetic and ●
peracetic acids.
We measured temperature and relative humidity. ●
We used smoke tubes to observe airflow patterns in the A2 ●
GI Lab Steris Room.
We spoke with employees confidentially about possible work- ●
related symptoms, safety and health training, use of personal
protective equipment (PPE), chemical exposure incidents,
and indoor environmental quality.
We looked at Food and Drug Administration reports ●
of sterilant spills, worker exposures, and injuries during
endoscope reprocessing at other hospitals to identify possible
causes of problems reported at this facility.
What NIOSH Found
Concentrations of peracetic acid are thought to be low, ●
although we could not measure current levels.
Latex gloves worn while handling peracetic acid sterilant ●
containers do not provide adequate protection.
Some workers reported not using all available PPE (aprons ●
and sleeve protectors) due to high temperatures in the A2 GI
Lab Steris Room.
Two workers reported prior chemical burns from contact ●
with Steris 20 Sterilant Concentrate.
Employees did not receive adequate training in chemical ●
hazard communication and in standard operating procedures
for chemical spills, leaks, and processor malfunctions.
Ventilation in the A2 GI Lab Steris Room was inadequate. ●
Exposure to peracetic acid sterilant is unlikely when Steris ●
processors are maintained and operated properly and when
technicians follow the manufacturer’s operating procedures.
In July 2006, the National
Institute for Occupational
Safety and Health (NIOSH)
received a confidential
health hazard evaluation
(HHE) request from
employees at Kaleida
Health-Buffalo General
Hospital in Buffalo, New
York. The HHE request
stated that inadequate
ventilation was provided
in the A2 GI Lab Steris
Room where five
employees clean and
sterilize endoscopes
using Klenzyme®
Enzymatic Cleaner and
Steris® 20 Sterilant
Concentrate. Health
problems identified in the
request were headache,
shortness of breath, eye
irritation, and diminished
sense of smell. We
conducted a site visit on
December 18–19, 2006.
Hi g H l i g H t s o f t H e
niosH He A l t H
HA z A R d ev A l u A t i o n

Page iv
Health Hazard Evaluation Report 2006-0298-3090
Hi g H l i g H t s o f t H e
niosH He A l t H
HA z A R d ev A l u A t i o n
(C o n t i n u e d )
What Hospital Managers Can Do
Require use of appropriate PPE to prevent eye, face, hand, ●
arm, and body contact with concentrated peracetic acid
as well as other cleaning chemicals and contaminated
equipment.
Provide hazard communication training for A2 GI Lab Steris ●
Room employees.
Train employees in standard operating procedures for spills, ●
leaks, and processor malfunctions.
Ask Steris Corporation to provide new employee and annual ●
refresher inservice training.
Make sure that processors are inspected periodically for worn ●
parts that can cause leaks.
Notify Steris Corporation of leaks and equipment problems. ●
Increase ventilation in the A2 GI Lab Steris Room for odor ●
control and the comfort of the workers.
What Steris Room Employees Can Do
Wear tight-fitting splash-resistant goggles and acid-resistant ●
gloves, sleeves, and apron when handling sealed Steris cups
during normal operations.
Wear a face shield over eye protection along with routine ●
PPE when handling or disposing of a cup that is not
completely empty.
Follow the manufacturer’s instructions for handling Steris ●
cups and operating processors.
Tell management about problems with processors or Steris ●
cups, or if you notice worn processor seals or other parts.
Follow standard operating procedures for processor ●
problems, leaks, and sterilant spills.
Participate in training when provided. ●

Page v
Health Hazard Evaluation Report 2006-0298-3090
In July 2006, NIOSH received a confidential HHE request from
employees at Kaleida Health-Buffalo General Hospital in Buffalo,
New York. The HHE request stated that inadequate ventilation was
provided in the A2 GI Lab Steris Room where five employees clean
and sterilize endoscopes with Klenzyme® Enzymatic Cleaner and
Steris® 20 Sterilant Concentrate. Health problems identified in
the request were headache, shortness of breath, eye irritation, and
diminished sense of smell.
On December 18–19, 2006, we conducted a site visit that included
an opening conference, a walk-through of the A2 GI Lab Steris
Room, air sampling for peracetic and acetic acids, measurements
of temperature and RH, smoke tube visualization of airflow, and
confidential informal interviews with several employees.
Air samples did not contain detectable concentrations of acetic
acid. Sampling results and our onsite observations indicate very
little, if any, airborne exposure to peracetic acid sterilant on the
sampling date. The temperature was 74ºF to 76ºF, and the RH was
17% to 20%. Smoke tube visualization of airflow at the ceiling-
mounted ventilation supply diffusers and return grilles in the
Steris room indicated that the HVAC system provided insufficient
airflow. Ventilation in the Steris room appeared to be inadequate
for providing reliable odor control and maintaining the work
environment within an acceptable range of temperature and RH.
Employees reported periodic headaches and burning eyes that
were more noticeable when SS1 processors malfunctioned and
leaked. Poor ventilation and high environmental temperatures
were noted by workers. Although gloves, sleeves and aprons are
provided, some workers reported not using all available PPE due
to high environmental temperatures. Two workers reported prior
chemical burns from occupational exposure to Steris 20 Sterilant
Concentrate. Several workers reported that they had not received
formal chemical hazard communication training for Steris room
operations.
A review of FDA CDRH data files indicated that occupational
exposure to peracetic acid sterilant should be unlikely when
SS1 processors are maintained and operated properly and when
technicians follow the manufacturer’s operating procedures.
However, processor malfunctions and improper handling and
disposal of Steris 20 Sterilant Concentrate containers can result
in dermal or inhalation exposures. Appropriate employee training,
Exposure to peracetic
acid sterilant is unlikely
when SS1 processors
are maintained and
operated properly and
when technicians follow
the manufacturer’s
operating procedures.
Processor malfunctions,
and improper handling
and disposal of Steris
20 Sterilant Concentrate
containers can result
in dermal or inhalation
exposures.
su m m A R y

Page vi
Health Hazard Evaluation Report 2006-0298-3090
su m m A R y
(C o n t i n u e d )
use of adequate PPE, and routine maintenance of processors
should help reduce the likelihood of worker exposures, as well as
the risk of employee illness or injury if a spill or leak does occur.
Keywords: NAICS 622110 (General Medical and Surgical
Hospitals), endoscope reprocessing, endoscope sterilization,
peracetic acid, anosmia, chemical burns, dyspnea, eye irritation,
sense of smell, shortness of breath.

Page 1
Health Hazard Evaluation Report 2006-0298-3090
in t R o d u C t i o n
In July 2006, NIOSH received a confidential HHE request from
employees at Kaleida Health-Buffalo General Hospital in Buffalo,
New York. The HHE request stated that inadequate ventilation was
provided in the A2 GI Lab Steris Room where five employees clean
and sterilize endoscopes using Klenzyme® Enzymatic Cleaner and
Steris® 20 Sterilant Concentrate. Health problems identified in
the request were headache, shortness of breath, eye irritation, and
diminished sense of smell.
Background
Management representatives told us that SS1 had been used
at BGH for approximately 10 years prior to our site visit. SS1
was introduced into BGH as a replacement for ethylene oxide
sterilization. During the opening conference, management noted
that health complaints from employees in the A2 GI Lab Steris
Room began in approximately May 2006, following renovations
in that area. Full-shift air sampling conducted by a consultant
in June 2006 indicated that airborne concentrations of acetic
acid were less than 0.2 ppm. Although management was not
aware of spills involving SS1 processors, employees had reported
occasional leaks. In November 2006, SS1 processors were inspected
by a representative from Steris Corporation who identified no
problems.
The A2 GI Lab Steris Room is one of several Steris rooms at BGH.
Although referred to as a single room, the A2 GI Lab Steris Room
is divided into two small rooms (“dirty side” and “clean side,”
which are separated by a floor-to-ceiling wall with a sliding window.
The dirty side adjoins a hospital corridor along a 6-foot wall, which
has a single doorway for entry. The length of the room extends
approximately 15 feet from the corridor. The dirty side contains a
stainless steel counter and sink along the 15-foot wall that separates
the dirty and clean sides. The window between these rooms is
located a few feet from the most interior wall. Each of these rooms
has a plumbed eyewash station.
The clean side is approximately 10 feet wide by 15 feet long, with a
single doorway to the corridor. Three SS1 processors are installed
on a stainless steel counter near the window between the dirty and
clean sides. Two processors are located along the back wall and
one along the wall opposite the window. Also along this wall is a
GUS® Model G17HS endoscope immersion unit, which contains
approximately one-half gallon of Cidex® OPA Solution. The GUS
unit is a compact, ductless vapor control system that exhausts into
the room via a carbon filter. It is our understanding that the GUS

Page 2
Health Hazard Evaluation Report 2006-0298-3090
in t R o d u C t i o n
(C o n t i n u e d )
unit is used infrequently for endoscope disinfection; however,
Cidex OPA remains in the unit at all times.
A canopy hood is mounted on the ceiling of the clean side against
the wall separating the two small rooms and the most interior
(back) wall (the hood is open on two sides). The sides of the hood
extend downward to within approximately 4 feet above four of the
six processors. The Steris room is provided with ceiling diffusers
and returns for general ventilation. Facilities staff informed us that
the Steris room is supplied with 100% outside air.
When an endoscopic procedure is completed, the endoscope is
brought to the dirty side where a technician manually cleans it
using Klenzyme® enzymatic cleaner. After cleaning, the endoscope
is passed through the sliding window to a technician in the clean
side. The clean side technician installs the appropriate channel
connectors, places the endoscope in a processing tray in one of
the SS1 processors along with a sealed container of Steris 20
Sterilant Concentrate, closes the processor lid, and starts the
microprocessor-controlled operating cycle. When the approximately
30-minute sterilization cycle is finished, the technician opens the
processor, removes the endoscope, flushes it with 120 milliliters
of isopropyl alcohol, and purges cavities within the endoscope
with forced air to remove the alcohol. This procedure is repeated
for each endoscope that is returned for cleaning and sterilization.
More than one processor may be operating at any given time. The
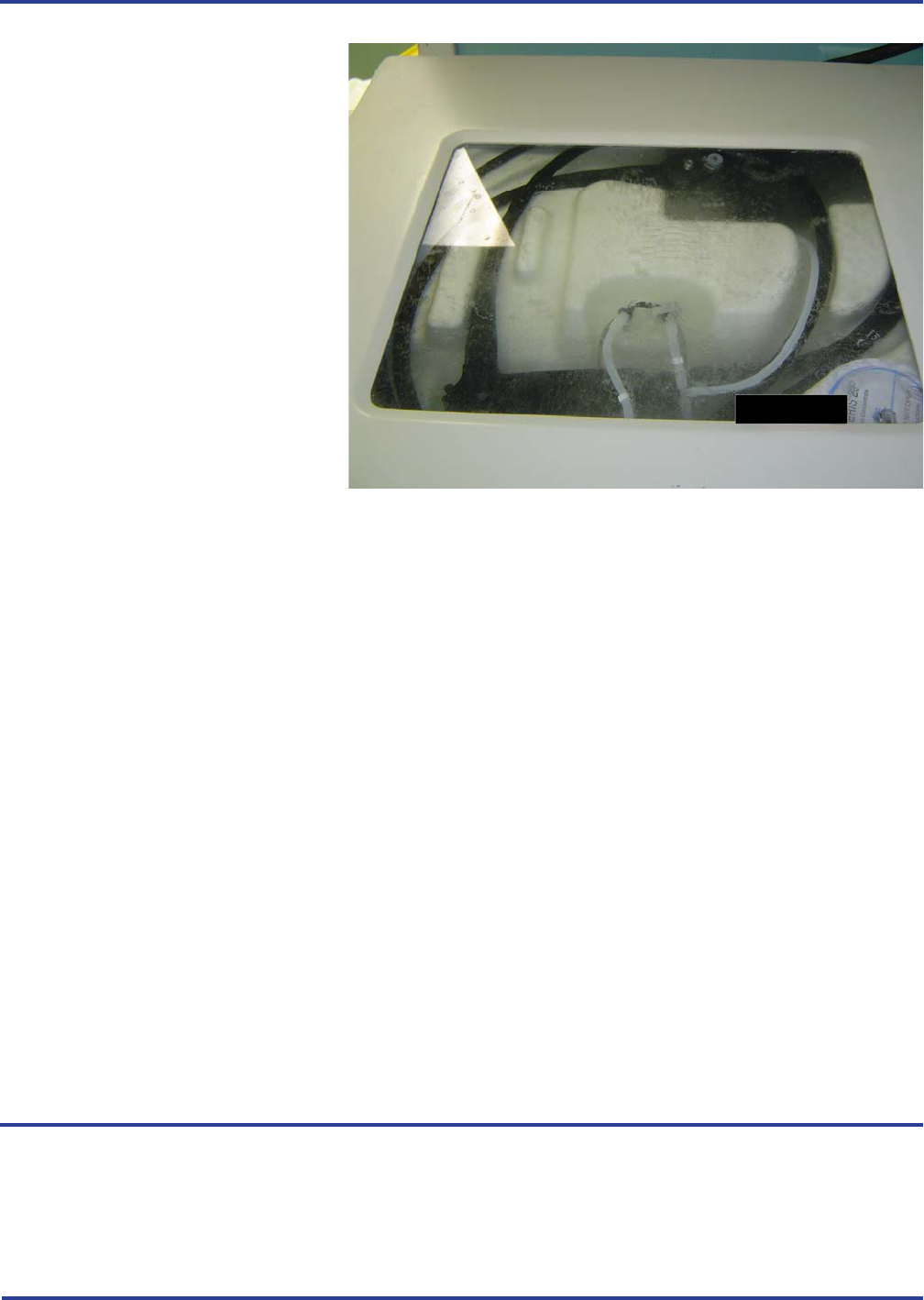
Figure 1. Steris System 1® processor in operation

Page 3
Health Hazard Evaluation Report 2006-0298-3090
in t R o d u C t i o n
(C o n t i n u e d )
only PPE that we observed being worn in the clean side during our
site visit was latex gloves.
Each SS1 processor is a fully-enclosed tabletop unit. Steris 20
Sterilant Concentrate is provided in sealed single-use containers
(“cups”) that hold 2.02 fluid ounces (67.5 grams) of liquid and
163.7 grams of powder. The composition of the liquid (% by
volume) is 35.5% peracetic acid, 40.0% acetic acid, 6.5% hydrogen
peroxide, and 1.0% sulfuric acid [Steris 1995]. The solid powder
consists of proprietary builders and buffers [Alfa 2004; Steris
2007]. During the sterilization cycle, the processor aspirates
the concentrated liquid sterilant, and dilutes it to a working
concentration of 0.2% PAA at a pH of 6.4 and a temperature
of 50ºC to 56ºC [Alfa 2004; Steris 2007]. When diluted, PAA
hydrolyzes to acetic acid and hydrogen peroxide with a half-life
of less than 20 minutes at 50ºC [Steris 1995]. The 0.2 % PAA
solution circulates around and through the endoscope for 12
minutes before being discharged into the sewer system. After the
sterilant has been discharged from the processor, the processor
flushes the endoscope four times with filtered water [Alfa 2004;
Steris 2007; Steris 2008]. The technician can open the processor
after the final rinse water has been discharged down the drain.
Figure 2. Row of Steris System 1® processors
Page 4
Health Hazard Evaluation Report 2006-0298-3090
in t R o d u C t i o n
(C o n t i n u e d )
Contact with Steris 20 Sterilant Concentrate can cause severe
irritation and burns to eyes and skin. Animal studies indicate
that Steris 20 Sterilant Concentrate may be a sensitizer [Steris
1995]. Inhalation of PAA vapor may cause pulmonary edema and
sensitization [IPCS 1994a; Sciencelab.com 2005]. No OELs have
been established for PAA [NJDHSS 1998a].
Contact with acetic acid can cause severe irritation and burns
to the eyes and skin. Inhalation exposure can cause respiratory
irritation, bronchitis, pharyngeal edema, and pulmonary edema
[IPCS 1994b; Hathaway et al. 1996; NJDHSS 1998b]. The NIOSH
REL for acetic acid is 10 ppm for up to 10 hours per workday
during a 40-hour workweek. OSHA and ACGIH have established
8-hour TWA OELs of 10 ppm for acetic acid. In addition, NIOSH
and ACGIH recommend that exposures to acetic acid not exceed
15 ppm during any 15-minute exposure during the course of the
day (short-term exposure limit) [ACGIH 2009; NIOSH 1992]. The
odor threshold for acetic acid is reported to be approximately 0.48
to 1.0 ppm [NJDHSS 1998b].
In response to the HHE request, we conducted a site visit on
December 18–19, 2006. The evaluation included an opening
conference, a walk-through of the A2 GI Lab Steris Room,
Figure 3. Steris System 1® processor in operation showing Steris 20
Sterilant Concentrate container in lower right corner of the processor.
As s e s s m e n t

Page 5
Health Hazard Evaluation Report 2006-0298-3090
As s e s s m e n t
(C o n t i n u e d )
air sampling for peracetic and acetic acids, measurements of
temperature and RH
,
and confidential informal interviews with
several employees.
Full-shift PBZ air samples were collected for each of the three
technicians who were working in the Steris room on December
19. Two area air samples were collected in the clean side. One
area air sample was collected in the dirty side at the open window
between the dirty and clean sides. Air samples were collected on
ORBO™ 53 activated silica gel tubes at a nominal flow rate of 100
mL/min. Samples were analyzed for PAA and acetic acid by high
performance liquid chromatography according to a NIOSH draft
method. Draeger® short-term colorimetric detection tubes were
used to measure the airborne concentration of acetic acid in the
clean side while four processors were in operation. These tubes
have a standard measurement range of 5 to 80 ppm during a 30
second sampling period [Draeger 2009].
Temperature and RH were measured in the clean side using a
hand-held, battery operated, TSI Model 8722 TH-Calc™ Thermal
Hygrometer (TSI Inc., Shoreview, Minnesota). This instrument
measures temperature and RH in the ranges of 32ºF to 140ºF and
5% to 95% RH. A ventilation smoke tube was used to visualize
airflow patterns within the Steris room and to determine if the
clean and dirty sides were under positive or negative pressure
relative to each other and to the adjoining corridor.
Confidential, voluntary interviews were conducted with employees
who work in the A2 GI Lab Steris Room. Employees were asked
about potential work-related health symptoms, safety and health
training, PPE use, chemical exposure incidents, and indoor
environmental quality.
Industrial Hygiene
Air samples did not contain detectable concentrations of acetic
acid. The analytical LOD for acetic acid in the air samples was
approximately 25 micrograms of acetic acid per sample [Neumeister
2009]. Based on the LOD and the average volume of the PBZ
samples (20.1 liters), acetic acid concentrations in these samples
were no greater than 0.5 ppm. The three area air samples, which
had an average sample volume of 43 liters, indicated that acetic
acid concentrations were no greater than 0.24 ppm. Draeger
colorimetric detector tubes did not detect acetic acid in the clean
side.
Re s u l t s

Page 6
Health Hazard Evaluation Report 2006-0298-3090
Re s u l t s
(C o n t i n u e d )
We attempted to quantitate PAA using a draft NIOSH method
originally intended for acetic acid; however, PAA coeluted with
the solvent front during analysis, which prevented separation and
quantitation of PAA. Further efforts to resolve PAA in the samples
were not made because (1) acetic acid (a major component of Steris
20 sterilant) was not detected above the LOD; (2) although PAA
coeleuted with the solvent front, the area of the chromatogram
peak was consistent with the area of the blank samples,
indicating that PAA was not present in large quantity; and (3)
no acid odor was detected during the sampling visit [Neumeister
2009].
Temperatures in the clean side between 8:50 a.m. and 1:15 p.m.
were 74ºF to 76ºF, and RH was between 17% and 20%. Smoke
tube visualization of airflow at the ceiling-mounted ventilation
supply diffusers and return grilles in the clean side indicated that
the HVAC system provided insufficient airflow. No air appeared
to be coming from the supply diffusers. The open doors between
the Steris room and the corridor served as the source of make-
up air for the canopy hood; there was no other source of outside
air. The dirty side appeared to be under slight negative pressure
relative to the corridor, while the clean side was under negative
pressure relative to the corridor and the dirty side, causing air
to flow toward the clean side and out through the canopy hood.
Turbulence beneath the canopy hood in the clean side caused
smoke to drift away from the Steris processors, rather than being
immediately captured and exhausted by the hood.
Interviews
Confidential, voluntary interviews were conducted with four of five
employees who work in the A2 GI Lab Steris Room; one employee
was on extended family leave and not available to participate. The
median length of employment at BGH was 14 years; however, the
median length of employment in the A2 GI Lab Steris Room was
13 months, and three of the four employees had worked in the
department less than 14 months. Workers reported no formalized,
documented initial or refresher hazard communication training
in their current assignment at BGH; however, such training had
been provided when they were employed in other sections of the
hospital. On-the-job training was provided by coworkers with
longer tenure in the department; however, two of four employees
did not know the proper procedures for responding to a chemical
spill or SS1 processor malfunction and overflow.

Page 7
Health Hazard Evaluation Report 2006-0298-3090
Re s u l t s
(C o n t i n u e d )
Three employees reported periodic headaches and burning eyes;
these symptoms were worse when the processors malfunctioned
and overflowed, or when excessive liquid was left in the bottom
of the machine after completion of a sterilization cycle. Poor
ventilation and high environmental temperatures were common
complaints among workers; these conditions were reportedly
worse during the summer. Workers reported leaving the doors
between both sides of the Steris rooms and the corridor open to
improve ventilation, but are instructed by supervisors to keep these
doors closed, reportedly due to odor complaints from patients
and nursing staff. PPE in the form of chemically resistant, sleeve
protectors and aprons are provided by management; however,
some workers reported not using all available PPE due to high
environmental temperatures. Two workers reported having had
chemical burns from prior use of Steris 20 Sterilant Concentrate.
On the day of our site visit, we did not smell an acid odor, which
we would have noticed if airborne acid vapor concentrations had
approached the OELs for acetic acid. This observation is consistent
with air sampling results, which indicate that airborne levels of
acetic acid were below the analytical LOD. Although exposure
limits have not been established for PAA, the sampling results and
our onsite observations indicated little, if any, airborne exposure to
PAA on the sampling date.
Although we do not know the specific sources of odors reportedly
emitted from the Steris room, odor complaints from patients and
nursing staff suggest that the ventilation in the Steris room is
inadequate. Odor complaints, worker reports of uncomfortably
warm temperatures especially during the summer, and our
observations during the site visit point to a need for increasing the
general ventilation in the Steris room.
While Klenzyme Concentrate Plus Enzymatic Cleaner and
Cidex OPA Solution were not the focus of this investigation,
it is important to note hazards associated with these products.
Klenzyme, which can irritate the skin and eyes, contains proteolytic
enzymes, also known as subtilisins. Subtilisins in powder form
are a known respiratory sensitizer. In 2001, researchers reported
a case of extrinsic allergic alveolitis in a hospital worker who was
exposed to subtilisins in Klenzyme that the worker used to wash
surgical instruments and clean operating room surfaces [Tripathi
and Grammer 2001]. OPA is an eye, skin, and respiratory irritant
that may also cause sensitization [Advanced Sterilization Products
2007]. A 2006 article describes a case of occupational asthma and
di s C u s s i o n

Page 8
Health Hazard Evaluation Report 2006-0298-3090
di s C u s s i o n
(C o n t i n u e d )
dermatitis that is believed to be due to exposure to OPA in an
endoscopy unit [Fujita et al. 2006]. BGH employees and managers
should be aware of the hazards associated with these materials.
The FDA CDRH maintains Adverse Event Reporting Data Files
that consist of voluntary reports, user facility reports, distributor
reports, and manufacturer reports of medical devices that may
have malfunctioned or caused a death or serious injury [USFDA
2009]. To better understand workplace hazards during endoscope
reprocessing, we searched the online CDRH data files for adverse
event reports received in 1996 through 2008 that involved SS1.
Reports involving SS1 were reviewed to identify factors related to
worker safety and health at all medical facilities that had submitted
reports, or that were described in reports.
Steris 20 Sterilant Concentrate was involved in approximately
50% of the 63 adverse event reports identified during our review.
Worker exposure was noted in all but one of these reports.
More than 80% of reported exposures to concentrated PAA
sterilant resulted in worker injury; most of these incidents
occurred while handling a sealed Steris 20 Sterilant Concentrate
cup prior to placing the cup into a processor, or while disposing
of incompletely emptied cups at the end of a sterilization cycle.
The most common type of injury was a chemical burn of the skin,
which varied from what appeared to be minor burns, to several
reports of second degree burns, and at least one report of a third
degree burn. Several instances of eye contact that reportedly
resulted in burns and pain were identified. Respiratory exposures
to concentrated PAA sterilant resulted in reports of shortness of
breath; nasal irritation and scabbing of nasal passages; and rare
events, including lung hypertension and pneumonia, and an
asthmatic-like reaction in a hospital receptionist.
Eight reports noted that hospital workers were burned when the
seal on unopened cups ruptured as the workers squeezed the cups
to break up powdered buffers. As reported in three manufacturer
narratives, the manufacturer’s instructions state that “powders
can be broken up by gently squeezing the bottom portion of the
Steris 20 container.” The manufacturer narratives attributed these
incidents to improper handling by the workers. These incidents
resulted in reports of burns on hands, arm, eyes, face, neck,
and abdomen. In one instance, concentrated PAA sterilant was
reportedly splashed onto the eyes, face, and neck of a bystander.
In two instances, a cup lid “popped” or leaked as a cup was being
removed from its carton.

Page 9
Health Hazard Evaluation Report 2006-0298-3090
di s C u s s i o n
(C o n t i n u e d )
Ten reports described incidents involving disposal of cups that
had expired, or that had not been completely emptied during
a sterilization cycle. In most cases, the exposure occurred to
the worker who was disposing of the cup; however, two reports
noted burns due to contact with concentrated sterilant spilled on
work surfaces or furniture, and in one instance, a housekeeping
employee reported shortness of breath that was attributed to
a Steris cup that had been thrown in the trash. Other reports
describe skin and eye contact with concentrated sterilant as a result
of cup leaks, improper sterilant storage, and spray released while
inserting or removing the SS1 aspirator into/from the sterilant
cup.
Only eight reports were identified in which PPE was mentioned.
Of these, five noted that PPE had not been used by the exposed
worker, and two indicated that the PPE was inadequate. Based on
the descriptions of dermal and eye exposures to concentrated PAA
sterilant, it appears that worker injuries could have been prevented
if appropriate PPE had been used.
Twenty-five reports appear to involve releases of 0.2% PAA sterilant
(“use dilution”) from SS1 processors. Failure of the inflatable
processor lid seal was reported as the cause of most processor leaks.
Other leaks occurred when the processor lid opened suddenly
during a sterilization cycle, or when defective endoscope trays
were used. Only six releases of dilute sterilant resulted in reports
of worker exposure. Four reports identified health effects such as
eye, skin, or respiratory irritation. Two reports of exposure during
cleanup of dilute sterilant described respiratory difficulties: in one
instance, a worker was treated with a nebulizer after cleaning a
dilute sterilant spill for 10 minutes, and in the second instance, a
worker was treated for reactive airways dysfunction syndrome after
cleaning a spill for 15 minutes.
Exposure to peracetic acid sterilant is unlikely when SS1 processors
are maintained and operated properly, and technicians follow
the manufacturer’s operating procedures; however, processor
malfunctions, improper handling and disposal of Steris 20
Sterilant Concentrate containers, and nonroutine events can result
in dermal or inhalation exposures. Even though the sterilant cups
are designed to prevent exposure to PAA sterilant, rough handling
and accidental or forceful squeezing can result in exposure to
the concentrated acid. Appropriate employee training, use of
adequate PPE, and routine maintenance of equipment should
help reduce the likelihood that such events will occur, and also
Co n C l u s i o n s

Page 10
Health Hazard Evaluation Report 2006-0298-3090
di s C u s s i o n
(C o n t i n u e d )
Re C o m m e n d A t i o n s
reduce the risk of employee illness or injury if a spill or leak does
occur. Ventilation in the Steris room appears to be insufficient
for providing reliable odor control and maintaining the work
environment within an acceptable range of temperature and RH.
The following recommendations are provided to improve the safety
and health of hospital staff that clean and sterilize endoscopes at in
the A2 GI Lab Steris Room.
Training
Conduct and document hazard communication training ●
required by the OSHA Hazard Communication Standard
(29 CFR 1910.1200). Training should be provided for new
and current employees, and should be designed specifically
for A2 GI Lab Steris Room workers. Training should
address chemical hazards, exposure controls, and PPE for all
chemicals used to process endoscopes, including Steris 20
Sterilant Concentrate, Klenzyme Concentrate Plus Enzymatic
Cleaner and Cidex OPA Solution.
Conduct training for Steris room employees that addresses ●
standard operating procedures in the event of chemical
spills, processor malfunctions, and processor leaks. Training
should include notification procedures for contacting
Environmental Services for spill cleanup.
Contact Steris Corporation to request new employee initial ●
and annual refresher inservice training for SS1 processor
operators. Training should include routine and nonroutine
processor operations, handling of unopened sterilant cups,
and disposal of incompletely aspirated and expired cups.
Annual refresher training would allow a Steris representative
to review technicians’ technique, and to provide instructions
for the proper use and handling of Steris 20 Sterilant
Concentrate.
Personal Protective Equipment
Given the serious nature of injuries that may result from ●
exposure to Steris 20 Sterilant Concentrate, appropriate PPE
should be worn by workers when handling both sealed and
used containers of Steris 20 Sterilant Concentrate.

Page 11
Health Hazard Evaluation Report 2006-0298-3090
Re C o m m e n d A t i o n s
(C o n t i n u e d )
Minimum PPE worn while performing routine tasks ●
involving the handling of sealed Steris cups should include
tight-fitting splash-resistant goggles, acid-resistant sleeves
and apron, and gloves made of butyl rubber, neoprene
rubber, Viton®, or Barrier® [Forsberg and Mansdorf 2007].
Very thin gloves, as typically worn in healthcare settings,
provide poor chemical resistance and mechanical strength,
and should not be the only barrier between the wearer and
a chemical hazard, such as PAA [Forsberg and Mansdorf
2007]. Latex gloves do not provide appropriate protection
and introduce a known allergen into the workplace [NIOSH
1997].
If sterilant remains in a cup at the end of a sterilization ●
cycle, the technician should don additional face protection
(e.g., face shield in addition to gloves, sleeves, apron, and
eye protection used during normal operations). This PPE
should be worn when handling unsealed cups containing
any sterilant concentrate, and when disposing of expired
sterilant.
Preventive Maintenance and Equipment
Malfunctions
SS1 processors should be inspected periodically for ●
components that can fail due to normal wear, resulting in a
leak or worker exposure. These components include aspirator
tubing, processor lid seal, and endoscope trays.
Employees should notify management of all spills, leaks, ●
and equipment malfunctions so that the causes of these
events can be identified and appropriate corrective actions
can be taken. BGH should notify Steris Corporation of
equipment malfunctions and request assistance from Steris
in diagnosing and correcting problems.
Ventilation and Indoor Environmental
Quality
The Steris room must be under negative pressure relative to ●
all surrounding areas in order to control odors. The HVAC
system serving the Steris room should exhaust completely
to the outdoors, i.e., no recirculation. The dirty side should
be under negative pressure relative to the clean side to help
prevent migration of bioaerosols from the dirty side to the
clean side.

Page 12
Health Hazard Evaluation Report 2006-0298-3090
Re C o m m e n d A t i o n s
(C o n t i n u e d )
Re f e R e n C e s
A minimum of 10 air changes per hour should be provided ●
in the Steris room, with a minimum of 2 air changes
of outside air per hour [ASHRAE 2003; ACGIH 2007;
ASHRAE 2007].
Supply diffusers and return grilles need to be located so that ●
supply air reaches room occupants without “short circuiting,”
i.e., flowing directly from supply diffusers to return ducts
without ventilating the occupied space.
ASHRAE recommends maintaining sterilizer equipment ●
rooms between 72ºF and 76ºF, with RH between 30% and
60% [ASHRAE 2007].
Ensure that the GUS Vapor Control System is operating ●
whenever it contains OPA, and that the charcoal filters are
changed every 6 months or as advised by PCI Medical, Inc
[PCI 2009].
ACGIH [2007]. Industrial ventilation: a manual of recommended
practice for design. 26
th
ed. Cincinnati, OH: American Conference
of Governmental Industrial Hygienists.
ACGIH [2009]. 2009 TLVs® and BEIs®: threshold limit values for
chemical substances and physical agents and biological exposure
indices. Cincinnati, OH: American Conference of Governmental
Industrial Hygienists.
Advanced Sterilization Products [2007]. Material safety data sheet,
CIDEX® OPA solution. MSDS-09588-0-001, Rev. F. Irvine, CA:
Advance Sterilization Products. [www.sterrad.com/Customer_
Support/user_resources/msds/cidexopa_msds.pdf]. Date accessed:
March 30, 2009.
Alfa MJ [2004]. SYSTEM 1® Sterile Processing System: liquid
chemical sterilization anthology. [www.steris.com]. Date accessed:
March 23, 2009.
ASHRAE [2003]. HVAC design manual for hospitals and clinics.
Atlanta, GA: American Society of Heating, Refrigerating, and Air-
Conditioning Engineers, Inc.
ASHRAE [2007]. The ASHRAE handbook—HVAC applications.
Atlanta, GA: American Society of Heating, Refrigerating, and Air-
Conditioning Engineers, Inc.

Page 13
Health Hazard Evaluation Report 2006-0298-3090
Re f e R e n C e s
(C o n t i n u e d )
Draeger [2009]. Short-term measurements with Dräger-Tubes.
[www.draeger.com]. Date accessed: March 14, 2009.
Forsberg K, Mansdorf SZ [2007]. Quick selection guide to chemical
protective clothing. 5
th
ed. Hoboken, NJ: John Wiley & Sons, Inc.
Fujita H, Ogawa M, Endo YA [2006]. A case of occupational
bronchial asthma and contact dermatitis caused by ortho-
phthalaldehyde exposure in a medical worker. J Occup Health
48(6): 413–416.
Hathaway GJ, Proctor NH, Hughes JP [1996]. Chemical hazards of
the workplace. 4th ed. New York, NY: Van Nostrand Reinhold.
IPCS [1994a]. International chemical safety cards, peracetic acid
(stabilized). ISCS no. 1031, partial update April 2005. Geneva,
Switzerland: World Health Organization, International Programme
on Chemical Safety. [www.cdc.gov/niosh/ipcsneng/neng1031.
html]. Date accessed: July 23, 2009.
IPCS [1994b]. International chemical safety cards, acetic acid.
ISCS no. 0363, partial update October 2005. Geneva, Switzerland:
World Health Organization, International Programme on
Chemical Safety. [www.cdc.gov/niosh/ipcsneng/neng0363.html].
Date accessed: July 23, 2009.
Neumeister CE [2009]. E-mail communication from C.
Neumeister, Division of Applied Research and Technology,
National Institute for Occupational Safety and Health, Centers for
Disease Control, U.S. Department of Health and Human Services
to D. Sylvain. February 3, 2009.
NIOSH [1992]. Recommendations for occupational safety and
health: compendium of policy documents and statements.
Cincinnati, OH: U.S. Department of Health and Human Services,
Centers for Disease Control, National Institute for Occupational
Safety and Health, DHHS (NIOSH) Publication No. 92-100.
NIOSH [1997]. Preventing allergic reactions to natural rubber latex
in the workplace. Cincinnati, OH: U.S. Department of Health and
Human Services, Centers for Disease Control, National Institute
for Occupational Safety and Health, DHHS (NIOSH) Publication
No. 97-135.
NJDHSS [1998a]. Hazardous substance fact sheet, peroxyacetic
acid. RTK substance no. 1482, revised October 2004. Trenton, NJ:

Page 14
Health Hazard Evaluation Report 2006-0298-3090
Re f e R e n C e s
(C o n t i n u e d )
New Jersey Department of Health and Senior Services.
[http://nj.gov/health/eoh/rtkweb/documents/fs/1482.pdf]. Date
accessed: March 14, 2009.
NJDHSS [1998b]. Hazardous substance fact sheet, acetic acid. RTK
substance no. 0004, revised July 2007. Trenton, NJ: New Jersey
Department of Health and Senior Services.
[nj.gov/health/eoh/rtkweb/documents/fs/0004.pdf]. Date
accessed: March 14, 2009.
PCI [2009]. GUS® vapor control systems for OPA and
glutaraldehyde, frequently asked questions. Deep River, CT: PCI
Medical. [www.pcimedical.com]. Date accessed: March 25, 2009.
Sciencelab.com [2005]. Material safety data sheet, peracetic acid,
35%, updated November 11, 2008. Houston, TX: Sciencelab.com,
Inc. [www.sciencelab.com]. Date accessed: March 30, 2009.
Steris [1995]. Product safety data sheet, Steris 20® Sterilant
Concentrate. MSDS No. 612038, revised January 21, 2009.
Mentor, OH: Steris Corporation. [www.steris.com]. Date accessed:
March 26, 2009.
Steris [2007]. SYSTEM 1® Sterile Processing System in-service
checklist. Document ST1006EN.2007-07, August 2007. [www.
steris.com/]. Date accessed: March 26, 2009.
Steris [2008]. SYSTEM 1® Sterile Processing System technical data
document SD707, revised June 1, 2008 [www.steris.com]. Date
accessed: March 30, 2009.
Tripathi A, Grammer LC [2001]. Extrinsic allergic alveolitis from a
proteolytic enzyme. Ann Allergy Asthma Immunol 86(4):425–427.
USFDA [2009]. Adverse event reporting data files. Center
for Devices and Radiological Health, U.S. Food and Drug
Administration, Department of Health and Human Services.
[www.fda.gov/cdrh/mdr/mdr-file-general.html]. Date accessed:
March 24, 2009.

Page 15
Health Hazard Evaluation Report 2006-0298-3090
AC k n o w l e d g m e n t s A n d
AvAilAbility o f Re p o R t
The Hazard Evaluation and Technical Assistance Branch (HETAB)
of the National Institute for Occupational Safety and Health
(NIOSH) conducts field investigations of possible health hazards
in the workplace. These investigations are conducted under the
authority of Section 20(a)(6) of the Occupational Safety and
Health (OSHA) Act of 1970, 29 U.S.C. 669(a)(6) which authorizes
the Secretary of Health and Human Services, following a written
request from any employer or authorized representative of
employees, to determine whether any substance normally found
in the place of employment has potentially toxic effects in such
concentrations as used or found. HETAB also provides, upon
request, technical and consultative assistance to federal, state, and
local agencies; labor; industry; and other groups or individuals to
control occupational health hazards and to prevent related trauma
and disease.
The findings and conclusions in this report are those of the
authors and do not necessarily represent the views of NIOSH.
Mention of any company or product does not constitute
endorsement by NIOSH. In addition, citations to websites
external to NIOSH do no constitute NIOSH endorsement of
the sponsoring organizations or their programs or products.
Furthermore, NIOSH is not responsible for the content of these
websites. All Web addresses referenced in this document were
accessible as of the publication date.
This report was prepared by David Sylvain and John Gibbins of
HETAB, Division of Surveillance, Hazard Evaluations and Field
Studies. Analytical support was provided by Charles Neumeister
of the Division of Applied Research and Technology. Health
communication assistance was provided by Stefanie Evans.
Editorial assistance was provided by Ellen Galloway. Desktop
publishing was performed by Robin Smith.
Copies of this report have been sent to employee and management
representatives at Kaleida Health-Buffalo General Hospital, the
state health department, and the OSHA Regional Office. This
report is not copyrighted and may be freely reproduced. The report
may be viewed and printed at
www.cdc.gov/niosh/hhe. Copies may
be purchased from the National Technical Information Service at
5825 Port Royal Road, Springfield, Virginia 22161.
Below is a recommended citation for this report:
NIOSH [2009]. Health hazard evaluation report: evaluation of worker exposures
to peracetic acid-based sterilant during endoscope reprocessing, Buffalo, NY.
By Sylvain D, Gibbins J. Cincinnati, OH: U.S. Department of Health and Human
Services, Centers for Disease Control and Prevention, National Institute for
Occupational Safety and Health, NIOSH HETA No. 2006-0298-3090.
To receive NIOSH documents or information about
occupational safety and health topics, contact NIOSH at:
1-800-CDC-INFO (1-800-232-4636)
TTY: 1-888-232-6348
E-mail: [email protected]
or visit the NIOSH web site at: www.cdc.gov/niosh.
For a monthly update on news at NIOSH, subscribe to
NIOSH eNews by visiting www.cdc.gov/niosh/eNews.
Delivering on the Nation’s promise:
Safety and health at work for all people
through research and prevention.
National Institute for Occupational
Safety and Health
