
1 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Safety Assurance Factors
for EHR Resilience
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Self Assessment
High Priority Practices
General Instructions
for the SAFER Self Assessment Guides
The SAFER Guides are designed to help healthcare
organizations conduct self-assessments to optimize the
safety and safe use of electronic health records (EHRs) in
the following areas.
▪
High Priority Practices
▪
Organizational Responsibilities
▪
Contingency Planning
▪
System Conguration
▪
System Interfaces
▪
Patient Identication
▪
Computerized Provider Order Entry
with Decision Support
▪
Test Results Reporting and Follow-Up
▪
Clinician Communication
Each of the nine SAFER Guides begins with a Checklist
of “recommended practices.” The downloadable SAFER
Guides provide llable circles that can be used to indicate
the extent to which each recommended practice has been
implemented. Following the Checklist, a Practice Worksheet
gives a rationale for and examples of how to implement
each recommended practice, as well as likely sources of
input into assessment of each practice, and llable elds
to record team members and follow-up action. In addition
to the downloadable version, the content of each SAFER
Guide, with interactive references and supporting materials,
can also be viewed on ONC’s website at www.healthit.gov/
SAFERGuide.
The SAFER Guides are based on the best evidence available
at this time (2013), including a literature review, expert
opinion, and eld testing at a wide range of healthcare
organizations, from small ambulatory practices to large
health systems. The recommended practices in the SAFER
Guides are intended to be useful for all EHR users. However,
every organization faces unique circumstances and will
implement a particular practice differently. As a result, some
of the specic examples in the SAFER Guides for recommend-
ed practices may not be applicable to every organization.
The SAFER Guides are designed in part to help deal with
safety concerns created by the continuously changing land-
scape that healthcare organizations face. Therefore, changes
in technology, clinical practice standards, regulations and
policy, and associated industry practices should be taken into
account when using the SAFER Guides. Periodic self-assess-
ments using the SAFER Guides may also help organizations
identify areas in which it is particularly important to address
the implications of change for the safety and safe use of EHRs.
In some instances, Meaningful Use and/or HIPAA Security Rule
requirements are identied in connection with recommend-
ed practices. The SAFER Guides are not intended to be used
for legal compliance purposes, and implementation of a
recommended practice does not guarantee compliance with
Meaningful Use, HIPAA, or other laws. The SAFER Guides are
for informational purposes only and are not intended to be
an exhaustive or denitive source. They do not constitute
legal advice or offer recommendations based on a healthcare
provider’s specic circumstances. Users of the SAFER Guides
are encouraged to consult with their own legal counsel with
regard to compliance with Meaningful Use, HIPAA, and other
laws. For more information on Meaningful Use, please visit
the Centers for Medicare & Medicaid Services website at
www.cms.gov. For more information on HIPAA, please visit
the HHS Ofce for Civil Rights website at www.hhs.gov/ocr.

2 of 26
SAFER Self Assessment | High Priority Practices
SAFER
Safety Assurance Factors
for EHR Resilience
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
January 2014
Self Assessment
High Priority Practices
Introduction
The High Priority Practices SAFER Guide identies
“high risk” and “high priority” recommended safety
practices intended to optimize the safety and safe use
of EHRs. It broadly addresses the EHR safety concerns
discussed in greater detail in the other eight SAFER
Guides. Assembling a multi-disciplinary safety team is
recommended to complete this guide, as a team will
be best equipped to identify which EHR-related safety
practices should be addressed rst and which of the
other SAFER Guides to turn to next.
The potential benets of EHRs may not be fully
maximized unless the people responsible for their
implementation, maintenance, and use are prepared
for (and manage) the new challenges and risks they
create.
1-6
These new risks are both “social” (involving
people, leadership, workow, and policies) and
“technical” (involving EHR hardware and software and
system-to-system interfaces, congurations, upgrades,
and maintenance). This guide is designed to help the
people responsible for EHR safety in each specic
complex “sociotechnical” healthcare organization
focus on the most important safety challenges and risks
introduced by EHRs.
Completing the self-assessment in the High Priority
Practices SAFER Guide requires the engagement of
people both within and outside the organization (such
as EHR technology developers and diagnostic services
providers). Because this guide is designed to help
organizations prioritize EHR-related safety concerns,
clinician leadership in the organization should be
engaged to assess whether and how any particular
recommended practice affects the organization’s
ability to deliver safe, high quality care. Collaboration
between clinicians and staff members while completing
the self-assessment in this guide will enable an
accurate snapshot of the organization’s EHR status (in
terms of safety) and, even more importantly, should
lead to a consensus about the organization’s future
path to optimize EHR-related safety and quality:
setting priorities among the recommended practices
not yet addressed, ensuring a plan is in place to
maintain recommended practices already in place,
dedicating the required resources to make necessary
improvements, and working together to mitigate the
highest priority safety risks introduced by the EHR.

3 of 26
SAFER Self Assessment | High Priority Practices
SAFER
Safety Assurance Factors
for EHR Resilience
January 2014
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Self Assessment
High Priority Practices
Table of Contents
General Instructions 1
Introduction 2
About the Checklist 4
Checklist 5
Team Worksheet 7
About the Recommended
Practice Worksheets 8
The SAFER Self Assessment Guides were developed by health IT safety researchers and informatics experts:
Joan Ash
, PhD MLS, MS, MBA, Professor and Vice Chair, Department of Medical Informatics and Clinical Epidemiology, School of Medicine,
Oregon Health & Science University;
Hardeep Singh, MD, MPH, Associate Professor of Medicine at the Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medi-
cine and Chief of the Health Policy, Quality and Informatics Program at the Houston VA HSR&D Center of Excellence, and Director of the Houston VA
Patient Safety Center of Inquiry; and
Dean Sittig, PhD, University of Texas School of Biomedical Informatics at Houston, UT–Memorial Hermann Center for Healthcare Quality & Safety.
This guide was developed under the contract Unintended Consequences of Health IT and Health Information Exchange, Task Order HHSP23337003T/HHSP23320095655WC.
The ONC composite mark is a mark of the U.S. Department of Health and Human Services. The contents of the publication or project are solely the responsibility of the authors and do not necessarily represent
the ofcial views of the U.S. Department of Health and Human Services, Ofce of the National Coordinator for Health Information Technology.
4 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Self Assessment
High Priority Practices
About the Checklist
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
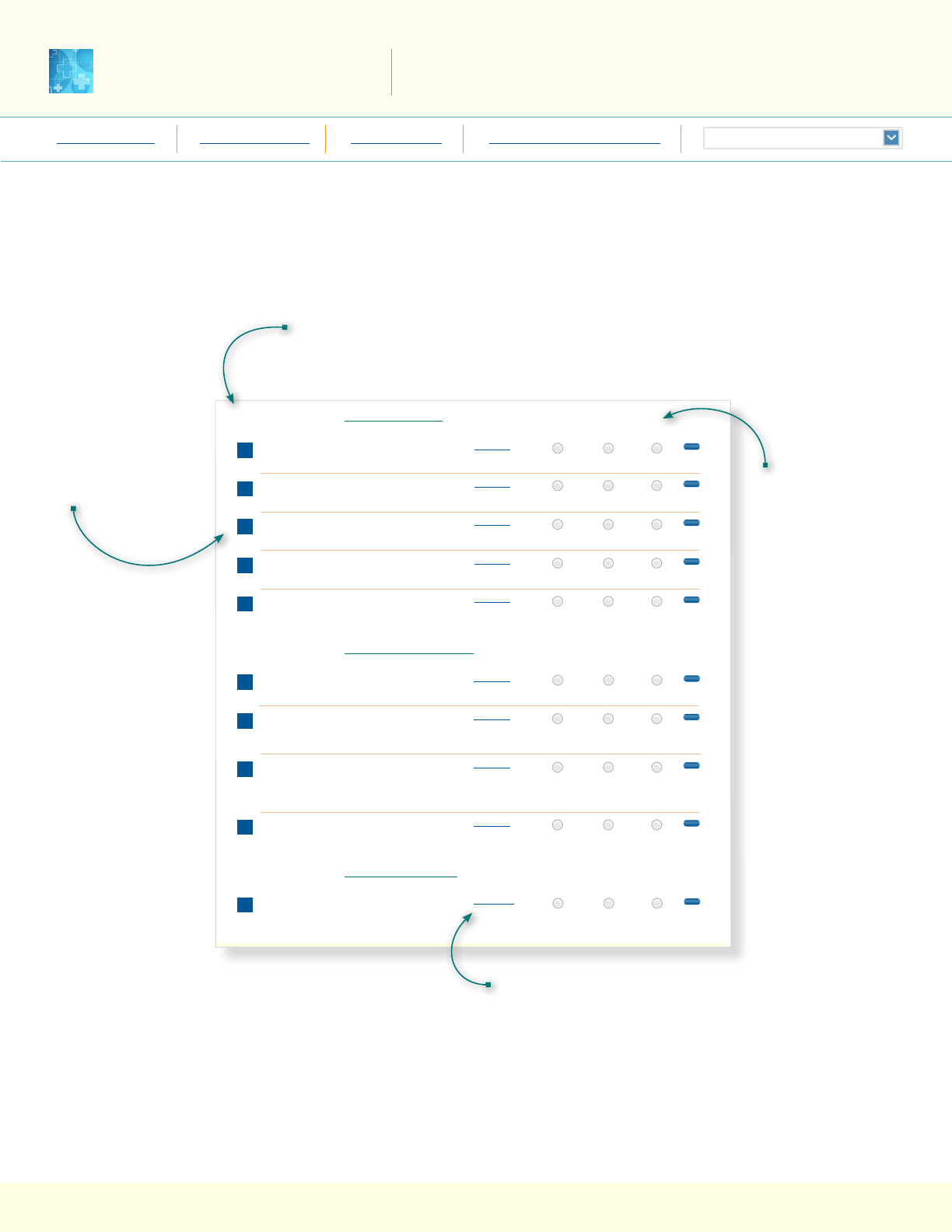
The Checklist is structured as a quick way to enter and print your self-assessment.
Your selections on the checklist will automatically update the related section
of the corresponding recommended practice worksheet.
The Phase associated with the Recommended Practice(s) appears at the top of
the column. Click on the link to access more information about the Phases and
Principles from the website.
Self Assessment
SAFER
5 of 17
Contingency Planning
SAFER Self Assessment | Contingency Planning
December xx, 2013
Checklist
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Recommended Practices for Phase 1 — Safe Health IT
1
Hardware that runs applications critical to the
organization’s operation is duplicated.
Implementation Status
Fully
in all areas
Partially
in some areas
Not
implemented
reset
2
An electric generator and sufcient fuel are available
to support the EHR during an extended power outage.
3
Paper forms are available to replace key EHR functions
during downtimes.
4
Patient data and software application congurations
critical to the organization’s operations are backed up.
5
Policies and procedures are in place to ensure accurate
patient identication when preparing for, during,
and after downtimes.
6
Staff are trained and tested on downtime
and recovery procedures.
7
A communication strategy that does not rely on the
computing infrastructure exists for downtime and
recovery periods.
8
Written policies and procedures on EHR down-
times and recovery processes ensure continuity
of operations with regard to safe patient care and
critical business operations.
9
The user interface of the locally maintained backup,
read-only EHR system is clearly differentiated from
the live/production EHR system.
Worksheet 1
10
There is a comprehensive testing and monitoring
strategy in place to prevent and manage EHR down-
time events.
Worksheet 2
Worksheet 3
Worksheet 4
Worksheet 5
reset
reset
reset
reset
Implementation Status
Fully
in all areas
Partially
in some areas
Not
implemented
reset
Recommended Practices for Phase 2 — Using Health IT Safely
Worksheet 6
Worksheet 7
Worksheet 8
Worksheet 9
reset
reset
reset
Implementation Status
Fully
in all areas
Partially
in some areas
Not
implemented
reset
Recommended Practices for Phase 3 — Monitoring Safety
Worksheet 10
The Recommended
Practice(s) for the
topic appear below
the associated Phase.
Select the level
of Implementation
achieved by your
organization for
each Recommended
Practice.
Your Implementation
Status will be
reected on the
Recommended
Practice Worksheet
in this PDF.
To the right of each Recommended Practice is a link
to the Recommended Practice Worksheet in this PDF.
The Worksheet provides guidance on implementing
the Practice.
Self Assessment
5 of 26
High Priority Practices
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
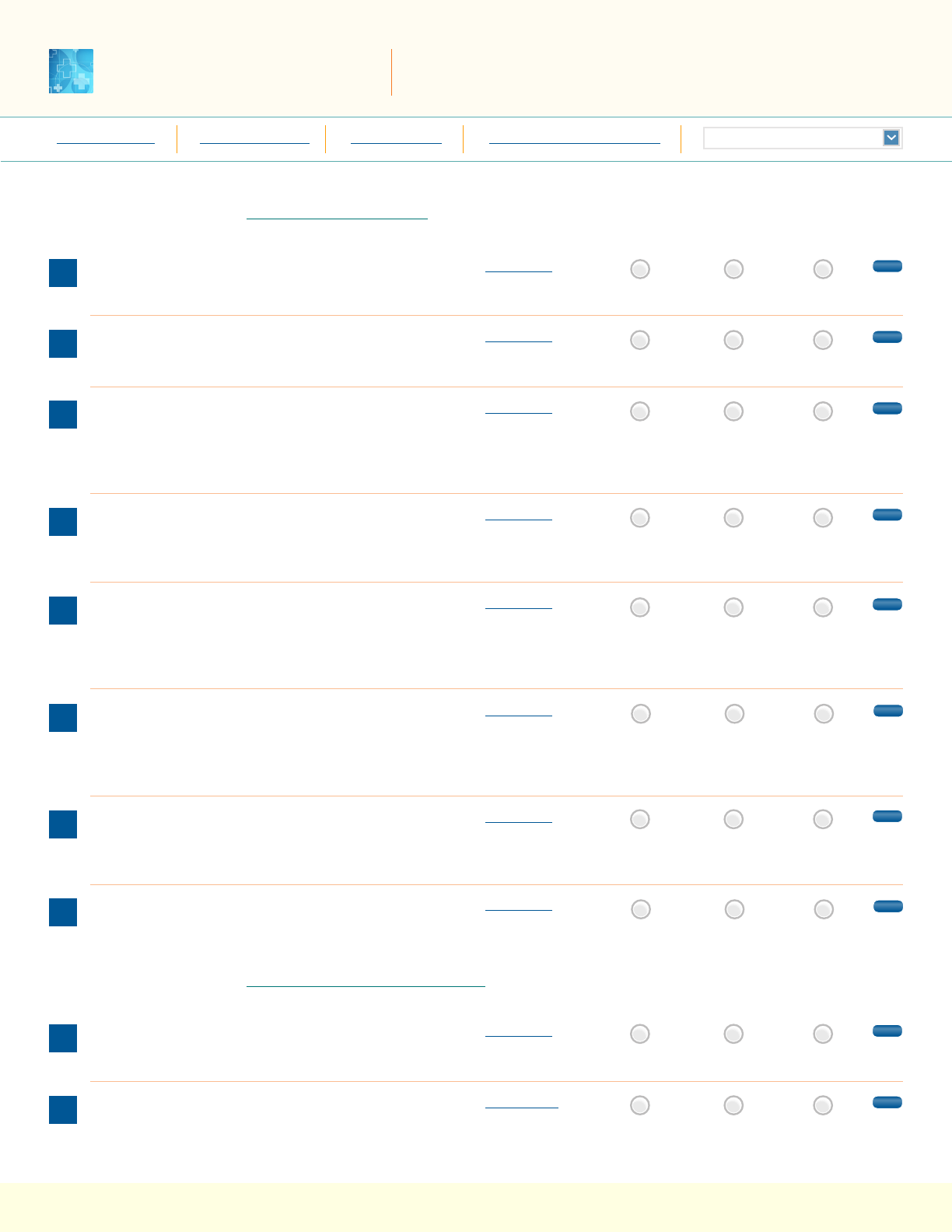
Checklist
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Fully
in all areas
Partially
in some areas
Not
implemented
Implementation Status
Fully
in all areas
Partially
in some areas
Not
implemented
Recommended Practices for Phase 1 — Safe Health IT
1
Data and application congurations are backed up and
hardware systems are redundant.
Worksheet 1
reset
2
EHR downtime and reactivation policies and procedures
are complete, available, and reviewed regularly.
Worksheet 2
reset
3
Allergies, problem list entries, and diagnostic test
results (including interpretations of those results, such
as “normal” and “high”), are entered/stored using
standard, coded data elements in the EHR.
Worksheet 3
reset
4
Evidence-based order sets and charting templates are
available for common clinical conditions, procedures,
and services.
Worksheet 4
reset
5
Interactive clinical decision support features and
functions (e.g., interruptive warnings, passive
suggestions, or info buttons) are available
and functioning.
Worksheet 5
reset
6
Hardware and software modications and system-system
interfaces are tested (pre- and post-go-live) to ensure
data are not lost or incorrectly entered, displayed, or
transmitted within or between EHR system components.
Worksheet 6
reset
7
Clinical knowledge, rules, and logic embedded in the
EHR are reviewed and addressed regularly and whenever
changes are made in related systems.
Worksheet 7
reset
8
Policies and procedures ensure accurate patient
identication at each step in the clinical workow.
Worksheet 8
reset
Recommended Practices for Phase 2 — Using Health IT Safely
9
Information required to accurately identify the
patient is clearly displayed on screens and printouts.
Worksheet 9
reset
10
The human-computer interface is easy to use and
designed to ensure that required information is
visible, readable, and understandable.
Worksheet 10
reset

Self Assessment
6 of 26
High Priority Practices
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Checklist
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Recommended Practices for Phase 2 — Using Health IT Safely
11
The status of orders can be tracked in the system.
Worksheet 11
Implementation Status
Fully
in all areas
Partially
in some areas
Not
implemented
reset
12
Clinicians are able to override computer-generated
clinical interventions when they deem necessary.
Worksheet 12
reset
13
The EHR is used for ordering medications, diagnostic
tests, and procedures.
Worksheet 13
reset
14
Knowledgeable people are available to train, test,
and provide continuous support for clinical EHR users.
Worksheet 14
reset
15
Pre-dened orders have been established for common
medications and diagnostic (laboratory/radiology)
testing.
Worksheet 15
reset
Recommended Practices for Phase 3 — Monitoring Safety
16
Key EHR safety metrics related to the practice/organization
are monitored.
Worksheet 16
Implementation Status
Fully
in all areas
Partially
in some areas
Not
implemented
reset
17
EHR-related patient safety hazards are reported
to all responsible parties, and steps are taken to
address them.
Worksheet 17
reset
18
Activities to optimize the safety and safe use of EHRs
include clinician engagement.
Worksheet 18
reset

Self Assessment
7 of 26
High Priority Practices
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Team Worksheet
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
reset page
A multidisciplinary team should complete this self-assessment and evaluate potential health IT-related patient safety risks addressed
by this specic SAFER Guide within the context of your particular healthcare organization.
This Team Worksheet is intended to help organizations document
the names and roles of the self-assessment team, as well as
individual team members’ activities. Typically team members
will be drawn from a number of different areas within your
organization, and in some instances, from external sources. The
suggested Sources of Input section in each Recommended Practice
Worksheet identies the types of expertise or services to consider
engaging. It may be particularly useful to engage specic clinician
and other leaders with accountability for safety practices identi-
ed in this guide.
The Worksheet includes llable boxes that allow you to document
relevant information. The Assessment Team Leader box allows
documentation of the person or persons responsible for ensuring
that the self-assessment is completed. The section labeled
Assessment Team Members enables you to record the names of
individuals, departments, or other organizations that contributed
to the self-assessment. The date that the self-assessment is
completed can be recorded in the Assessment Completion Date
section and can also serve as a reminder for periodic reassess-
ments. The section labeled Assessment Team Notes is intended to
be used, as needed, to record important considerations or conclu-
sions arrived at through the assessment process. This section can
also be used to track important factors such as pending software
updates, vacant key leadership positions, resource needs, and
challenges and barriers to completing the self-assessment or
implementing the Recommended Practices in this SAFER Guide.
Assessment Team Leader
Assessment Completion Date
Assessment Team Members
Assessment Team Notes

Self Assessment
8 of 26
High Priority Practices
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
About the Recommended
Practice Worksheets
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Each Worksheet provides guidance on implementing a specic Recommended Practice,
and allows you to enter and print information about your self-assessment.
Self Assessment
Contingency Planning
11 of 17
SAFER Self Assessment | Contingency Planning
December xx, 2013
reset page
SAFER
Recommended Practice 4
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Recommended Practice
4
Patient data and software application congurations critical
to the organization’s operations are backed up.
HIPAA
Checklist
Implementation Status
Rationale for Practice or Risk Assessment
Backup of mission-critical patient data and EHR system
conguration allows system restoration to a “pre-failure”
state with minimal data loss.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
The organization has a daily, off-site, complete, encrypted
backup of patient data.
6
▪
The off-site backup is tested regularly (optimally on at least
a monthly basis, i.e., complete restore).
7
▪
The content required to congure the system is backed up
on a regular basis (optimally on a monthly basis and before
every system upgrade).
▪
The organization maintains multiple backups,
created at different times.
▪
Backup media are physically secured.
▪
Backup media are rendered unreadable (i.e., use software
to scramble media contents or physically destroy/shred
media) before disposal.
▪
The organization has a “read-only” backup EHR system
that is updated frequently (optimally at least hourly).
▪
The read-only EHR system is tested regularly
(optimally at least weekly).
▪
Users can print from the read-only EHR system.
▪
If there is a “unit-level” read-only backup EHR
system, it is connected to a local UPS or “red plug.”
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
Click on a link below to view the topic online:
»References »Phases & Principles »HIPAA »Meaningful Use
The Rationale section
provides guidance
about “why” the
safety activities
are needed.
The Suggested Sources
of Input section
indicates categories
of personnel
who can provide
information to help
evaluate your level
of implementation.
The Examples section
lists potentially
useful practices or
scenarios to inform
your assessment and
implementation of the
specic Recommended
Practice.
Enter any notes about
your self-assessment.
Enter any follow-up
activities required.
Enter the name
of the person
responsible for the
follow-up activities.
Each Worksheet shows
links to additional
information available
on the website.

9 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFERSAFER
Self Assessment
High Priority Practices
Recommended Practice 1
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Recommended Practice
1
Data and application congurations are backed up and hardware systems
are redundant.
8-10
HIPAA
Checklist
Implementation Status
Rationale for Practice or Risk Assessment
Hardware and software failures are inevitable. Without redun-
dant backup hardware, delays in restoring system operation
can affect business continuity. Without data backups, key
clinical and administrative information can be lost.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Mission-critical hardware systems (e.g., database
servers, network routers, connections to the Internet) are
duplicated.
▪
Data are encrypted and backed up frequently, and
transferred to an off-site storage location at least weekly.
▪
System backups are tested (e.g., restored to the test
environment) on a monthly basis.
See the Contingency Planning Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
reset page

Self Assessment
High Priority Practices
10 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 2
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Recommended Practice
2
EHR downtime and reactivation policies and procedures are complete,
available, and reviewed regularly.
11
HIPAA
Checklist
Implementation Status
Rationale for Practice or Risk Assessment
Failure to prepare for the inevitability of EHR downtimes greatly
increases the potential for errors in patient care during these
difcult times.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Policies describe:
▪ When a “downtime” should be called (including when the EHR
is functionally unavailable [e.g., very slow response time]),
▪ Who will be in charge during the downtime,
▪ How everyone will be notied, and
▪ Who is responsible for entering data collected
during the downtime.
▪
Hospital personnel are trained (and tested annually) in
these procedures.
▪
The organization regularly conducts tabletop downtime and
reactivation simulations or “drills.”
See the Contingency Planning Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
reset page

Self Assessment
High Priority Practices
11 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 3
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Recommended Practice
3
Allergies, problem list entries, and diagnostic test results (including interpreta-
tions of those results, such as “normal” and “high”), are entered/stored using
standard, coded data elements in the EHR.
7,12-21
Meaningful Use
Checklist
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Rationale for Practice or Risk Assessment
Free text data cannot be used by clinical decision support
logic
22
to check for data entry errors or notify clinicians about
important new information.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
EHR developer
Examples of Potentially Useful Practices/Scenarios
▪
RxNorm is used for coding medications and NDF-RT
for medication classes.
▪
SNOMED-CT is used for coding allergens, reactions,
and severity.
▪
SNOMED-CT, ICD-10, or ICD-9 is used for coding clinical
problems and diagnoses.
▪
LOINC and SNOMED-CT are used for coding clinical
laboratory results.
▪
Abnormal laboratory results are coded as such.
See the Computerized Provider Order Entry with Decision
Support Guide and Test Results Reporting and Follow-Up
Guide for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
12 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 4
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
4
Evidence-based order sets and charting templates are available for common
clinical conditions, procedures, and services.
7, 23
Checklist
Rationale for Practice or Risk Assessment
Requiring clinicians to enter individual orders for routine clinical
practices increases risk of overlooking one or more items.
Allowing individual clinicians to create order sets runs the risk
of institutionalizing poor practice.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Clinical content is developed or modied based on
evidence through consensus by experts relying, where
available, on nationally recognized, consensus-based
clinical decision support (CDS) recommendations.
See AHRQ’s Clinical Decision Support Initiative.
▪
Institute for Safe Medication Practices (ISMP) order set
guidelines
24
are used to create order sets.
▪
Order sets exist for the 10 most common clinical conditions
(e.g., management of chest pain), procedures (e.g., insulin
administration and monitoring), and clinical services (e.g.,
admission to labor and delivery).
See the Computerized Provider Order Entry with Decision
Support Guide for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
13 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 5
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
5
Interactive clinical decision support features and functions
(e.g., interruptive warnings, passive suggestions, or info buttons)
are available and functioning.
25-30
Meaningful Use
Checklist
Rationale for Practice or Risk Assessment
Interactive clinical decision support interventions help
reduce the risks associated with ordering inappropriate,
contraindicated, and non-therapeutic doses (i.e., under
or overdoses), and provide just-in-time clinical knowledge
to clinicians.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Each practice identies a minimum number of highly
specic CDS features and functions and monitors their
availability and use.
▪
Appropriate CDS features and functions include:
▪ Alerts for abnormal laboratory test results.
5
▪ Tiered drug-drug interaction checks.
26
▪ Drug-allergy interaction checks.
31
▪ “Reverse allergy” checking occurs when a new
allergen is entered for a patient.
▪ Drug-food interaction support.
▪ Drug-condition interaction checks (e.g., Accutane or tetracycline
prescribed for a pregnant woman).
▪ Drug-patient age interaction checks (e.g., medications
contraindicated in the elderly).
▪ Drug dosing support for maximum (dose, daily, and lifetime),
minimum, renal,
32
weight-based, and age-appropriateness.
See the Computerized Provider Order Entry with Decision
Support Guide for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
14 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 6
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
6
Hardware and software modications and system-system interfaces are tested
(pre- and post-go-live) to ensure data are not lost or incorrectly entered,
displayed, or transmitted within or between EHR system components.
33-36
HIPAA
Checklist
Rationale for Practice or Risk Assessment
Failure to test new or modied hardware and software func-
tions along with system-system interfaces, both pre- and post-
go-live, increases the risk of inadvertent errors and patient
harm. Routine changes can result in unexpected side-effects
leading to incomplete or unreliable functionality.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Hardware and software should be tested both pre- and
post-go-live. Include tests using clearly named “test”
patients (e.g., ZZtest345 with patient ID 999999999)
in the “live” environment.
▪
High-priority clinical processes should be simulated using
real clinicians.
▪
Use the Leapfrog Group’s “Evaluation Tool for
Computerized Physician Order Entry” (or some similar
automated tool) to assess point-of-care CDS intervention
completeness and reliability on a regular basis.
33
▪
Applications and system-system interfaces are tested to
ensure that data are neither lost nor incorrectly entered,
displayed, or transmitted.
▪
Interfaces (e.g., HL-7) capable of sending, receiving,
acknowledging, and cancelling orders and results exist
and are tested between ADT – Laboratory, -Pharmacy,
and -Radiology; and CPOE – Pharmacy, -Laboratory, and
-Radiology.
▪
Error logs are regularly inspected and errors xed.
See the System Conguration Guide, System Interfaces
Guide, and Test Results Reporting and Follow-Up Guide
for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
15 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 7
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
7
Clinical knowledge, rules, and logic embedded in the EHR are reviewed and
addressed regularly and whenever changes are made in related systems.
30, 37-40
Checklist
Rationale for Practice or Risk Assessment
Medical knowledge is constantly evolving. Failure to review
and update clinical content can result in outdated practices
continuing long after they should be discontinued or updated.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Clinical content (e.g., order sets, default values, charting
templates, patient education materials, and health
maintenance reminders) are reviewed at least bi-annually
or as needed (e.g., following user feedback, changes in
clinical practice standards, or manufacturer alert) against
recent evidence and best practices.
See the Computerized Provider Order Entry with Decision
Support Guide for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
16 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 8
Worksheet
Phase 1 —
Safe Health IT
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
8
Policies and procedures ensure accurate patient identication at each step in
the clinical workow.
HIPAA
Checklist
Rationale for Practice or Risk Assessment
Wrong patient charting is one of the more common safety
problems in EHRs and can result in both data integrity and
data condentiality issues when protected health information
is disclosed in the wrong chart and is missing from the right
chart. Accurate and consistent patient identication is one
of the most important patient safety measures in an EHR-
enabled healthcare system.
Suggested Sources of Input
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Information required to facilitate positive patient ID is visible
on all screens and printouts and includes: Last name, rst
name, date of birth (with calculated age in age-appropriate
units), gender, medical record number, in-patient location
(or home address), recent photograph (recommended),
and responsible physician (optional).
▪
The master patient index employs a probabilistic matching
algorithm that uses patient’s rst and last names, date of
birth, gender, and zip code or telephone number or social
security number.
41
▪
The system generates a pop-up alert when a user
attempts to create a record for a new patient or looks up
an existing patient with the same rst and last name as an
existing patient.
▪
Before allowing the user to change the current patient
(and display data for another patient), the system checks
that all entered data have been saved (i.e., signed).
42
See the Patient Identication Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
17 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 9
Worksheet
Phase 2 —
Using Health IT Safely
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
9
Information required to accurately identify the patient is clearly displayed
on screens and printouts.
42,43
Checklist
Rationale for Practice or Risk Assessment
If clinicians cannot clearly identify the patient they are working
on, they are at increased risk of making EHR entries in the
wrong record or relying on information on the wrong patient,
resulting in patient care and treatment errors, which are among
the most common types of errors in the modern EHR-enabled
healthcare system.
Suggested Sources of Input
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Information required for patient ID includes:
▪ Last name
▪ First name
▪ Date of birth (with calculated age)
▪ Gender
▪ Medical record number
▪ In-patient location (or home address)
▪ Recent photograph (optional)
▪ Responsible physician (e.g., attending, PCP, or admitting).
▪
The duplicate patient ID rate (number of patient records
with the same rst name, last name, and date of birth in the
EHR database) is monitored.
See the Computerized Provider Order Entry with Decision
Support Guide and Patient Identication Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
18 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 10
Worksheet
Phase 2 —
Using Health IT Safely
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
10
The human-computer interface is easy to use and designed to ensure that
required information is visible, readable, and understandable.
43-46
Checklist
Rationale for Practice or Risk Assessment
Clinicians are constantly under time pressure. User interfaces
that are difcult to see, comprehend, and use signicantly
increase the risk of error and patient harm.
Suggested Sources of Input
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Visible: columns are wide enough to view critical data.
45
▪
Readable: appropriate font sizes and contrast are used.
▪
Understandable: only standardized abbreviations are used;
the most recent orders and results are clearly marked.
43
▪
Consistent: similar functions have similar labels; different
functions have different labels.
▪
When possible, items that are related, or have similar
functions, are grouped and displayed together rather
than alphabetically.
▪
System response time is adequate (e.g., mean under
3 seconds; max under 10 seconds).
▪
User input data elds are large enough to enter required
information, and selection options are clearly dened and
easy to select.
See the System Conguration Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
19 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 11
Worksheet
Phase 2 —
Using Health IT Safely
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
11
The status of orders can be tracked in the system.
7
Checklist
Rationale for Practice or Risk Assessment
Errors often occur when users assume that orders entered
into the computer will be done as specied. To facilitate closed
loop communication and tracking of tasks and orders, the EHR
should provide users with information regarding their status.
Suggested Sources of Input
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Users are notied of key actions (or inactions) relating
to their orders, such as when ordered medications get
discontinued (manually or automatically), antibiotic
renewals are not processed, and when orders placed
at later times of the day will not be acted upon till the
next day.
▪
Users are able to track the status of orders (e.g., specimen
collected, specimen received, resulted).
▪
There is clear distinction (e.g., different font or color)
between newly entered and copied data.
45
See the Computerized Provider Order Entry with Decision
Support Guide and Test Results Reporting and Folllow-Up
Guide for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
20 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 12
Worksheet
Phase 2 —
Using Health IT Safely
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
»References
Click on a link below to view the topic online:
»Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
12
Clinicians are able to override computer-generated clinical interventions when
they deem necessary.
47,48
Checklist
Rationale for Practice or Risk Assessment
Computers cannot practice medicine. Disallowing clinician
overrides of computer-generated interventions implies that
computers have access to more accurate data and greater
medical knowledge and expertise than clinicians. This is
rarely true.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical
administration
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Hard stop alerts (i.e., the user must take an action before
proceeding) are used only for the most egregious potential
errors. Hard stop alert overrides are closely monitored and
reviewed often.
47
▪
The alert override rate (i.e., the number of point-of-care
alerts that clinicians override divided by the total number of
point-of-care alerts generated) is monitored, and alerts with
high override rates are reviewed.
See the Computerized Provider Order Entry with Decision
Support Guide for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
21 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 13
Worksheet
Phase 2 —
Using Health IT Safely
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
13
The EHR is used for ordering medications, diagnostic tests,
and procedures.
7
Meaningful Use
Checklist
Rationale for Practice or Risk Assessment
Partial EHR use means that clinicians must look in two sepa-
rate places to nd the most recent orders, which increases the
potential to miss or delay lling critical orders. Hybrid systems,
part electronic and part paper, are particularly hazardous.
53
Suggested Sources of Input
Clinicians, support staff,
and/or clinical administration
Diagnostic services
Health IT support staff
Pharmacy
Examples of Potentially Useful Practices/Scenarios
▪
The CPOE rate (i.e., the number of orders electronically
entered by clinicians divided by the total number of orders
entered) is monitored.
▪
The percentage of verbal or paper orders that are entered
by ancillary personnel is less than 10 percent.
▪
Free text and “miscellaneous” orders are discouraged by
providing appropriate supports.
▪
Policies and procedures are in place that clearly identify
and manage hazards associated with ordering that
continues to occur outside of the EHR.
See the Computerized Provider Order Entry with Decision
Support Guide and Test Results Reporting and Folllow-Up
Guide for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
22 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 14
Worksheet
Phase 2 —
Using Health IT Safely
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
14
Knowledgeable people are available to train, test, and provide continuous
support for clinical EHR users.
49
Checklist
Rationale for Practice or Risk Assessment
Clinicians cannot use EHRs safely if they have not been
trained and do not have access to assistance when needed.
EHRs are complex tools. In order to maximize patient safety,
clinicians must not be expected to “learn the basics on the job.”
Suggested Sources of Input
Clinicians, support staff,
and/or clinical administration
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
All clinicians receive training appropriate to their expected
use of the EHR. An assessment is made of the need for
such specialized training beyond system-wide, generic
training.
▪
Trainers have advanced EHR and/or informatics training.
▪
Trainers are available before and after go-live, and provide
on-going support for users during EHR optimization.
49
▪
All clinicians are trained and tested on basic
EHR and CPOE operations before being issued
login credentials.
▪
The clinician training rate (i.e., the number of clinicians
trained to use the EHR who have passed a basic
competency test divided by the total number of clinicians
with EHR user privileges) is monitored.
▪
When any category of clinician users of EHRs requests
training, especially when they also indicate that they are
not adequately trained to safely do their jobs, such training
is promptly provided. Organizations have processes to
identify training opportunities that would optimize the safe
use of EHRs.
See the Organizational Responsibilities Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
23 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 15
Worksheet
Phase 2 —
Using Health IT Safely
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
»References
Click on a link below to view the topic online:
»Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
15
Pre-dened orders have been established for common medications and
diagnostic (laboratory/radiology) testing.
50
Checklist
Rationale for Practice or Risk Assessment
Unnecessary clinical practice variation should be minimized.
Forcing clinicians to enter specic values that are then
matched to a list of allowable values or to select from a set of
possible values increases variability and can result in errors.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical administration
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
Complete medication order sentences exist for the most
commonly ordered medications, laboratory tests, and
radiology studies.
51
See the Computerized Provider Order Entry
with Decision Support Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
24 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 16
Worksheet
Phase 3 —
Monitoring Safety
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
16
Key EHR safety metrics related to the practice/organization are monitored.
52
Checklist
Rationale for Practice or Risk Assessment
Measurement and monitoring of key performance indicators
is essential for improvements in safety.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical administration
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
EHR uptime rate
Minutes the EHR was available to clinicians divided by
number of minutes in the reporting period.
52
▪
System response time
Mean time to display a recent CBC result on a test patient,
measured every minute of every day in the reporting
period.
▪
Serious EHR-related adverse events
A list of reported EHR-related adverse events (whether
they resulted in patient harm or not, including any reported
breaches of patient condentiality).
▪
Potential wrong patient error rate
Requests to “change” orders that result in cancellation of
rst order and the creation of an order for the same item on
a different patient by the same user.
See the Organizational Responsibilities Guide and System
Conguration Guide for related recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
25 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 17
Worksheet
Phase 3 —
Monitoring Safety
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
17
EHR-related patient safety hazards are reported to all responsible parties,
and steps are taken to address them.
Checklist
Rationale for Practice or Risk Assessment
Ensuring that EHR-related patient safety hazards are
systematically identied, reported, and addressed is
essential to improving the safety of EHRs.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical administration
EHR developer
Health IT support staff
Examples of Potentially Useful Practices/Scenarios
▪
The organization clearly identies through policies and
procedures how to address reports of EHR safety hazards.
▪
The organization ensures that reports of hazards and
adverse events are reported, as appropriate, to EHR
developers as well as senior leadership and boards.
▪
The organization has a relationship with a patient safety
organization experienced in investigating and addressing
EHR-related patient safety incidents.
▪
The total number of EHR-related software errors
(i.e., bugs) reported is monitored.
▪
The serious EHR error x rate (i.e., the number of errors
with potential for causing direct patient harm xed within
3 months divided by the total number of errors reported)
is monitored.
See the Organizational Responsibilities Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page

Self Assessment
High Priority Practices
26 of 26
SAFER Self Assessment | High Priority Practices
January 2014
SAFER
Recommended Practice 18
Worksheet
Phase 3 —
Monitoring Safety
>Table of Contents >About the Checklist >Team Worksheet >About the Practice Worksheets
>Practice Worksheets
Implementation Status
Click on a link below to view the topic online:
»References »Phases & Principles »Meaningful Use »HIPAA
Recommended Practice
18
Activities to optimize the safety and safe use of EHRs include
clinician engagement.
Checklist
Rationale for Practice or Risk Assessment
Unless clinicians are included in decisions that affect their
use of the EHR, they may not understand or accept changes,
which increases risks. Clinicians should be engaged in
identifying opportunities for the EHR to support safe and
effective clinical use.
Suggested Sources of Input
Clinicians, support staff,
and/or clinical administration
Diagnostic services
EHR developer
Health IT support staff
Pharmacy
Examples of Potentially Useful Practices/Scenarios
▪
Representatives from the following groups are involved
in decision making about EHR safety: clinicians,
administrators, patients, IT/informatics, board of directors
and CEO, and quality and legal staff.
See the Organizational Responsibilities Guide for related
recommended practices.
Assessment Notes
Follow-up Actions
Person Responsible for Follow-up Action
reset page
