
NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
845
GETTING TO THE GOOD PLACE: IMPLEMENTING NEW JERSEY’S
MEDICAL AID IN DYING FOR THE TERMINALLY ILL ACT
Megan Nigro
*
I. INTRODUCTION
In 2019, New Jersey approved an aid in dying bill and joined several
states that have expanded legal end of life choices to include forms of
physician-assisted death. New Jersey’s Medical Aid in Dying for the
Terminally Ill Act (hereinafter “the Act”) raises interesting questions
about patient choice, but some patients have not been able to use this
choice since the Act became effective on August 1, 2019. Robin Granat,
a former singer and ice skater, diagnosed with an incurable brain tumor,
made an appointment for August 19, 2019, to make her first request for
the aid in dying medication.
1
Before the appointment, a Mercer County
court had already placed a temporary restraining order on the Act.
2
A
few days later, Robin lost her ability to speak and could not make her
first oral request as required by the Act.
3
Other New Jersey patients
have used or still hope to use the Act. Katie Kim, a former pharmacist,
diagnosed with an incurable neuromuscular disorder eight years prior,
wanted to move to a state with an aid in dying law, but her doctors were
*
J.D. Candidate, 2021, Seton Hall University School of Law; B.A., 2018, Wake Forest
University. Many thanks to Professor Carl Coleman for his guidance and to Tracy
Forsyth, Deputy General Counsel at University Hospital, for her support in pursuing this
topic.
1
Lindy Washburn & Stacey Barchenger, She Hoped for Death on Her Own Terms.
Then NJ’s Aid-In-Dying Law Was Challenged, NORTH JERSEY REC. (Aug. 30, 2019, 5:30 AM),
https://www.northjersey.com/story/news/new-jersey/2019/08/30/nj-aid-dying-
law-challenge-prevents-woman-with-brain-cancer-from-ending-life-on-her-own-
terms/2123105001/.
2
Id. The temporary injunction on the use of the Act had been removed, but the
lawsuit continued. Stacey Barchenger, New Jersey’s ‘Aid-in-Dying’ Law Reinstated After
a Pair of Court Rulings, TRENTON BUREAU (Aug. 27, 2019, 10:53 AM), https://www.north
jersey.com/story/news/2019/08/27/nj-aid-dying-law-reinstated-appeals-court/212
9382001. The doctor suing argued that the Act as a whole was unconstitutional, and he
objected to turning over patient records in compliance with the Act. Id. In 2020, the
judge dismissed the case for “failure to state a claim upon which relief may be granted.”
Glassman v. Grewal, No. MER-C-53-19 (N.J. Super. Ct. Ch. Div. Apr. 1, 2020) (order
granting dismissal of complaint).
3
Washburn & Barchenger, supra note 1.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
846 SETON HALL LAW REVIEW [Vol. 51:845
all in New Jersey.
4
When New Jersey allowed a similar choice, she hoped
to use the law to help her die in peace.
5
Within the first several weeks
of the Act, at least one New Jersey resident used the Act to request and
self-administer medication to end her suffering.
6
Zebbie Geller, a retired
teacher, was diagnosed with terminal lung cancer nine months prior
and was told she had only months left to live.
7
From July 2019 to her
death at the end of September 2019, Zebbie and her family contacted 40
doctors before they could find physicians willing to aid in Zebbie’s
death.
8
At eighty-years-old and while surrounded by family, Zebbie
swallowed an anti-nausea pill and apple juice mixed with digoxin, “a
cardiac drug that slows the heart,” and died within 90 minutes.
9
Zebbie’s story depicts how the Act was made to work. Zebbie met the
standard requirements, physicians could personally object to aid in her
dying, and Zebbie could request and self-administer her own
medication.
10
This Comment discusses considerations for implementation for
New Jersey doctors and facilities on behalf of New Jersey patients who
want to participate in successful aid in dying stories like Zebbie’s. As
readers consider this Comment, they should think about these patients
and the myriad of other patients who might choose to request or use aid
in dying medication. This Comment will not discuss whether New Jersey
patients should have the right to make this choice. This Comment will
examine other states and countries where patients have similar end of
life options and make suggestions for New Jersey safeguards and best
practices so the Act may best serve its purpose in providing patients
with this end of life choice and protecting against unintended
consequences and abuse.
While the Act does promise to give patients more choice while
protecting them from coercion, abuse, or neglect, and is partially
modeled after statutes in other states, this Comment argues that New
Jersey can learn from other states and countries in its implementation
4
Susan K. Livio, She Wants to End Her Life Because of Agonizing Pain. ‘Every Day
Katie Asks Me to Help Her Die.’, N.J. ADVANCE MEDIA (Aug. 23, 2019), https://www.nj.com/
news/2019/08/she-wants-to-die-because-of-agonizing-pain-from-incurable-disease-
but-law-that-gave-hope-is-stalled.html.
5
Id.
6
Susan K. Livio, N.J. Woman Used New Law to End Her Life. ‘I’m Ready, Let’s Do It.’, N.J.
ADVANCE MEDIA (Oct. 18, 2019), https://www.nj.com/news/2019/10/nj-woman-used-
new-law-to-end-her-life-im-ready-lets-do-it.html.
7
Id.
8
Id.
9
See id.
10
See id.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 847
and application while considering its unique population and statutory
definitions. Part II introduces the Act and the statutory language
describing the self-administration, residency, and time between
requests requirements and discusses initial concerns with the
definitions and language. Part III analyzes and compares other states’
and countries’ definitions of the three requirements discussed in this
Comment, with an emphasis on the self-administration requirement.
Part IV compares usage and implementation based on a statistical
analysis of census data and state aid in dying reports. Part V converts
these comparisons into considerations for New Jersey’s implementation
and best practices.
II. DEFINITIONS IN NEW JERSEY’S MEDICAL AID IN DYING FOR THE TERMINALLY
ILL ACT
This Part introduces New Jersey’s Medical Aid in Dying for the
Terminally Ill Act and explains three definitions from the Act: self-
administer, resident, and time between requests.
A. Introduction to the Act
In April 2019, after seven years of proposed legislation,
11
Governor
Murphy signed New Jersey’s Medical Aid in Dying for the Terminally Ill
Act.
12
While Governor Murphy grappled with the ethical questions
raised by this legislation, he ultimately wanted New Jersey residents to
have the freedom to make their own end of life choices.
13
The Act itself
states its purpose to continue the state’s “long-standing commitment to
individual dignity, informed consent, and the fundamental right of
competent adults to make health care decisions.”
14
Under the Act, only specific adults will be eligible to make aid in
dying their end of life choice.
15
The Act defines a qualified terminally ill
patient as follows:
[A] capable adult who is a resident of New Jersey and has
satisfied the requirements to obtain a prescription for
medication pursuant to P.L.2019, c.59 (C.26:16-1 et al.). A
11
To read more about the years of legislation, see New Jersey, COMPASSION & CHOICES,
https://compassionandchoices.org/in-your-state/new-jersey/#extended-state-
content (last visited Oct. 29, 2019).
12
Philip D. Murphy, Governor’s Statement Upon Signing Assembly Bill No. 1504 (Apr.
12, 2019), http://d31hzlhk6di2h5.cloudfront.net/20190412/4b/cd/8b/1f/02854e1f1
393a35250679633/A1504.pdf.
13
Id.
14
N.J. STAT. ANN. § 26:16-2 (2019), https://www.njleg.state.nj.us/2018/Bills/PL19/
59_.PDF.
15
§ 26:16-1 to 20.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
848 SETON HALL LAW REVIEW [Vol. 51:845
person shall not be considered to be a qualified terminally ill
patient solely because of the person’s age or disability or a
diagnosis of any specific illness, disease, or condition.
16
Furthermore, “‘[t]erminally ill’ means that the patient is in the terminal
stage of an irreversibly fatal illness, disease, or condition with a
prognosis, based upon reasonable medical certainty, of a life expectancy
of six months or less.”
17
A qualified patient must make three requests
before an attending physician can prescribe aid in dying medication.
18
The Act provides a sample written request form for patients to use as
one of the three requests.
19
The attending physician must also refer the
qualified patient to a consulting physician who may confirm the physical
diagnosis and the patient’s capability to make an informed and
voluntary decision.
20
If either physician has questions or concerns
about a patient’s mental capability, that physician must refer the patient
to a mental health care professional.
21
The Act clarifies twice that any
health care professional or patient who takes action under the Act does
not participate in euthanasia, suicide, assisted suicide, or homicide.
22
Therefore, this Comment respectfully refers to the actions taken under
the Act as furthering aid in dying but uses other states’ and countries’
respective terms, such as euthanasia, when discussing those
jurisdictions’ laws.
B. Defining and Applying Self-Administration
In New Jersey’s statute, “‘[s]elf-administer’ means a qualified
terminally ill patient’s act of physically administering, to the patient’s
own self, medication that has been prescribed pursuant to” the Act.
23
This language impliedly excludes any patient who may otherwise
qualify for the Act but lacks enough physical strength or coordination to
administer their own medication. This may include patients who had an
existing physical disability limiting strength or coordination before
acquiring a terminal illness and becoming otherwise eligible for the Act.
The Act could also exclude a patient who, through the time it takes to
complete the Act’s requirements, loses her strength and ability to self-
administer medication. Remember that Zebbie Geller needed enough
16
§ 26:16-3.
17
Id.
18
§ 26:16-10.
19
§ 26:16.
20
§ 26:16-6.
21
§ 26:16-8.
22
§ 26:16-15, -17.
23
§ 26:16-3.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 849
control of her limbs and head to take a pill and drink a medication.
24
The
Act, however, does not explicitly state that a patient must ingest (rather
than inject) medication, but the requirements discussed herein imply an
expectation that a patient would have the physical ability to ingest the
medication.
Further analysis of the Act demonstrates how the term “self-
administer” imposes certain physical eligibility requirements for
patients beginning with the first request. A patient must complete a
valid written request for the aid in dying medication.
25
A valid written
request must be initialed, signed, and dated by the patient.
26
The Act
requires a patient to have enough physical strength and coordination to
initial, sign, and date a document. The same hypothetical patient
discussed above, who had a physical disability before terminal illness or
who acquired a physical disability since diagnosis of a terminal illness,
could be excluded even before consideration of whether that patient can
physically self-administer if that patient physically cannot complete the
required written request.
C. Defining and Applying Residency
Under the Act, the attending physician who would ultimately
prescribe the aid in dying medication must require the patient to
demonstrate New Jersey residency.
27
The patient must provide the
physician with a copy of:
a. a driver’s license or non-driver identification card issued by
the New Jersey Motor Vehicle Commission;
b. proof that the person is registered to vote in New Jersey;
c. a New Jersey resident gross income tax return filed for the
most recent tax year; or
d. any other government record that the attending physician
reasonably believes to demonstrate the individual’s current
residency in this State.
28
This language allows for a person who previously lived in New
Jersey but currently resides across the accessible borders of New York
or Pennsylvania to continue to utilize a New Jersey driver’s license to
easily access the Act. In becoming a terminally ill patient, a person could
utilize a license with her hometown address to access the Act while
residing in New York City. Patients with terminal illnesses may not have
24
See Livio, supra note 6.
25
§ 26:16-5.
26
§ 26:16-20.
27
§ 26:16-6.
28
§ 26:16-11.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
850 SETON HALL LAW REVIEW [Vol. 51:845
the strength or ability to change states.
29
But an inability to travel
because of a need for particular doctors or lack of strength may be made
easier by the physical proximity of New Jersey’s neighboring states. Part
(d) of the residency definition leaves room for physician discretion in
determining residency.
30
As applied by an attending physician, this
discretionary portion could work either in favor of or against patient
access to aid in dying medication. A physician could reasonably find
residency in (d) even when a patient may not be a New Jersey resident.
A patient who is a resident of New Jersey may only have (d)
documentation but be denied legitimate access to the Act because of the
physician’s discretionary determination of residency. While physicians
are always allowed to refuse to participate in aid in dying,
31
patients
without an ID, voter registration, or a most recent tax return might feel
a sense of injustice if their request is denied for lack of such
documentation. Residency seems like it should be a simple checkmark
in the Act’s requirements, but entire court cases can dispute a person’s
residency in one or multiple locations.
32
D. Defining and Applying Time Between Requests
Under the Act, patients and physicians must follow a minimum
timeline for making requests and writing prescriptions.
33
The timeline
requires that:
(1) at least 15 days shall elapse between the initial oral
request and the second oral request; . . .
(3) the patient may submit the written request to the
attending physician when the patient makes the initial oral
request or at any time thereafter; . . .
(5) at least 15 days shall elapse between the patient’s initial
oral request and the writing of a prescription pursuant to
P.L.2019, c.59 (C.26:16-1 et al.); and
(6) at least 48 hours shall elapse between the attending
physician’s receipt of the patient’s written request and the
writing of a prescription . . . .
34
In applying the quickest scenario possible, a patient could submit an oral
and written request on Day One, wait fifteen days, submit a second oral
request on Day Sixteen, and receive a prescription to self-administer the
29
See, e.g., Livio, supra note 4.
30
§ 26:16-11.
31
See § 26:16-3.
32
See generally Sheehan v. Gustafson, 967 F.2d 1214 (8th Cir. 1992).
33
§ 26:16-10.
34
Id.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 851
same day.
35
But if a patient waits until his second oral request on Day
Sixteen to provide a written request, then the attending physician must
wait until at least Day Eighteen to write the prescription.
36
A clear
reading of the Act does not impose a maximum time limit between
patient requests. A qualified terminally ill patient could make an initial
request in January 2021, survive past a six-month prognosis, and make
the second oral request with a written request in January 2022. Under
the Act, the patient has not re-started the aid in dying process.
Additionally, the Act does not set a maximum amount of time between
an attending physician receiving oral and written requests and writing
a prescription for medication.
37
The lack of maximum time between requests will become an issue
when trying to evaluate the efficiency of implementation under the Act.
While attending physicians are required to document all requests,
38
an
attending physician is only required to report the dispensing
medication record and the death record to the Department of Health for
statistical purposes.
39
Therefore, the public data of the Act will only
show two points in the aid in dying process; thus, limiting New Jersey’s
understanding of average time spent considering and completing this
end of life option. If a purpose of the Act is to increase patient choice in
treatment, then New Jersey should understand the length of time a
patient takes to make and implement treatment choices.
III. IMPLEMENTATION AND COMPARISON OF OTHER STATES’ AND COUNTRIES’
AID IN DYING LAWS
In the United States, individual states can enact statutes to create
an ability for physicians and patients to participate in aid in dying, but
states may also explicitly ban any physician-assisted death without
violating the Constitution.
40
Even as applied to competent, terminally ill
adult patients,
41
the federal Constitution does not protect a patient’s
access to aid in dying medication.
42
In Washington v. Glucksberg, the
35
See id.
36
See id.
37
See id.
38
§ 26:16-10(d).
39
N.J. STAT. ANN. § 26:16-13.
40
See Washington v. Glucksberg, 521 U.S. 702, 728, 735 (1997).
41
This is one of four scenarios where a person may wish to accelerate death. The
other three are suicide of a non-terminally ill person or patient, withdrawal of life
support of a terminally ill patient, and physician active euthanasia of a terminally ill
patient. See NOAH R. FELDMAN & KATHLEEN M. SULLIVAN, CONSTITUTIONAL LAW 595 (20th ed.
2019).
42
See Glucksberg, 521 U.S. at 735.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
852 SETON HALL LAW REVIEW [Vol. 51:845
Supreme Court concluded that past precedent allowing patients to deny
unwanted, life-sustaining treatment does not transform into a right to
assisted suicide.
43
Furthermore, it held that the right to personal
autonomy under the Due Process Clause of the federal Constitution does
not extend to every possible personal decision.
44
This Part will compare
the self-administration, residency, and time between request
requirements in New Jersey to those requirements in other states and
countries.
A. Definitional Comparisons of United States Statutes
In Oregon, patients have access to medication to hasten death
through the state’s Death with Dignity Act.
45
In 1994, citizens voted in
the act by a small margin, but then an injunction stalled the process until
1997 when a second vote to keep the legislation resulted in the law’s
enactment.
46
Oregon Health Authority has been collecting data since
that year.
47
Oregon’s act does not provide specific language for a self-
administration requirement.
48
It does, however, require a written
request signed and dated by a qualified patient,
49
which suggests a need
for the patient to have a level of physical strength and control, similarly
required for physical self-administration in New Jersey.
50
The Oregon
Health Authority does clarify that a patient must self-administer and
that a physician may not administer.
51
Oregon’s residency requirement
provides a list of acceptable documentation, such as a driver’s license,
voter registration, and tax return,
52
but leaves discretion, like in New
Jersey’s act, by allowing other documentation. Additionally, the ability
for a person to show he leases property as documentation
53
may allow
for a non-resident to meet this requirement. Oregon required fifteen
days between the first request and a prescription and 48 hours between
43
See id. at 725–26. The Court references its discussion of removing treatment in
Cruzan v. Director, Missouri. Dept. of Health, and of ending life in Vacco v. Quill. Id.
44
See id. at 727–28. The Court references its discussion of right to abortion in
Planned Parenthood of Southeastern Pennsylvania v. Casey. Id.
45
Frequently Asked Questions: Oregon’s Death with Dignity Act, OR. HEALTH AUTHORITY,
https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EVALUATIONRE
SEARCH/DEATHWITHDIGNITYACT/Pages/faqs.aspx (last visited Nov. 1, 2020).
46
Id.
47
See id.
48
OR. REV. STAT. §§ 127.800–127.897 (1994).
49
§ 127.810-2.02.
50
See supra text accompanying note 23.
51
Frequently Asked Questions: Oregon’s Death with Dignity Act, supra note 45.
52
OR. REV. STAT. § 127.860-3.10.
53
Id.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 853
a written request and prescription
54
and, like New Jersey, did not set a
maximum time period between requests. But a change to Oregon law in
2019 allowed Oregon patients to bypass the fifteen-day waiting period
if they are expected to die within the fifteen days.
55
In California, qualified terminally ill patients can request aid in
dying medication through the End of Life Option Act.
56
California’s
history in allowing aid in dying as an end of life option began, in part,
with a patient named Brittany Maynard.
57
At twenty-nine-years-old,
Brittany was diagnosed with a brain tumor but with an otherwise
healthy body and expected a lengthy, painful death.
58
After doing some
research about her treatment options, she chose to use aid in dying
medication, but that option was unavailable in California.
59
Brittany
moved to Oregon, found new doctors, and established residency to
qualify for Oregon’s act.
60
She received the aid in dying medication in
Oregon but kept fighting for a change in California’s law and end of life
options.
61
Under the California act, an aid in dying drug is specifically defined
as a drug an individual can self-administer,
62
and “‘[s]elf-administer’
means a qualified individual’s affirmative, conscious, and physical act of
administering and ingesting the aid-in-dying drug to bring about his or
her own death.”
63
California also explicitly requires that an individual
must have the physical ability to self-administer,
64
and reinforces these
physical requirements by mandating (a) a request form signed and
dated by the patient;
65
and (b) a final attestation form signed, initialed,
and dated by the patient 48 hours before the patient self-administers.
66
Notably, California’s act explicitly prohibits a person who is present at
54
§ 127.850-3.08.
55
The Oregonian/OregonLive Politics Team, New Law Shortens ‘Death with Dignity’
Waiting Period for Some Patients, OREGONIAN (July 24, 2019), https://www.oregon
live.com/politics/2019/07/new-law-shortens-death-with-dignity-waiting-period-for-
some-patients.html.
56
End of Life Option Act, CAL. DEP’T PUB. HEALTH, https://www.cdph.ca.gov/
Programs/CHSI/Pages/End-of-Life-Option-Act-.aspx (last visited Nov. 1, 2020).
57
See Brittany Maynard, COMPASSION & CHOICES, https://compassionandchoices.org/
stories/brittany-maynard (last visited Nov. 1, 2020).
58
Id.
59
See id.
60
Id.
61
See id.
62
CAL. HEALTH & SAFETY CODE § 443.1 (West 2015).
63
Id.
64
§ 443.2.
65
Id.
66
§ 443.5, .11.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
854 SETON HALL LAW REVIEW [Vol. 51:845
the time of death from helping a patient ingest the medication.
67
Overall,
California’s language and requirements surrounding self-
administration are more explicit than those in New Jersey’s act. New
Jersey lacks any language describing how a patient must ingest a
medication and does not specifically reinforce the physical strength
needed near the time of self-administration through a final attestation
form, as California’s act does.
Unlike New Jersey, California does not allow for any unlisted forms
of identification to show residency.
68
California’s requirement does,
however, allow for a patient to demonstrate residency through a leased
property,
69
similar to Oregon’s residency requirement.
70
California’s
requirement of a minimum of fifteen days between requests, but no
maximum number of days,
71
parallels New Jersey’s requirement.
72
California does, however, add a maximum time of 48 hours for a patient
to complete a final attestation form and self-administer the aid in dying
drug.
73
New Jersey’s law contains no similar temporal limitation.
In Washington state, patients can access aid in dying medication
through the Death with Dignity Act.
74
The law was approved by voters
in 2008 after a ballot initiative campaign launched in 2005 with the
support of Oregon funds and advisers; then, it became effective in March
2009.
75
Washington’s act clarifies that self-administration must be
through an act of ingesting medication.
76
In Washington, a qualified
patient must sign and date a written request;
77
this suggests the same
level of physical strength and ability to self-administer under the New
Jersey act, which does not explicitly say that a patient must ingest aid in
dying medication. Washington’s residency requirement allows for
unlisted documentation outside the options and allows for a patient to
show leased property as evidence of residency.
78
These broad options
allow for more residency options than the acts in New Jersey, Oregon,
67
CAL. HEALTH & SAFETY CODE § 443.14.
68
§ 443.2.
69
Id.
70
OR. REV. STAT. § 127.860-3.10.
71
CAL. HEALTH & SAFETY CODE § 443.3.
72
N.J. STAT. ANN. § 26:16-10.
73
CAL. HEALTH & SAFETY CODE § 443.5.
74
Death with Dignity Act, WASH. ST. DEP’T HEALTH, https://www.doh.wa.gov/Youand
YourFamily/IllnessandDisease/DeathwithDignityAct (last visited Oct. 31, 2019).
75
Washington, DEATH WITH DIGNITY, https://www.deathwithdignity.org/states/
washington (last visited Sept. 18, 2019).
76
WASH. REV. CODE § 70.245.010 (2008).
77
§ 70.245.090.
78
§ 70.245.130. Options to show residency include a state driver’s license, voter
registration, and owning or leasing property in the state. Id.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 855
and California. The fifteen days required between oral requests and 48
hours required from a physician receiving a written request and writing
a prescription
79
match New Jersey’s time between requests
requirements.
80
In Colorado, terminally ill patients can access aid in dying
medication pursuant to Colorado’s End-of-Life Options Act,
81
which
voters approved in 2016.
82
Colorado requires a qualified patient to
make an informed decision to self-administer.
83
“‘Self-administer’
means a qualified individual’s affirmative, conscious, and physical act of
administering the medical aid in dying medication to himself or herself
to bring about his or her own death.”
84
This language is similar to the
California law but, like New Jersey’s statute, it fails to explicitly require
that a patient ingest the medication. Colorado also requires a patient to
sign and date a written request,
85
which, like New Jersey’s requirement,
reinforces the requirement of the patient’s physical ability to self-
administer. Unlike New Jersey, Colorado only allows for the listed
documentation options to prove residency, but one of these options
includes showing a leased property in the state.
86
Colorado requires
fifteen days between oral requests
87
but, unlike New Jersey, does not
add an additional forty-eight-hour waiting period between the patient
making the written request and the physician writing the prescription.
Patients in Maine recently gained access to aid in dying with
Maine’s Death with Dignity Act.
88
The state legislature voted in the act
in Spring 2019, and Governor Janet Mills signed it into law in June
2019.
89
In Maine, a qualified patient may self-administer by “voluntarily
ingest[ing] medication to end the qualified patient’s life in a humane and
dignified manner.”
90
This language differs from New Jersey’s approach
by specifically requiring a patient to ingest the medication. Like New
Jersey and other states, the Maine act requires the patient to have the
79
§ 70.245.090, .110.
80
N.J. STAT. ANN. § 26:16-10.
81
Medical Aid in Dying, COLO. DEP’T OF PUB. HEALTH & ENV’T, https://www.colorado.
gov/pacific/cdphe/medical-aid-dying (last visited Oct. 31, 2019).
82
Id.
83
COLO. REV. STAT. § 25-48-102 (2016).
84
Id.
85
§ 25-48-104; see also § 25-48-112.
86
§ 25-48-102.
87
§ 25-48-104.
88
Paula Span, Aid in Dying Soon Will Be Available to More Americans. Few Will Choose
It., N.Y. TIMES (July 8, 2019), https://www.nytimes.com/2019/07/08/health/aid-in-
dying-states.html.
89
Id.
90
ME. REV. STAT. ANN. tit. 418, § 2140(2)(L) (2019).

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
856 SETON HALL LAW REVIEW [Vol. 51:845
physical capacity to sign and date a written form.
91
Maine’s residency
requirement offers the longest list of options for documentation of
residency and gives the most detail in what the documentation can and
cannot show.
92
The residence of a person is that place where the person has
established a fixed and principal home to which the person,
whenever temporarily absent, intends to return. The following
factors may be offered in determining a person’s residence
under this Act and need not all be present in order to
determine a person’s residence: A. Possession of a valid
driver’s license issued by the Department of the Secretary of
State, Bureau of Motor Vehicles; B. Registration to vote in this
State; C. Evidence that the person owns or leases property in
this State; D. The location of any dwelling currently occupied
by the person; E. The place where any motor vehicle owned
by the person is registered; F. The residence address, not a
post office box, shown on a current income tax return; G. The
residence address, not a post office box, at which the person’s
mail is received; H. The residence address, not a post office box,
shown on any current resident hunting or fishing licenses held
by the person; I. The residence address, not a post office box,
shown on any driver’s license held by the person; J. The receipt
of any public benefit conditioned upon residency, defined
substantially as provided in this subsection; or K. Any other
objective facts tending to indicate a person’s place of
residence.
93
Unlike other states, Maine’s other evidence option relies more on
objective facts of residency than other forms of identification.
Additionally, the “need not all be present” phrase can prompt physicians
to consider multiple forms of identification, which other states,
including New Jersey, have failed to recommend.
94
While Maine’s
residency requirements are unique, its waiting period requirements for
a minimum of fifteen days between oral requests
95
and 48 hours from a
patient writing a request and the physician writing a prescription
96
parallel the requirements in New Jersey and the majority of the states
discussed infra.
91
§ 2140(5).
92
§ 2140(15).
93
Id. (emphasis added).
94
N.J. STAT. ANN. § 26:16-11.
95
ME. REV. STAT. ANN. tit. § 2140(11) (2019).
96
§ 2140(13).

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 857
B. Aid in Dying Around the World: A Comparison of New Jersey and
United States Requirements with International Requirements
In Belgium, competent adults and emancipated minors gained
access to hasten their death pursuant to The Belgian Act on Euthanasia
on May 28, 2002.
97
These persons must be patients “in a medically futile
condition of constant and unbearable physical or mental suffering that
can not [sic] be alleviated, resulting from a serious and incurable
disorder caused by illness or accident.”
98
In 2014, Belgium removed its
previous age limit; thus, the country radically extended its law to allow
children of any age to request the lethal injection as long as the parents
give consent.
99
Since then, physicians have euthanized seventeen-,
eleven-, and nine-year-old patients.
100
Rather than requiring patients to
self-administer, Belgium allows euthanasia, which it defines as a
physician—not the patient—terminating the patient’s life.
101
The default requirements under Belgian law do assume some level
of patient physical strength and ability. Similar to New Jersey and other
United States acts, Belgium’s act requires a patient to write and sign a
request.
102
Unlike in New Jersey and the United States, however,
Belgium provides an exception where a patient may designate a person
to write and sign the request if the person lists why the patient is
incapable of independently writing a request.
103
Therefore, Belgium
does not necessarily restrict patients who are physically disabled from
their illness or a previous condition from access to euthanasia, whereas
New Jersey and other states restrict these patients from access to aid in
dying options.
Additionally, Belgium’s act does not contain residency
requirements.
104
Further, Belgium’s equivalent of the time between
requests requirements offers more discretion than New Jersey or other
97
Belgium, PATIENTS RTS. COUNCIL, http://www.patientsrightscouncil.org/site/
belgium (last visited Sept. 19, 2019).
98
§ 1 [The Belgian Act on Euthanasia] of May 28, 2002, 10 EUR. J. HEALTH L. 329
(2003).
99
Belgium, PATIENTS RTS. COUNCIL, http://www.patientsrightscouncil.org/site/
belgium (last visited Nov. 13, 2020). Note that while technically the child makes the
decision, it is easy to imagine the technical lines blurring between a child making a
decision and a parent making a decision but a child expressing it as her own.
100
Dale Hurd, The ‘Default Way to Die’: Are Dutch and Belgian Doctors Euthanizing
People Who Don’t Want to Die?, CHRISTIAN BROADCASTING NETWORK (Aug. 28, 2019),
https://www1.cbn.com/cbnnews/world/2019/april/euthanasia-becoming-default-
way-to-die-in-belgium.
101
§ 1 [The Belgian Act on Euthanasia] of May 28, 2002.
102
§ 3(4) (Belg.).
103
Id.
104
See [The Belgian Act on Euthanasia] of May 28, 2002.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
858 SETON HALL LAW REVIEW [Vol. 51:845
United States laws. The act requires physicians to engage in “several”
conversations with the patient about the patient’s request and physical
and mental suffering over a “reasonable period of time.”
105
Belgium’s
act is clear, however, in requiring at least one month between the
written request and euthanasia if the “physician believes patient is
clearly not expected to die in the near future.”
106
One month between a
written request and death is longer than New Jersey’s 48 hours,
107
but
the above language leaves the physician some discretion and an ability
to euthanize even before 48 hours have elapsed.
Even though Belgium does not require a maximum time between
requests and death, Belgium does cap advance directives for euthanasia;
still, people who may not be mentally competent at the time of
administration may access Belgium’s act.
108
If the patient’s euthanasia
request comes as an advance directive, the directive will only be valid if
it was drafted in the last “five years prior to the person’s loss of the
ability to express his/her wishes.”
109
In 2019, developments to Canada’s aid in dying law offered some
compelling justifications for why a state or country should allow
advance directives for medically assisted dying.
110
Members of Canada’s
legislative body recognize that Alzheimer’s patients are in a unique
position: when they are first diagnosed, they may be able to consent to
medical assistance in dying, but they are not at the required “end of
life.”
111
But, when an Alzheimer’s patient is near the end of life, they
have lost their ability to make a decision about medical assistance in
dying.
112
This legislative debate follows the Lamb case, where the court
expanded what it means for a patient’s death to be “reasonably
105
§ 3(2) (Belg.).
106
§ 3(3) (Belg.).
107
N.J. STAT. ANN. § 26:16-10.
108
§ 4(1) (Belg.). “[A]n advance directive, a legal document that goes into effect only
if you are incapacitated and unable to speak for yourself. This could be the result of
disease or severe injury—no matter how old you are. It helps others know what type of
medical care you want.” NAT’L INST. ON AGING, Advance Care Planning: Healthcare
Directives, U.S. DEP’T HEALTH & HUM. SERVS., https://www.nia.nih.gov/health/advance-
care-planning-healthcare-directives#after (last visited Jan. 9, 2020).
109
§ 4(1) (Belg.).
110
See Quebec to Expand Law on Medically Assisted Dying, Look at Advance Consent,
CBC NEWS (Nov. 29, 2019 9:34 AM), https://www.cbc.ca/news/canada/montreal/
medical-assistance-in-death-report-1.5377890.
111
See id.
112
See id. See infra pp. 870–72, for an explanation of why New Jersey should not use
advance directives for aid in dying.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 859
foreseeable.”
113
The Supreme Court ruled against the current legislative
members’ understandings of “reasonably foreseeable” and in favor of a
patient-centered definition where “patients can meet the ‘reasonably
foreseeable’ criterion if they have demonstrated a clear intent to take
steps to make their natural death happen soon or to cause their death to
be predictable.”
114
The case could expand the current understanding of
the legislation to allow for advance directives, which may not require
informed consent at the time of request and the time of either
euthanasia or self-administration.
115
An advance directive could mean
the patient has lost his capacity to make informed consent by the time
he is requesting or receiving aid in dying treatment. Canada already
allowed patients with dementia, who still understand the requests they
are making, to be capable of the required informed consent.
116
Since 2002, doctors in the Netherlands have been legally allowed
to perform euthanasia on patients or assist in their suicides, even if the
patients do not have a terminal illness.
117
By 2015, 4.5% of deaths in the
Netherlands were caused by acts of euthanasia, with non-terminally ill
patients being a small portion of that percentage.
118
In 2018,
committees reviewed cases of euthanasia to compile resources and
guidance for physicians in the Euthanasia Code 2018.
119
In addition to
the lack of minimum or maximum time required between requests and
death,
120
the Netherlands act is not concerned with a specific prognosis.
It only requires that a patient’s suffering be “lasting and unbearable.”
121
113
Jocelyn Downie, A Watershed Month for Medical Assistance in Dying, POL’Y OPTIONS
POLITIQUES (Sept. 20, 2019), https://policyoptions.irpp.org/magazines/september-
2019/a-watershed-month-for-medical-assistance-in-dying.
114
See id.
115
See Medical Assistance in Dying, GOV’T OF CAN., https://www.canada.ca/en/health-
canada/services/medical-assistance-dying.html (last visited Feb. 14, 2020).
116
See, e.g., The Sunday Edition, B.C. Man Is One of the First Canadians With Dementia
to Die with Medical Assistance, CBC RADIO (Oct. 27, 2019), https://www.cbc.ca/radio/
thesundayedition/the-sunday-edition-for-october-27-2019-1.5335017/b-c-man-is-
one-of-the-first-canadians-with-dementia-to-die-with-medical-assistance-1.5335025.
117
The Associated Press, Euthanasia Deaths Becoming Common in Netherlands, CBS
NEWS (Aug. 3, 2017), https://www.cbsnews.com/news/euthanasia-assisted-suicide-
deaths-netherlands.
118
Id.
119
Euthanasia Code 2018, REGIONAL EUTHANASIA REV. COMM. (Jan. 10, 2019),
https://english.euthanasiecommissie.nl/the-committees/documents/publications/
euthanasia-code/euthanasia-code-2018/euthanasia-code-2018/euthanasia-code-
2018.
120
Termination of Life on Request and Assisted Suicide (Review Procedures) Act
2001, 137. Art. 2(1)e (Neth.), https://www.worldrtd.net/dutch-law-termination-life-
request-and-assisted-suicide-complete-text.
121
See id. at Art. 2(1)b (Neth.).

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
860 SETON HALL LAW REVIEW [Vol. 51:845
Netherlands’ act does not contain language requiring a patient to
administer his own medication. Rather, in the Netherlands, doctors can
give a lethal injection to a person with unbearable suffering and no
reasonable alternative.
122
In its first criminal investigation of
euthanasia, the Netherlands court cleared a doctor of any criminal
charges for administering a sedative and lethal injection to a dementia
patient who exhibited mixed signals about wanting to die.
123
The
patient in this case, and like many other reported cases in the
Netherlands, had an advanced directive for euthanasia, and the doctor
had to perform that directive with due care.
124
At first glance, this case seems like the result of the “slippery slope”
people might be wary of and that United States laws want to protect
against by allowing only patients to self-administer their prescribed aid
in dying medications. But the doctor or the patient administering is not
the only distinction in this case. Even if states allowed for physician
administration, patients and health care professionals would not face
the issues seen in the Netherlands case. In that case, the patient had an
advance directive for euthanasia, like the law in Belgium allows and
possible changes to the law in Canada would allow;
125
no United States
statute, however, allows advance directives for aid in dying medication.
The Netherlands patient was not able to change her mind at the time of
administration, and the doctor ignored her mixed signals because of her
dementia.
126
A New Jersey case would never reach this point—even if
physicians could administer or prepare injections—because New Jersey
further requires the qualified patient to be capable and “hav[e] the
capacity to make health care decisions and to communicate them to a
health care provider, including communication through persons
familiar with the patient’s manner of communicating if those persons
are available.”
127
Given the symptoms of dementia,
128
it does not seem
122
Palko Karasz, Dutch Court Clears Doctor in Euthanasia of Dementia Patient, N.Y.
TIMES (Sept. 11, 2019), https://www.nytimes.com/2019/09/11/world/europe/
netherlands-euthanasia-doctor.html. For more recent examples of Dutch courts
allowing physicians to euthanize patients with dementia, see Another Netherlands Court
Approves Euthanasia by Advance Directive, MED. FUTILITY BLOG (Sept. 14, 2020),
http://www.bioethics.net/2020/09/another-netherlands-court-approves-euthanasia-
by-advance-directive.
123
See Karasz, supra note 122.
124
See id.
125
See supra pp. 857–59.
126
See Karasz, supra note 122.
127
N.J. STAT. ANN. § 26:16-3.
128
“Dementia is the loss of cognitive functioning—thinking, remembering, and
reasoning—and behavioral abilities to such an extent that it interferes with a person’s
daily life and activities. These functions include memory, language skills, visual

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 861
like many qualified terminally ill patients with dementia would be
deemed capable to make this health care decision.
129
Even if a physician
found an otherwise qualified terminally ill patient with early-stage
dementia capable under the New Jersey act, the patient would not have
the ability to make an advance directive for when the dementia
progresses and would always have the ability to rescind a request
regardless of his patient’s previous wishes.
130
New Jersey’s lack of a
maximum time between requests would allow the patient to complete
the request process very early in the stages of dementia, then, wait to
take the medication.
In Western Australia, patients gained access to aid in dying with the
Voluntary Assisted Dying Bill.
131
As the Victorian Voluntary Assisted
Dying Act 2017 became effective in June 2019, another Australian state,
Western Australia, was developing legislation in its parliament for its
own Voluntary Assisted Dying Act.
132
As Western Australia continued
developing legislation, an Australian woman became the first to use
Victoria’s new law.
133
After a twenty-six-day approvals process,
terminal cancer patient Kerry Robertson died at a nursing home.
134
Of all these international sources, Western Australia’s
requirements and safeguards for administration of medication,
residency, and timing of requests most closely parallel those used across
the United States, so New Jersey could implement some of Western
Australia’s safeguards. Furthermore, Western Australia’s act allows
United States health departments to draw more exact international
comparisons about aid in dying and consider cross-cultural
explanations for differences in trends. It is more challenging to compare
numbers across countries’ sets of data when the countries allow
perception, problem solving, self-management, and the ability to focus and pay
attention.” Nat’l Inst. of Aging, What Is Dementia? Symptoms, Types, and Diagnosis, U.S.
DEP’T HEALTH & HUM. SERVS., https://www.nia.nih.gov/health/what-dementia-
symptoms-types-and-diagnosis (last visited Jan. 9, 2020).
129
But see The Sunday Edition, supra note 116.
130
N.J. STAT. ANN. § 26:16-6(8).
131
See Voluntary Assisted Dying Bill 2019 (WA) (Austl.), https://www.parliament.wa.
gov.au/Parliament/Bills.nsf/502E87F2E1B94E27482584A3003A757C/$File/Bill139-
2.pdf; see also Voluntary Assisted Dying Bill 2019, PARLIAMENT W. AUSTL.,
https://www.parliament.wa.gov.au/parliament/bills.nsf/BillProgressPopup?openFor
m&ParentUNID=502E87F2E1B94E27482584A3003A757C (last visited Jan. 10, 2020).
132
Bregje Onwuteaka-Philipsen, Lindy Willmot & Ben P. White, Regulating Voluntary
Assisted Dying in Australia: Some Insights from the Netherlands, MED. J. AUSTL. (Sept. 9,
2019), https://www.mja.com.au/journal/2019/211/10/regulating-voluntary-
assisted-dying-australia-some-insights-netherlands#4.
133
Assisted Dying: Australian Cancer Patient First to Use New Law, BBC NEWS (Aug. 5,
2019), https://www.bbc.com/news/world-australia-49230903.
134
Id.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
862 SETON HALL LAW REVIEW [Vol. 51:845
patients of different ages and categories, such as minors or non-
terminally ill patients, to access aid in dying options.
135
Even though the Western Australian bill was modeled after the
Victorian act, it differs in its definition of acceptable administration
methods.
136
In Western Australia, self-administration is the default
option for a patient receiving medication.
137
A patient with a six-month
prognosis
138
can make the decision to have her physician administer the
substance if the physician has certain qualifications to be an
administering practitioner, including specific training.
139
A patient may
choose to self-administer or to have the practitioner administer the
medication.
140
Patients have an equal ability to choose between
practitioner administration or self-administration, but the provision
requires that practitioner administration should only be used when it
would be impossible or inappropriate for a patient to self-administer.
141
This language strikes a balance between (a) an emphasis on patients
taking their own voluntary assisted death actions and (b) a conscious
inclusion of patients who may lack physical ability but who are identical
to other patients in every other requirement. The signed, written
declaration requirement
142
suggests that patients using the law must
have the physical ability to self-administer, as New Jersey’s act requires.
But, as Belgium’s act requires,
143
an Australian patient who is unable to
sign the declaration can have another person sign the declaration on her
135
In other words, current cross-cultural comparisons are limited because of the
certain requirements in other countries. For example, if data trends showed patients in
Belgium spending five years between request and administration and New Jersey
patients show an average of six months between request and administration, it would
be hard to infer that this has something to do with the culture of healthcare in either
country because Belgium, unlike New Jersey, does not require a six-month prognosis but
does allow advance directives. A data analyst trying to infer cultural differences
between any/all U.S. states and Western Australia could be more confident in that
comparison because the similarities between the laws means eliminating differing
requirements that would otherwise be intervening variables.
136
Frances Bell, Voluntary Euthanasia Bill to Be Introduced into West Australian
Parliament, ABC NEWS (Aug. 6, 2019), https://www.abc.net.au/news/2019-08-06/
voluntary-assisted-dying-bill-introduced-to-wa-parliament/11386512.
137
Voluntary Assisted Dying Bill 2019 (WA) pt 4 div 2 s 56 (Austl.),
https://www.parliament.wa.gov.au/Parliament/Bills.nsf/502E87F2E1B94E27482584
A3003A757C/$File/Bill139-2.pdf.
138
Id. pt 2 s 16. But a twelve-month prognosis is required for neurodegenerative
illness. Id.
139
Id. pt 4 div 1 ss 54–55.
140
Id. s 56.
141
See id.
142
Voluntary Assisted Dying Bill 2019 (WA) pt 3 div 5 s 42.
143
§ 3(4) [The Belgian Act on Euthanasia] of May 28, 2002.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 863
behalf.
144
The default option encourages a patient’s physical ability to
self-administer, but the exception allows a patient with a physical
disability from a previous condition or the terminal illness to still access
voluntary assisted dying. Physically disabled patients in New Jersey and
across the United States, however, are not granted these exceptions for
providing written documentation or for self-administration.
Western Australia’s residency requirement is based on objective
facts about residency in the prior year, rather than specific
documentation.
145
The most notable part of this requirement is the
specific ability of a patient to appeal to the Western Australian residency
decision from either the coordinating or consulting physician to a
tribunal.
146
New Jersey does not specifically allow for this type of
external, non-medical professional appeals process. Western Australia
only requires nine days between the first and final request for voluntary
assisted dying
147
and allows for an exception to the minimum nine days
if, among other requirements, the coordinating physician believes “the
patient is likely to die, or to lose decision-making capacity in relation to
voluntary assisted dying, before the end of the designated period.”
148
While New Jersey does not currently allow for physicians and patients
to hasten this process, future amendments should mirror the exceptions
in the Western Australian act and the amended Oregon act.
149
IV. STATISTICAL COMPARISON OF NEW JERSEY AND OTHER STATES AND
COUNTRIES
This Part reviews aid in dying data from other states and countries
discussed in this Comment, compares it with United States census data,
and makes predictions about how providers and patients could use New
Jersey’s act. This Part also considers data-reporting concerns similar to
those in other states and concerns unique to New Jersey.
144
Id.
145
See id. pt 2 s 16.
146
Id. pt. 5 sec. 84.
147
Id. pt. 3 div. 6 sec. 47.
148
Id. pt. 3 div. 6 sec. 47.
149
See OregonLive Politics Team, supra note 55.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
864 SETON HALL LAW REVIEW [Vol. 51:845
A. Reported and Expected Deaths from Aid in Dying Medications
150
In Oregon’s data from 2017 through 2018, physicians wrote 467
prescriptions for aid in dying medication, and within the two years, 311
people died from ingesting the prescribed medication.
151
United States
census data for July 2017 through July 2018 revealed that 36,052 people
died in Oregon that year,
152
suggesting that 0.86% of deaths in Oregon
could have resulted from aid in dying medication.
California’s 2017–2018 data showed that physicians wrote 1,029
prescriptions for aid in dying medication, and within that period, 711
people died from the medication.
153
Census data for July 2017 to July
2018 revealed that 280,674 people died in the state that year,
154
suggesting that 0.25% of deaths in California could have resulted from
aid in dying medication.
Washington’s 2017–2018 data shows that physicians wrote 479
prescriptions for aid in dying medication, and within the two years, 367
people died from the medication.
155
Census data for July 2017 to July
150
See infra App’x. at 874. Note the lack of data for two other continental states that
allow physician-assisted dying. Montana’s Supreme Court ruled that Montana’s laws
allow for physicians to provide medication to hasten patient death; thus, the state has
not created an aid in dying statute with a reporting requirement and has not made data
readily available. See Baxter v. State, 224 P.3d 1211, 1222 (Mont. 2009); see also
Montana, DEATH WITH DIGNITY, https://www.deathwithdignity.org/states/montana (last
visited Jan. 5, 2020). Vermont’s statute requires physicians to report writing
prescriptions and death by aid in dying medication, but the state is only required to
report every other year. See Report Concerning Patient Choice at End of Life, VT. DEP’T
HEALTH (Jan. 15, 2018), https://www.healthvermont.gov/systems/end-of-life-
decisions/patient-choice-and-control-end-life. The initial and most recent report
included years 2013–2017, so Vermont’s available data is not comparable to the other
states’ 2017–2018 data. See id.
151
Death with Dignity Act Annual Reports, OR. HEALTH AUTHORITY,
https://www.oregon.gov/oha/ph/providerpartnerresources/evaluationresearch/dea
thwithdignityact/pages/ar-index.aspx (Year 2018) (last visited Sept. 20, 2019).
152
2018 National State and Population Estimates: Table 5. Estimates of the
Components of Resident Population Change for the United States, Regions, States, and
Puerto Rico: July 1, 2017 to July 1, 2018, U.S. CENSUS BUREAU, https://www.census.gov/
newsroom/press-kits/2018/pop-estimates-national-state.html (last visited Sept. 20,
2019) [hereinafter 2018 National State and Population Estimates]. Note that available
census data to track vital life events are measured from July 2017 through July 2018,
while the states produce annual aid in dying reports on the calendar year. Id. This
means, for example, a death in Colorado in June 2017 would be reflected in Colorado’s
data, but not in the census for July 2017–July 2018.
153
End of Life Option Act 2018 Data Report, CAL. DEP’T PUB. HEALTH, at 3,
https://www.cdph.ca.gov/Programs/CHSI/Pages/End-of-Life-Option-Act-.aspx (last
visited Sept. 20, 2019). Note that the two most common prescriptions were for
sedatives and “a combination of a cardiotonic, opioid, and sedative.” Id. at 3.
154
See 2018 National State and Population Estimates, supra note 152.
155
2018 Death with Dignity Act Report, WASH. ST. DEP’T HEALTH, at 1,
https://www.doh.wa.gov/Portals/1/Documents/Pubs/422-109-DeathWithDignityAct

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 865
2018 revealed that 57,568 people died in the state that year,
156
suggesting that 0.25% of deaths in Washington could have resulted from
aid in dying medication.
In its first two years of implementing its act, Colorado collected
data showing that physicians wrote 197 prescriptions for aid in dying
medication and that between 2017 and 2018, 174 people died from
ingestion.
157
Census data for July 2017 to July 2018 revealed that 38,367
people died in the state that year,
158
suggesting that 0.45% of deaths in
Colorado could have resulted from aid in dying medication.
B. Data-Reporting Concerns and Predictions
The lack of a maximum time between requests contributes to a
data-reporting issue. Current reports do not measure the time a patient
spends in the initial stages of the aid in dying process.
159
A future
evaluation of the efficacy of the Act would benefit from understanding
how long patients take to complete a decision. The prescription-to-
administration-and-death timeline is only measured by the calendar
year in current reports.
160
The states’ data referenced above measures
when a patient received a prescription in one year but ingested the
medication in another year,
161
but the reports cannot show whether
these dates happen quickly between December and January of two
calendar years or if patients tend to hold medication for many months
or even a full year before self-administering. New Jersey’s future data,
if it only follows its current reporting requirements,
162
will also fail to
measure these points and track these issues.
2018.pdf (last visited Sept. 20, 2019); 2017 Death with Dignity Act Report, WASH. ST. DEP’T
HEALTH, at 1, https://www.doh.wa.gov/Portals/1/Documents/Pubs/422-109-Death
WithDignityAct2017.pdf (last visited Sept. 20, 2019).
156
See 2018 National State and Population Estimates, supra note 152.
157
Colorado End-of-Life Options Act, Year Two 2018 Data Summary, with Updates to
2017 Data, COLO. DEP’T PUB. HEALTH & ENV’T, at 2, https://drive.google.com/file/d/
1FmoyCcL2gHopDO9rCJ2lGFEMUye8FQei/view (last visited Sept. 20, 2019). Some
individual state data, such as Colorado’s data, indicates the patient’s terminal illness. See
id. Looking at this available data and discussing the physical symptoms of different
illnesses might provide insight on the different capabilities of patients to self-
administer.
158
See 2018 National State and Population Estimates, supra note 152.
159
See sources cited supra notes 151–157.
160
See sources cited supra notes 151–157.
161
See sources cited supra notes 151–157.
162
The New Jersey statute includes the following reporting requirements:
(1) No later than 30 days after the dispensing of medication pursuant
to P.L.2019, c.59 (C.26:16-1 et al.), the physician or pharmacist who
dispensed the medication shall file a copy of the dispensing record
with the department, and shall otherwise facilitate the collection of

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
866 SETON HALL LAW REVIEW [Vol. 51:845
Despite these omissions of potentially useful data, this Comment
purports to make predictive calculations for New Jersey’s use of aid in
dying. These predictions are simply rough calculations to raise
potential concerns, address typical questions around aid in dying, and
encourage facilities and physicians to further prepare for the Act in New
Jersey. The average of the above states’ percentages of death from
ingesting prescribed medication is approximately 0.55% of state deaths.
The average lies closest to Colorado’s 0.45%, which reflects a
percentage of deaths in a state that has only had an aid in dying option
for a few years. By taking the 0.55% average and multiplying by the
number of Maine deaths from July 2017 to July 2018 (14,079 deaths),
163
we can predict 77 deaths in Maine from ingesting prescribed
medication. By multiplying the same 0.55% average by New Jersey’s
total deaths from July 2017 to July 2018 (76,370),
164
we can estimate
about 420 deaths within two years.
165
The average number of prescriptions within the past two years in
Oregon, California, Washington, and Colorado is 543 prescriptions. The
average of the confirmed deaths from ingesting prescribed medication
is 390.75 deaths. Comparing the 543 prescriptions to the 390.75 deaths,
there is an average proportion of 1.4 aid in dying prescriptions per
death from ingesting the medication. Applying this proportion to Maine
suggests 107.8 prescriptions within two years. Applying it to New
Jersey suggests 588 prescriptions within two years. These predictions
would be even higher than the values for the past two years in
Oregon,
166
a state that has had its act in place for decades.
such information as the director may require regarding compliance
with P.L.2019, c.59 (C.26:16-1 et al.).
(2) No later than 30 days after the date of the qualified terminally ill
patient’s death, the attending physician shall transmit to the
department such documentation of the patient’s death as the director
shall require.
N.J. STAT. ANN. § 26:16-13.
163
See 2018 National State and Population Estimates, supra note 152.
164
See id.
165
On July 31, 2020, approximately a year after enactment, New Jersey’s Department
of Health released its first annual report. Annual Report Chronicles Impact of New Jersey’s
Death with Dignity Law, N.J. DEP’T OF HEALTH (July 31, 2020) [hereinafter Annual Report],
https://www.nj.gov/health/news/2020/approved/20200731b.shtml. While only
twelve reported deaths, the state only released from between August 1, 2019 and
December 31, 2019. Id. The release offers no explanation for the lack of reports between
January 1, 2020 and July 30, 2020. Id.
166
See supra note 151 and accompanying text.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 867
These numbers do not, however, support any slippery slope
argument about people choosing to end their lives in New Jersey more
than in other states.
167
Furthermore, these elementary predictions are
simply meant to alert physicians and facilities that, insofar as New
Jersey is similar to other states and has a similar statute, patients may
use the Act similarly. At an estimated 588 prescriptions per
approximately two years, participating physicians across the state could
be writing approximately one prescription every other day. This
potential level of use supports the concerns in the discussion below
about considerations for changing residency and implementation to
avoid errors in physician discretion and use of the Act. These statutes
are as much about patient choice as they are about compliance and the
ability to report compliance with the definitions discussed above.
C. New Jersey Residency
While not explicitly stated in New Jersey’s act, it is important to
consider how New Jersey patients, physicians, and caretakers might lose
protection under the Act if a patient self-administers in another state.
168
This is an especially important consideration for people who qualify as
New Jersey residents because other states—New York and
Pennsylvania, namely—are in such close proximity but do not offer any
protections for medical aid in dying. Depending upon physical ability
and the type of illness, any transportation at the ultimate stage of an
illness may become impossible, but the self-administration and writing
requirements
169
in New Jersey do require some level of physical
strength that might make traveling with a terminal illness more
probable. While not the focus of this Comment, it is important to
mention that a patient’s ability to move and take a drug elsewhere
would create inaccuracies in how many people died in any given year in
a state from self-administering medication and could distort results in
reporting data as required by many of these statutes.
167
New Jersey just has more people, and more people could lead to a higher
number—but there is no need for concern. As a potential counter to any slippery slope
concerns about New Jersey’s trends: if New Jersey followed the Netherlands trend of
4.5% of deaths from euthanasia, it would be estimating about 3,437 deaths, a number
more than eight times greater than the 420 deaths predicted based off of United States
trends. In fact, in the first six months, New Jersey only recorded twelve deaths. See
Annual Report, supra note 165.
168
“If you take a dose prescribed under a death with dignity law outside the state
where you obtained it, you may lose the legal protections afforded by the law in
question. For example, your death may be ruled a suicide under another state’s law, with
resulting effects on your insurance policies.” Frequently Asked Questions, DEATH WITH
DIGNITY, https://www.deathwithdignity.org/faqs (last visited Sept. 18, 2019).
169
See discussion supra Section II.B.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
868 SETON HALL LAW REVIEW [Vol. 51:845
V. RECOMMENDATIONS FOR NEW JERSEY
This Part will recommend best practices for New Jersey facilities,
including private practices or hospitals, under the current Act. Then, it
will offer some recommendations for amendments to the Act.
A. Implementation and Best Practices Under the Current Act
New Jersey facilities have to be careful not to unfairly limit a
patient’s ability to access the Act, but they can implement the internal
safeguards below without changing the procedures outlined in the Act.
Facilities have an interest in protecting their physicians and treating
their patients with respect, whether or not their physicians are willing
and able to aid in a patient’s death under the Act.
1. Provide Training for Self-administration
Similar to how Western Australia requires all physicians to learn
how to administer,
170
New Jersey facilities or medical and hospital
associations could provide training that teaches physicians how to teach
patients to self-administer properly. By enabling physicians to show
patients and families how to properly self-administer, New Jersey might
increase access to the Act for patients with certain physical disabilities
who may think they are incapable of using the Act. This training could
also show physicians how to teach caretakers to prepare drugs for a
patient’s self-administration. If New Jersey wants to follow other states
in requiring that the drugs be ingested rather than self-injected, the
training would have to differentiate between those two forms of
administration. This would help enforce that patients should be
ingesting medication, without explicitly changing the language of the
Act. Below, this Comment discusses the possibility of clarifying the Act
to include both forms of administration explicitly, therefore, expanding
the training possibilities. Lastly, providing physician training could
become a method for facilities and patients to determine which
physicians may be willing and able to participate in the aid in dying
process.
2. Documentation of Residency
Facilities should consider providing an internal system that allows
physicians to confirm a patient’s residency with a central residency
point-person. Similar to the tribunal appeal system required in Western
Australia, under the proposed system, a patient could ask for
reconsideration of a residency decision. Before the initial decision or at
170
See supra note 139 and accompanying text.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 869
the time of reconsideration, a physician and patient could refer to a
point-person in a facility’s legal department or a resource at a state-wide
medical or hospital association. While New Jersey’s act explicitly states
that the physician has discretion to accept another government
document as confirmation of residency,
171
there is nothing in the Act to
prevent a physician from consulting with other professionals about
whether the patient meets the residency requirement. The point-
person could have a list of other documents, such as a lease in the state,
or an understanding of a patient’s permanency or intent to return
(similar to Maine’s residency requirements)
172
to help a physician
consider a patient’s residency. The point-person could thoroughly
consider what, if any, properties, licenses, or leases a patient has in other
states that may determine whether a patient intends to stay in New
Jersey or return to another state or country.
A system for confirming residency would address some current
implementation issues that result from requiring medical professionals
to make determinations of residency. Such a system would protect
physicians from falsely identifying a patient as a resident through any of
the documentation. The system would also protect patients by making
sure that they are not prohibited from using the Act simply because one
physician did not determine residency under New Jersey’s requirement.
While there may be instances where a physician determines that a
person, such as an undocumented person, has enough “other
documentation” to show residency, but the point-person disagrees,
there could also be the inverse scenario where a physician does not find
enough documentation, but the point-person does and increases access
to the Act.
Facilities should additionally consider including residency
documentation within their data collection. Without including the
patient’s actual residency information, a facility could keep a record of
which type of documentation was provided to determine residency and
whether the facility found the patient to be a resident. If a facility,
through internal documents or state reports, finds that the unlisted
options available are being used frequently, this may be a warning that
non-New Jersey residents are crossing local state borders to access the
Act.
171
N.J. STAT. ANN. § 26:16-11.
172
ME. REV. STAT. ANN. tit. 418, § 2140(15) (2019).

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
870 SETON HALL LAW REVIEW [Vol. 51:845
3. Limiting Time Between Requests
New Jersey only requires a minimum waiting period between
requests. Patients can wait more than fifteen days to make a second
request and can wait after two oral requests to make a written
request;
173
the law does not, however, prevent a physician from
continually clarifying that a patient is voluntarily requesting the
medication. Unlike other statutes, New Jersey physicians do not need to
prepare final request forms under the Act. Facilities could require
professionals participating in the Act to use similar forms to indicate the
physician’s own opinion at the time of prescription, even if an initial
determination of eligibility was made months or years earlier. This
Comment does not suggest that facilities require patients to make more
than the required number of requests, but rather that facilities supply a
tool for physicians to review the patient’s eligibility if the requests are
spread over time. New Jersey’s Department of Health website currently
provides a follow-up form, but it is only to confirm that the physician
followed the Act’s requirements.
174
A facility or physician’s practice
should have its own form, similar to the final attestation form in
California,
175
that notes a patient’s mental health and physical capacity
at the time the final request is made and confirms that the physician
informed the patient of the facility’s ingestion recommendation and
procedures.
4. Implementing Reporting Requirements
In teaching New Jersey health care professionals about the Act and
how to implement it effectively, it is important to recognize that, like
many other statutes, New Jersey’s act has reporting requirements.
176
Even though reporting is already required, implementation efforts for
the above definitions should continually emphasize the importance of
accurate reporting. Accurate reporting in patient medical records could
prevent medical errors that could be irreversible in an aid in dying
case.
177
Physicians do not want to expose themselves to criminal
liability for following the Act but failing to report, just as they want to
173
N.J. STAT. ANN. § 26:16-10.
174
Medical Aid in Dying, N.J. DEP’T HEALTH, https://www.state.nj.us/health/advance
directive/maid/#3 (last visited Jan. 10, 2020).
175
See supra note 73 and accompanying text.
176
Span, supra note 88.
177
See generally Christina Farr, This Patient’s Medical Record Said She’d Given Birth
Twice – In Fact, She’d Never Been Pregnant, CNBC (last updated Dec. 9, 2018 8:25 PM),
https://www.cnbc.com/2018/12/09/medical-record-errors-common-hard-to-
fix.html (discussing the national issue with minor medical reporting errors, including
mistaken patient identity, leading to major problems).

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 871
avoid any medical reporting error that could put a lethal prescription in
the wrong hands.
178
B. Changes to the Act
1. Medication Administration
New Jersey should consider explicitly allowing self-injection as a
form of administration to increase access to the Act for people with
existing or developed physical disabilities who cannot self-administer
through ingesting a prepared regimen of aid in dying medication. To
complement this expansion of the Act to people with physical
disabilities, New Jersey also needs an exception to the rule that the
written request be executed solely by the patient. To further implement
these expansions, New Jersey might have to allow for a non-verbal form
of communication typical of the patient, so the patient could convey his
aid in dying wish without saying, “I would like aid in dying medication.”
This might be a loved one conveying the patient’s interest and the
patient showing or making a sound typical of that patient’s agreement
to confirm the desire to make the request.
179
This change, however,
would need close monitoring. While other states’ data has shown few
instances of coercion and abuse,
180
states have not allowed non-verbal
requests; thus, New Jersey would need to report how the request was
made to determine if non-verbal requests are correlated with higher
instances of coercion and abuse.
Even if New Jersey allows an injected form of self-administration,
it would still have safeguards and restrictions, such as age, residency,
and terminal illness requirements, which prevent access by certain
patients. Even if New Jersey extended past any other state to allow
physician administration, New Jersey would not follow international
trends. New Jersey does not allow for advance directives for aid in
dying, so the patient would be able to stop the treatment up until the
moment of administration.
178
For more examples of implementation techniques, see The N.J. Aid in Dying for the
Terminally Ill Implementation Toolkit, N.J. HOSP. ASS’N, http://www.njha.com/resources/
toolkits/the-nj-aid-in-dying-for-the-terminally-ill-implementation-toolkit (last visited
Feb. 14, 2020).
179
I recognize the slippery slope concerns about coercion and elder abuse, but data
from other states have not supported these arguments. If New Jersey follows similar
trends for patients who use the Act, the state can avoid these arguments and make
changes to its Act.
180
See sources cited supra notes 151–157.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
872 SETON HALL LAW REVIEW [Vol. 51:845
New Jersey could decrease potential use by further changing the
law by adjusting the “age” requirement to consider more than just an
individual’s stated age. New Jersey could require more than just an
arbitrary eighteen-year-old age requirement and look into the actual
brain development of the individual to determine that individual’s
mental capacity for making such a major, and permanent, health care
decision. This suggestion comes from recent developments in
neuroscience, showing that most people do not have fully developed
frontal lobes—the area of the brain used for decision-making—until
their mid-twenties.
181
This practical change to the law would include a
requirement, similar to the requirement for checking general mental
health capacity,
182
that a physician sends patients aged 18 to 25 to
mental health professionals. The mental health professional would
consider symptoms and brain scans of the patient’s frontal lobe, then
determine if the patient is capable of adult-like decision-making.
2. Minimum Time Between Requests
Like Oregon,
183
New Jersey could amend its law to include an
exception to the fifteen-day and forty-eight-hour waiting periods
between requests and prescriptions. While the current waiting period
is important for encouraging patients to consider their decisions and
consult family and mental health resources, it may be too arbitrary. New
Jersey should leave timing questions to the doctors who know whether
a patient may die painfully between requests or lose the ability to
complete the requests.
VI. CONCLUSION
This Comment compared definitions and use across the United
States and the world to raise some potential concerns for New Jersey
facilities and physicians as they continue to choose whether to
participate in New Jersey’s Medical Aid in Dying for the Terminally Ill
Act. This Comment identified trends that New Jersey might follow and
181
See NELL BERNSTEIN, BURNING DOWN THE HOUSE 207–09 (2014) (explaining recent
studies and their subsequent influence on understanding the risks of incarcerating
juvenile offenders in adult prisons); see also Neurolaw and Order, BBC NEWS (Dec. 6,
2017), https://www.bbc.co.uk/programmes/w3cswcll. for a recent argument in favor
of halting the execution of a man who committed murder at age nineteen but was tried
and sentenced to death before current developments in neuroimaging and studies of
adolescent brains, see Dr. Jason Chein, Insight: Adolescent Brain Immaturity Makes
Pending Execution Inappropriate, TEMPLE. UNIV. (Sept. 17, 2020 4:00 AM),
https://news.bloomberglaw.com/coronavirus/insight-adolescent-brain-immaturity-
makes-pending-execution-inappropriate.
182
N.J. STAT. ANN. § 26:16-8.
183
See OregonLive Politics Team, supra note 55.

NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
2021] COMMENT 873
potential concerns of those trends. This Comment recommended self-
administration training, utilization of residency experts, additional
public reporting, and use of final report forms where no time limit
between requests exists. Additionally, this Comment suggested New
Jersey amend its law to include both ingestion and injection
administration, a less arbitrary age requirement, and exceptions to
waiting periods. This Comment encourages New Jersey facilities to use
such recommendations and to be on alert to how future states and
countries create aid in dying laws and address these issues. New Jersey
should consider its data over the next several years to re-evaluate the
Act and consider whether making the above amendments would be
appropriate given those results.
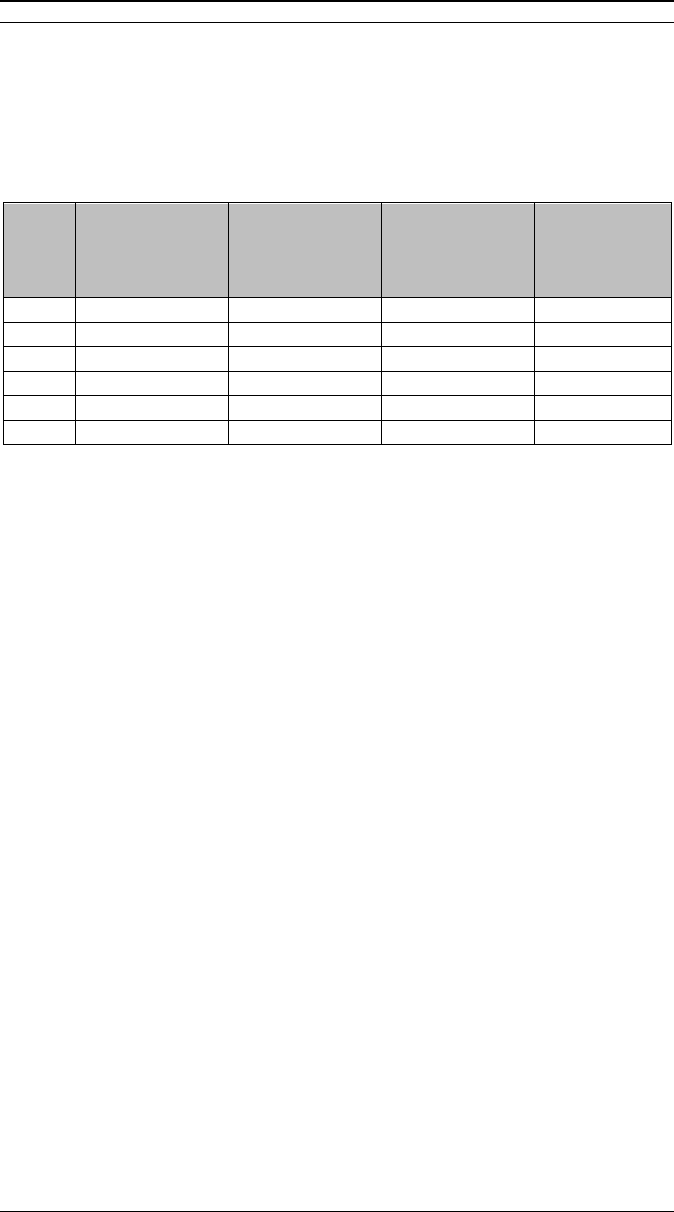
NIGRO (DO NOT DELETE) 1/7/2021 10:54 AM
874 SETON HALL LAW REVIEW [Vol. 51:845
APPENDIX
184
State
Prescriptions
Written in
2017 & 2018
Death by Aid
in Dying
Medication in
2017 & 2018
Total Census
Deaths
July 2017–
July 2018
% Total
Deaths by
Aid in Dying
Medication
OR
467
311
36,052
0.86%
CA
1029
711
280,674
0.25%
WA
479
367
57,568
0.25%
CO
197
174
38,367
0.45%
ME
14,079
NJ
76,730
184
This Table displays the numbers discussed in the text accompanying
notes 150–165.
